Mohamed
|Subscribers
Latest videos
A very simplified method giving information about cystic fibrosis
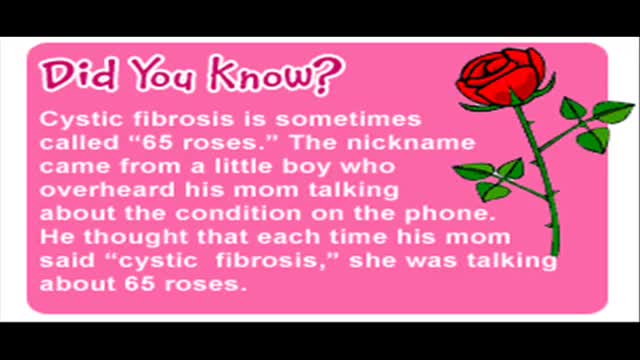
Cystic fibrosis is a disease passed down through families that causes thick, sticky mucus to build up in the lungs, digestive tract, and other areas of the body. It is one of the most common chronic lung diseases in children and young adults. It is a life-threatening disorder.
Amyotrophic lateral sclerosis The disorder causes muscle weakness and atrophy throughout the body caused by degeneration of the upper and lower motor neurons. Unable to function, the muscles weaken and atrophy. Affected individuals may ultimately lose the ability to initiate and control all voluntary movement, although bladder and bowel sphincters and the muscles responsible for eye movement are usually, but not always, spared. Cognitive function is generally spared for most patients although some (~5%) also have frontotemporal dementia.A higher proportion of patients (~30-50%) also have more subtle cognitive changes which may go unnoticed but are revealed by detailed neuropsychological testing. Sensory nerves and the autonomic nervous system, which controls functions like sweating, are generally unaffected but may be involved for some patients. The earliest symptoms of ALS are typically obvious weakness and/or muscle atrophy. Other presenting symptoms include muscle fasciculation (twitching), cramping, or stiffness of affected muscles; muscle weakness affecting an arm or a leg; and/or slurred and nasal speech. The parts of the body affected by early symptoms of ALS depend on which motor neurons in the body are damaged first. About 75% of people contracting the disease experience "limb onset" ALS i.e. first symptoms in the arms ("upper limb", not to be confused with "upper motor neuron") or legs ("lower limb", not to be confused with "lower motor neuron"). Patients with the leg onset form may experience awkwardness when walking or running or notice that they are tripping or stumbling, often with a "dropped foot" which drags along the ground. Arm-onset patients may experience difficulty with tasks requiring manual dexterity such as buttoning a shirt, writing, or turning a key in a lock. Occasionally, the symptoms remain confined to one limb for a long period of time or for the whole course of the illness; this is known as monomelic amyotrophy. About 25% of cases are "bulbar onset" ALS. These patients first notice difficulty speaking clearly or swallowing. Speech may become slurred, nasal in character, or quieter. Other symptoms include difficulty swallowing, and loss of tongue mobility. A smaller proportion of patients experience "respiratory onset" ALS where the intercostal muscles that support breathing are affected first. Regardless of the part of the body first affected by the disease, muscle weakness and atrophy spread to other parts of the body as the disease progresses. Patients experience increasing difficulty moving, swallowing (dysphagia), and speaking or forming words (dysarthria). Symptoms of upper motor neuron involvement include tight and stiff muscles (spasticity) and exaggerated reflexes (hyperreflexia) including an overactive gag reflex. An abnormal reflex commonly called Babinski's sign (the big toe extends upward and other toes spread out) also indicates upper motor neuron damage. Symptoms of lower motor neuron degeneration include muscle weakness and atrophy, muscle cramps, and fleeting twitches of muscles that can be seen under the skin (fasciculations). Around 15–45% of patients experience pseudobulbar affect, also known as "emotional lability", which consists of uncontrollable laughter, crying or smiling, attributable to degeneration of bulbar upper motor neurons resulting in exaggeration of motor expressions of emotion.
Most intact aortic aneurysms do not produce symptoms. As they enlarge, symptoms such as abdominal pain and back pain may develop. Compression of nerve roots may cause leg pain or numbness. Untreated, aneurysms tend to become progressively larger, although the rate of enlargement is unpredictable for any individual. Rarely, clotted blood which lines most aortic aneurysms can break off and result in an embolus. They may be found on physical examination. Medical imaging is necessary to confirm the diagnosis. Symptoms may include: anxiety or feeling of stress; nausea and vomiting; clammy skin; rapid heart rate. In patients presenting with aneurysm of the arch of the aorta, a common symptom is a hoarse voice as the left recurrent laryngeal nerve (a branch of the vagus nerve) is stretched. This is due to the recurrent laryngeal nerve winding around the arch of the aorta. If an aneurysm occurs in this location, the arch of the aorta will swell, hence stretching the left recurrent laryngeal nerve. The patient therefore has a hoarse voice as the recurrent laryngeal nerve allows function and sensation in the voicebox. Abdominal aortic aneurysms, hereafter referred to as AAAs, are the most common type of aortic aneurysm. One reason for this is that elastin, the principal load-bearing protein present in the wall of the aorta, is reduced in the abdominal aorta as compared to the thoracic aorta (nearer the heart). Another is that the abdominal aorta does not possess vasa vasorum, hindering repair. Most are true aneurysms that involve all three layers (tunica intima, tunica media and tunica adventitia), and are generally asymptomatic before rupture. The most common sign for the aortic aneuysm is the Erythema nodosum also known as leg lesions typically found near the ankle area. The prevalence of AAAs increases with age, with an average age of 65–70 at the time of diagnosis. AAAs have been attributed to atherosclerosis, though other factors are involved in their formation. An AAA may remain asymptomatic indefinitely. There is a large risk of rupture once the size has reached 5 cm, though some AAAs may swell to over 15 cm in diameter before rupturing. Before rupture, an AAA may present as a large, pulsatile mass above the umbilicus. A bruit may be heard from the turbulent flow in a severe atherosclerotic aneurysm or if thrombosis occurs. Unfortunately, however, rupture is usually the first hint of AAA. Once an aneurysm has ruptured, it presents with a classic pain-hypotension-mass triad. The pain is classically reported in the abdomen, back or flank. It is usually acute, severe and constant, and may radiate through the abdomen to the back. The diagnosis of an abdominal aortic aneurysm can be confirmed at the bedside by the use of ultrasound. Rupture could be indicated by the presence of free fluid in potential abdominal spaces, such as Morison's pouch, the splenorenal space (between the spleen and left kidney), subdiaphragmatic spaces (underneath the diaphragm) and peri-vesical spaces. A contrast-enhanced abdominal CT scan is needed for confirmation. Only 10–25% of patients survive rupture due to large pre- and post-operative mortality. Annual mortality from ruptured abdominal aneurysms in the United States alone is about 15,000. Another important complication of AAA is formation of a thrombus in the aneurysm.
Toxin is a protein produced by the bacterium Clostridium botulinum, and is extremely neurotoxic.
Neurotransmitter 3D Animation
on Tuesday, December 21, 2010
Neurotransmitters are endogenous chemicals which transmit signals from a neuron to a target cell across a synapse. Neurotransmitters are packaged into synaptic vesicles clustered beneath the membrane on the presynaptic side of a synapse, and are released into the synaptic cleft, where they bind to receptors in the membrane on the postsynaptic side of the synapse. Release of neurotransmitters usually follows arrival of an action potential at the synapse, but may also follow graded electrical potentials. Low level "baseline" release also occurs without electrical stimulation. Neurotransmitters are synthesized from plentiful and simple precursors, such as amino acids, which are readily available from the diet and which require only a small number of biosynthetic steps to convert. The chemical identity of neurotransmitters is often difficult to determine experimentally. For example, it is easy using an electron microscope to recognize vesicles on the presynaptic side of a synapse, but it may not be easy to determine directly what chemical is packed into them. The difficulties led to many historical controversies over whether a given chemical was or was not clearly established as a transmitter. In an effort to give some structure to the arguments, neurochemists worked out a set of experimentally tractable rules. According to the prevailing beliefs of the 1960s, a chemical can be classified as a neurotransmitter if it meets the following conditions: * There are precursors and/or synthesis enzymes located in the presynaptic side of the synapse. * The chemical is present in the presynaptic element. * It is available in sufficient quantity in the presynaptic neuron to affect the postsynaptic neuron; * There are postsynaptic receptors and the chemical is able to bind to them. * A biochemical mechanism for inactivation is present. There are many different ways to classify neurotransmitters. Dividing them into amino acids, peptides, and monoamines is sufficient for some classification purposes. Major neurotransmitters: * Amino acids: glutamate, aspartate, D-serine, γ-aminobutyric acid (GABA), glycine * Monoamines and other biogenic amines: dopamine (DA), norepinephrine (noradrenaline; NE, NA), epinephrine (adrenaline), histamine, serotonin (SE, 5-HT), melatonin * Others: acetylcholine (ACh), adenosine, anandamide, nitric oxide, etc. In addition, over 50 neuroactive peptides have been found, and new ones are discovered regularly. Many of these are "co-released" along with a small-molecule transmitter, but in some cases a peptide is the primary transmitter at a synapse. β-endorphin is a relatively well known example of a peptide neurotransmitter; it engages in highly specific interactions with opioid receptors in the central nervous system. Single ions, such as synaptically released zinc, are also considered neurotransmitters by some[by whom?], as are some gaseous molecules such as nitric oxide (NO) and carbon monoxide (CO). These are not classical neurotransmitters by the strictest definition, however, because although they have all been shown experimentally to be released by presynaptic terminals in an activity-dependent way, they are not packaged into vesicles. By far the most prevalent transmitter is glutamate, which is excitatory at well over 90% of the synapses in the human brain. The next most prevalent is GABA, which is inhibitory at more than 90% of the synapses that do not use glutamate. Even though other transmitters are used in far fewer synapses, they may be very important functionally—the great majority of psychoactive drugs exert their effects by altering the actions of some neurotransmitter systems, often acting through transmitters other than glutamate or GABA. Addictive drugs such as cocaine and amphetamine exert their effects primarily on the dop
A Bone scan or bone scintigraphy is a nuclear scanning test to find certain abnormalities in bone which are triggering the bone's attempts to heal. It is primarily used to help diagnose a number of conditions relating to bones, including: cancer of the bone or cancers that have spread (metastasized) to the bone, locating some sources of bone inflammation (e.g. bone pain such as lower back pain due to a fracture), the diagnosis of fractures that may not be visible in traditional X-ray images, and the detection of damage to bones due to certain infections and other problems.
Nuclear medicine bone scans are one of a number of methods of bone imaging, all of which are used to visually detect bone abnormalities. Such imaging studies include magnetic resonance imaging (MRI), X-ray computed tomography (CT) and in the case of 'bone scans' nuclear medicine. However, a nuclear bone scan is a functional test, which means it measures an aspect of bone metabolism, which most other imaging techniques cannot. The nuclear bone scan competes with the FDG-PET scan in seeing abnormal metabolism in bones, but it is considerably less expensive.
Nuclear bone scans are not to be confused with the completely different test often termed a "bone density scan," DEXA or DXA, which is a low exposure X-ray test measuring bone density to look for osteoporosis and other diseases where bones lose mass, without any bone re-building activity. The nuclear medicine scan technique is sensitive to areas of unusual bone re-building activity because the radiopharmaceutical is taken up by osteoblast cells which build bone. The technique therefore is sensitive to fractures and bone reaction to infections and bone tumors, including tumor metastases to bones, because all these pathologies trigger bone osteoblast activity. The bone scan is not sensitive to osteoporosis or multiple myeloma in bones, and therefore other techniques must be used to assess bone abnormalities from these diseases.
A breech birth is the birth of a baby from a breech presentation. In the breech presentation the baby enters the birth canal with the buttocks or feet first as opposed to the normal head first presentation.
There are either three or four main categories of breech births, depending upon the source:
* Frank breech - the baby's bottom comes first, and his or her legs are flexed at the hip and extended at the knees (with feet near the ears). 65-70% of breech babies are in the frank breech position.
* Complete breech - the baby's hips and knees are flexed so that the baby is sitting crosslegged, with feet beside the bottom.
* Footling breech - one or both feet come first, with the bottom at a higher position. This is rare at term but relatively common with premature fetuses.
* Kneeling breech - the baby is in a kneeling position, with one or both legs extended at the hips and flexed at the knees. This is extremely rare, and is excluded from many classifications.
As in labour with a baby in a normal head-down position, uterine contractions typically occur at regular intervals and gradually cause the cervix to become thinner and to open. In the more common breech presentations, the baby’s bottom (rather than feet or knees) is what is first to descend through the maternal pelvis and emerge from the vagina.
At the beginning of labour, the baby is generally in an oblique position, facing either the right or left side of the mother's back. As the baby's bottom is the same size in the term baby as the baby's head. Descent is thus as for the presenting fetal head and delay in descent is a cardinal sign of possible problems with the delivery of the head.
In order to begin the birth, internal rotation needs to occur. This happens when the mother's pelvic floor muscles cause the baby to turn so that it can be born with one hip directly in front of the other. At this point the baby is facing one of the mother's inner thighs. Then, the shoulders follow the same path as the hips did. At this time the baby usually turns to face the mother's back. Next occurs external rotation, which is when the shoulders emerge as the baby’s head enters the maternal pelvis. The combination of maternal muscle tone and uterine contractions cause the baby’s head to flex, chin to chest. Then the back of the baby's head emerges and finally the face.
Due to the increased pressure during labour and birth, it is normal for the baby's leading hip to be bruised and genitalia to be swollen. Babies who assumed the frank breech position in utero may continue to hold their legs in this position for some days after birth.
Breast reconstruction 3D Animation
on Friday, December 17, 2010
The primary part of the procedure can often be carried out immediately following the mastectomy. As with many other surgeries, patients with significant medical comorbidities (high blood pressure, obesity, diabetes) and smokers are higher-risk candidates. Surgeons may choose to perform delayed reconstruction to decrease this risk. Patients expected to receive external beam radiation as part of their adjuvant treatment are also commonly considered for delayed autologous reconstruction due to significantly higher complication rates with tissue expander-implant techniques in those patients. Breast reconstruction is a large undertaking that usually takes multiple operations. Sometimes these follow-up surgeries are spread out over weeks or months. If an implant is used, the individual runs the same risks and complications as those who use them for breast augmentation but has higher rates of capsular contracture (tightening or hardening of the scar tissue around the implant) and revisional surgeries. Outcomes based research on quality of life improvements and psychosocial benefits associated with breast reconstruction served as the stimulus in the United States for the 1998 Women's Health and Cancer Rights Act which mandated health care payer coverage for breast and nipple reconstruction, contralateral procedures to achieve symmetry, and treatment for the sequelae of mastectomy. This was followed in 2001 by additional legislation imposing penalties on noncompliant insurers. Similar provisions for coverage exist in most countries worldwide through national health care programs. There are many methods for breast reconstruction. The two most common are: * Tissue Expander - Breast implants This is the most common technique used in worldwide. The surgeon inserts a tissue expander, a temporary silastic implant, beneath a pocket under the pectoralis major muscle of the chest wall. The pectoral muscles may be released along its inferior edge to allow a larger, more supple pocket for the expander at the expense of thinner lower pole soft tissue coverage. The use of acellular human or animal dermal grafts have been described as an onlay patch to increase coverage of the implant when the pectoral muscle is released, which purports to improve both functional and aesthtic outcomes of implant-expander breast reconstruction. o In a process that can take weeks or months, saline solution is percutaneously injected to progressively expand the overlaying tissue. Once the expander has reached an acceptable size, it may be removed and replaced with a more permanent implant. Reconstruction of the areola and nipple are usually performed in a separate operation after the skin has stretched to its final size. * Flap reconstruction The second most common procedure uses tissue from other parts of the patient's body, such as the back, buttocks, thigh or abdomen. This procedure may be performed by leaving the donor tissue connected to the original site to retain its blood supply (the vessels are tunnelled beneath the skin surface to the new site) or it may be cut off and new blood supply may be connected. o The latissimus dorsi muscle flap is the donor tissue available on the back. It is a large flat muscle which can be employed without significant loss of function. It can be moved into the breast defect still attached to its blood supply under the arm pit (axilla). A latissimus flap is usually used to recruit soft-tissue coverage over an underlying implant. Enough volume can be recruited occasionally to reconstruct small breasts without an implant. o Abdominal flaps The abdominal flap for breast reconstruction is the TRAM flap or its technically distinct variants of microvascular "perforator flaps" like the DIEP/SIEP flaps. Both use the abdominal tissue between the umbilicus and the
Current treatment is a combination of pegylated interferon-alpha-2a or pegylated interferon-alpha-2b (brand names Pegasys or PEG-Intron) and the antiviral drug ribavirin for a period of 24 or 48 weeks, depending on hepatitis C virus genotype. In a large multicenter randomized control study among genotype 2 or 3 infected patients (NORDymanIC),[35] patients achieving HCV RNA below 1000 IU/mL by day 7 who were treated for 12 weeks demonstrated similar cure rates as those treated for 24 weeks.[36][37]
Pegylated interferon-alpha-2a plus ribavirin may increase sustained virological response among patients with chronic hepatitis C as compared to pegylated interferon-alpha-2b plus ribavirin according to a systematic review of randomized controlled trials .[38] The relative benefit increase was 14.6%. For patients at similar risk to those in this study (41.0% had sustained virological response when not treated with pegylated interferon alpha 2a plus ribavirin), this leads to an absolute benefit increase of 6%. About 16.7 patients must be treated for one to benefit (number needed to treat = 16.7; click here [39] to adjust these results for patients at higher or lower risk of sustained virological response). However, this study's results may be biased due to uncertain temporality of association, selective dose response.
Treatment is generally recommended for patients with proven hepatitis C virus infection and persistently abnormal liver function tests.
Treatment during the acute infection phase has much higher success rates (greater than 90%) with a shorter duration of treatment; however, this must be balanced against the 15-40% chance of spontaneous clearance without treatment (see Acute Hepatitis C section above).
Those with low initial viral loads respond much better to treatment than those with higher viral loads (greater than 400,000 IU/mL). Current combination therapy is usually supervised by physicians in the fields of gastroenterology, hepatology or infectious disease.
The treatment may be physically demanding, particularly for those with a prior history of drug or alcohol abuse. It can qualify for temporary disability in some cases. A substantial proportion of patients will experience a panoply of side effects ranging from a 'flu-like' syndrome (the most common, experienced for a few days after the weekly injection of interferon) to severe adverse events including anemia, cardiovascular events and psychiatric problems such as suicide or suicidal ideation. The latter are exacerbated by the general physiological stress experienced by the patient.
An animated illustration showing muscles of the forearm
Leopold's Maneuvers are difficult to perform on obese women and women who have hydramnios. The palpation can sometimes be uncomfortable for the woman if care is not taken to ensure she is relaxed and adequately positioned. To aid in this, the health care provider should first ensure that the woman has recently emptied her bladder. If she has not, she may need to have a straight urinary catheter inserted to empy it if she is unable to micturate herself. The woman should lie on her back with her shoulders raised slightly on a pillow and her knees drawn up a little. Her abdomen should be uncovered, and most women appreciate it if the individual performing the maneuver warms their hands prior to palpation. First maneuver: Fundal Grip While facing the woman, palpate the woman's upper abdomen with both hands. A professional can often determine the size, consistency, shape, and mobility of the form that is felt. The fetal head is hard, firm, round, and moves independently of the trunk while the buttocks feel softer, are symmetric, and the shoulders and limbs have small bony processes; unlike the head, they move with the trunk. Second maneuver After the upper abdomen has been palpated and the form that is found is identified, the individual performing the maneuver attempts to determine the location of the fetal back. Still facing the woman, the health care provider palpates the abdomen with gentle but also deep pressure using the palm of the hands. First the right hand remains steady on one side of the abdomen while the left hand explores the right side of the woman's uterus. This is then repeated using the opposite side and hands. The fetal back will feel firm and smooth while fetal extremities (arms, legs, etc.) should feel like small irregularities and protrusions. The fetal back, once determined, should connect with the form found in the upper abdomen and also a mass in the maternal inlet, lower abdomen. Third maneuver: Pawlick's Grip In the third maneuver the health care provider attempts to determine what fetal part is lying above the inlet, or lower abdomen.[2] The individual performing the maneuver first grasps the lower portion of the abdomen just above the symphysis pubis with the thumb and fingers of the right hand. This maneuver should yield the opposite information and validate the findings of the first maneuver. If the woman enters labor, this is the part which will most likely come first in a vaginal birth. If it is the head and is not actively engaged in the birthing process, it may be gently pushed back and forth. The Pawlick's Grip, although still used by some obstetricians, is not recommended as it is more uncomfortable for the woman. Instead, a two-handed approach is favored by placing the fingers of both hands laterally on either side of the presenting part. Fourth maneuver The last maneuver requires that the health care provider face the woman's feet, as he or she will attempt to locate the fetus' brow. The fingers of both hands are moved gently down the sides of the uterus toward the pubis. The side where there is resistance to the descent of the fingers toward the pubis is greatest is where the brow is located. If the head of the fetus is well-flexed, it should be on the opposite side from the fetal back. If the fetal head is extended though, the occiput is instead felt and is located on the same side as the back. Cautions Leopold's maneuvers are intended to be performed by health care professionals, as they have received the training and instruction in how to perform them. That said, as long as care taken not to roughly or excessively disturb the fetus, there is no real reason it cannot be performed at home as an informational exercise. It is important to note that all findings are not truly diagnostic, and as such ultrasound is required to conclusively determine the fetal position.
Left pleura rupture during laparoscopy
A video showing the examination of femoral hernia.
Repair of an indirect inguinal hernia
An endoscopy showing celiac disease
Pterygium excision and conjunctival autograft
Ovarian pregnancy: an unusual location of ectopic pregnancy
Knee Replacement Surgery Video
This is a very funny video from and episode of "House". you have to watch. It is hilarious