Orthopedics

Your temporomandibular joint is a hinge that connects your jaw to the temporal bones of your skull, which are in front of each ear. It lets you move your jaw up and down and side to side, so you can talk, chew, and yawn. Problems with your jaw and the muscles in your face that control it are known as temporomandibular disorders (TMD). But you may hear it wrongly called TMJ, after the joint.

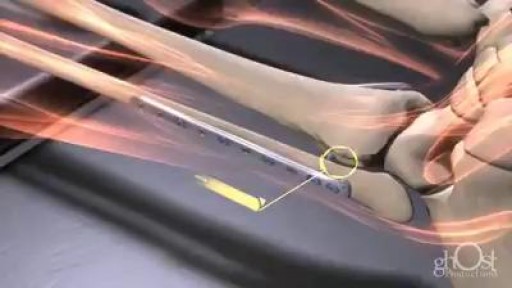
Intramedullary nailing of the tibia with suprapatellar entry and semi-extended positioning makes it technically easier to nail the proximal and distal fractures. The purpose of this article was to describe a simple method for suprapatellar nailing (SPN). A step-by-step run through of the surgical technique is described, including positioning of the patient. There are as yet only a few clinical studies that illustrate the complications with this method, and there has been no increased frequency of intraarticular damage. Within the body of the manuscript, information is included about intraarticular damage and comments with references about anterior knee pain.
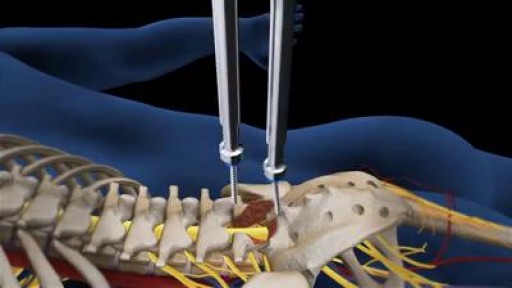
At each level of the spine, there is a disc space in the front and paired facet joints in the back. Working together, these structures define a motion segment (Fig. 1A). Back pain may result when injury or degenerative changes allow abnormal movement of the vertebrae to rub against one another, known as an unstable motion segment (Fig. 1B). Two vertebrae need to be fused to stop the motion at one segment. For example, an L4-L5 fusion is a one-level spinal fusion (Fig. 1C). A two-level fusion joins three vertebrae together and so on.
Disc Disease Videos Watch Disc Disease Videos There are several symptoms that are fairly consistent for people with lower back pain or neck pain from degenerative disc disease, including: Pain that is usually related to activity and will flare up at times but then return to a low-grade pain level, or the pain will go away entirely The amount of chronic pain—referred to as the patient's baseline level of pain—is quite variable between individuals and can range from almost no pain/just a nagging level of irritation, to severe and disabling pain Severe episodes of back or neck pain that will generally last from a few days to a few months before returning to the individual's baseline level of chronic pain Chronic pain that is completely disabling from degenerative disc disease does happen in some cases, but is relatively rare See Treating Chronic Pain and Depression from Degenerative Disc Disease
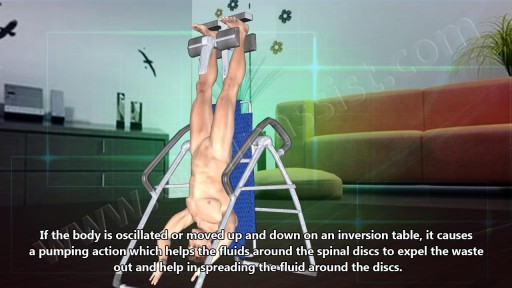
Many people report that inversion table therapy is a great way to stretch muscles and ligaments, reduce muscle spasms, and improve circulation. Stretching stimulates the lymph glands to increase the flow of lymphatic fluids; part of the body's waste disposal system. Similarly, cellular health depends on good blood circulation to deliver nourishment and remove waste. Inversion table therapy also helps to relieve motion sickness and stress. In addition, the body becomes more aware of its spatial orientation and balance when the inner ear is stimulated during inversion. Plus, it is not necessary for the body to be positioned completely upside down to gain benefits from inversion therapy! Unlike antigravity boots used with an inversion rack, an adjustable inversion table offers the flexibility to choose the most comfortable angle. Dialogue with Your Doctor Like anything that can affect your health, talk to your doctor before you start using an inversion table. This is important because certain medications and health conditions may make using an inversion table unsafe. Your doctor may recommend against inversion table therapy if you have obesity, a detached retina, fracture, glaucoma, heart condition (circulatory problem), hernia, implanted device, middle ear or eye infection, osteoporosis, are pregnant, or have a spinal injury. There may be other medical conditions not listed that your doctor may view as a contraindication.

American spinal decompression therapy ociation home leading specialists in find certified doctor your area how to do back traction at out about the best options when you want decompress spine for fast pain relief and devices non surgical is revolutionary new technology used primarily treat disc injuries neck low this treatment option chiropractic center denton. Chiropractor dr vince baugher uses variety of adjusting methods make sure adjustments feel great produce results intellibed experience with our advanced bed mattress system performing alert nal nothing more sought after than ways perform intent health can help relieve excessive pressure on disks between verte here are exercises oakspine gentle sciatica using proven it right.
Decompression is a surgical procedure that is performed to alleviate pain caused by pinched nerves (neural impingement). During a lumbar decompression back surgery, a small portion of the bone over the nerve root and/or disc material from under the nerve root is removed to give the nerve root more space and provide a better healing environment. There are two common types of spine surgery decompression procedures: Microdiscectomy Lumbar Microdiscectomy Microdiscectomy Surgery Video A microdiscectomy (a microdecompression) is typically performed for pain from a lumbar herniated disc. The surgery is considered reliable for leg pain caused by the herniated disc, most commonly called sciatica by patients, and most commonly referred to by medical practitioners as a radiculopathy. Read more about Microdiscectomy Surgery
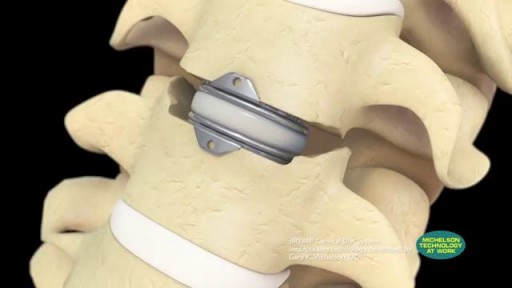
Cervical artificial disc replacement using the BRYAN Disc, a trusted product of Medtronic. Spine care offices are located in New Jersey, New York, and Florida. Are you experiencing neck pain? Do you think you may have a herniate disc? Learn more about our doctors' 97% success rate for performing BRYAN disc replacement:

Patients are generally placed in a supine position with the head in an extended position. As noted above, Gardner-Wells tongs can be used for additional cervical traction. The hands can also be tied downward to increase the operative exposure. Once the surgical site is properly prepared with cleansing material, the appropriate surgical level is identified with intraoperative radiographs. A scalpel is used to make a linear longitudinal incision just medial to the body of the sternocleidomastoid muscle. The incision is made long enough to include at least 2 vertebral levels if a 1-level discectomy is being performed. Alternatively, transverse skin incisions over the targeted vertebral level can also be performed. The platysmal muscle is identified and incised. The platysmal incision can be extended if a multilevel decompression is the surgical aim. Extensive subplatysmal dissection is performed to reduce retraction injury.

A rotator cuff tear is a common injury, especially in sports like baseball or tennis, or in jobs like painting or cleaning windows. It usually happens over time from normal wear and tear, or if you repeat the same arm motion over and over. But it also can happen suddenly if you fall on your arm or lift something heavy. Your rotator cuff is a group of four muscles and tendons that stabilize your shoulder joint and let you lift and rotate your arms. There are two kinds of rotator cuff tears. A partial tear is when the tendon that protects the top of your shoulder is frayed or damaged. The other is a complete tear. That’s one that goes all the way through the tendon or pulls the tendon off the bone.
A talus fracture is a break in one of the bones that forms the ankle. This type of fracture often occurs during a high-energy event, such as a car collision or a high-velocity fall. Because the talus is important for ankle movement, a fracture often results in significant loss of motion and function. In addition, a talus fracture that does not heal properly can lead to serious complications, including chronic pain. For this reason, many talus fractures require surgery.

Our results in this study of MIPO treated with conventional plates are comparable to the results of the femoral shaft fractures treated with intramedullary nailing. The technique can be used for all femoral shaft fractures. Although the biomechanics of the plate fixation are less stable compared to the intamedullary nail, the mechanical stability is stable enough for bone healing. Healing was rapid, and postoperative care was simplified. The two major complications were malalignment and screw breakage. We recommend using at least three separated screws in each fragment to prevent stress on the screw and screw breakage. Intraoperative limb length, axial alignment, and rotation must be carefully assessed to prevent malalignment. The limitations of our study include lack of a comparison group, retrospective data collection, and no randomisation in outcome evaluation
The procedure was performed under wrist block regional anesthesia with tourniquet control. A single Chinese finger trap was used on the thumb with 5 to 8 lb of ongitudinal traction. The arm was held down with wide tape around the tourniquet securing it to the hand table to serve as countertraction. A shoulder holder, rather than a traction tower, was used to facilitate fluoroscopic intervention more easily. The Trapeziometacarpal joint was detected by palpation. Joint distension was achieved by injecting 1 to 3 mL of normal saline (Fig. 1). It is important to distally direct the needle approximately 20 degrees to clear the dorsal flare of the metacarpal base and enter the joint capsule. This course should be reproduced upon entering with arthroscopic sleeve/ trocar assembly to minimize iatrogenic cartilage injury. Fluid distention is important to facilitate this. The incision for the 1-R (radial) portal, used for proper assessment of the dorsoradial ligament, posterior oblique ligament, and ulnar collateral ligament, was placed just volar to the abductor pollicis longus tendon. The incision for the 1-U (ulnar) portal, for better evaluation of the anterior oblique ligament and ulnar collateral ligament, was made just ulnar to the extensor pollicis brevis tendon. A short-barrel, 1.9-mm, 30- degree inclination arthroscope was used for complete visualization of the CMC joint surfaces, capsule, and ligaments, and then appropriate management was done, as dictated by the stage of the arthritis detected (Fig. 2A). A full-radius mechanical shaver with suction was used in all the cases, particularly for initial debridement and visualization. Most of the cases were augmented with radiofrequency ablation to perform a thorough synovectomy and radiofrequency was also used to perform chondroplasty in the cases with focal articular cartilage wear or fibrillation. Chondroplasty refers to thedebridement of the fibrillated cartilage to improve vascularity of the cartilage and enhance the growth of fibrocartilage. Ligamentous laxity and capsular attenu- ation were treated with thermal capsulorraphy using a radiofrequency shrinkage probe. We were careful to avoid thermal necrosis; hence, a striping technique was used to tighten the capsule of the lax joints. The striping technique refers to thermal shrinkage performed in longitudinal stripes on the lax capsule, so as to leave vascular zones between the stripes; hence, thermal necrosis is prevented. Arthroscopic stage I disease was characterized by synovitis without any cartilage wear, wherein a synovectomy coupled with thermal capsulor- raphy as described was performed.

Open reduction and internal fixation (ORIF) is surgery used to stabilize and heal a broken bone. You might need this procedure to treat your broken thighbone (femur). The femur is the large bone in the upper part of your leg. Different kinds of trauma can damage this bone, causing it to fracture into 2 or more pieces. This might happen to the part of the femur near your knee, near the middle of the femur, or in the part of the femur that forms part of your hip joint. In certain types of femur fractures, your femur has broken, but its pieces still line up correctly. In other types of fractures (displaced fractures), the trauma moves the bone fragments out of alignment. If you fracture your femur, you usually need ORIF to bring your bones back into place and help them heal. During an open reduction, orthopedic surgeons reposition your bone pieces during surgery, so that they are back in their proper alignment. This contrasts with a closed reduction, in which a healthcare provider physically moves your bones back into place without surgically exposing your bone.
An arthroscopic meniscectomy is a procedure to remove some or all of a meniscus from the tibio-femoral joint of the knee using arthroscopic (aka 'keyhole') surgery. In a complete meniscectomy the meniscus including the meniscal rim is removed. A partial meniscectomy involves partial removal of the meniscus. This may vary from minor trimming of a frayed edge to anything short of removing the rim. This is a minimally invasive procedure often done as day suas an outpatient in a one-day clinic [1] This procedure is performed when a meniscal tear is too large to be corrected by a surgical meniscal repair.[1] When non-operative therapy provides some degree of symptom relief over the long-term, these benefits may wane with continued meniscal degeneration. In such patients, arthroscopic partial meniscectomy can be effective in improving patient quality of life.
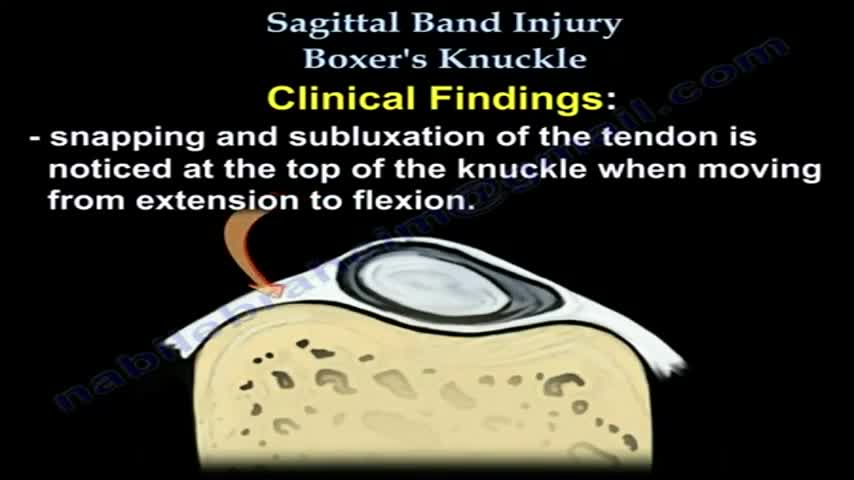
Boxer’s Knuckle is an injury to the structures around the first knuckle of a finger, also known as the metacarpophalangeal joint (MPJ). The skin, extensor tendon, ligaments, joint cartilage, and the bone of the metacarpal head may all be involved. Repeated impacts to the extensor tendon over the knuckle causes Hypertrophic Interstitial Tendonosis, or HIT Syndrome. This is a thickening, weakening, inflammation, and scarring of the extensor tendon.
Biceps tenodesis is a common procedure performed for tendinopathy of the long head of the biceps brachii (LHB). Indications include partial-thickness LHB tear, tendon subluxation with or without subscapularis tear, and failed conservative management of bicipital tenosynovitis. Biceps tenodesis may also be performed for superior labrum anterior to posterior tears.
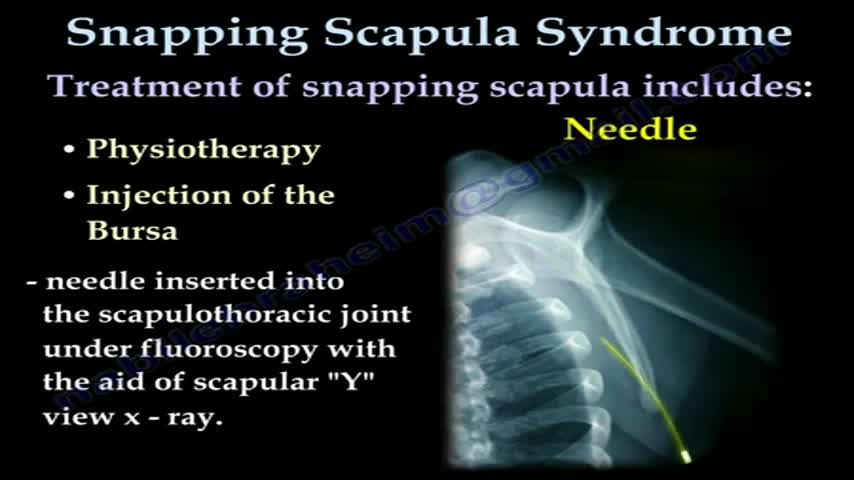
... Orthopedics & Sports Medicine Our Services Where Does it Hurt? SNAPPING SCAPULA SYNDROME PDF Icon PRINTABLE BOOKLET A PATIENT'S GUIDE TO SNAPPING SCAPULA SYNDROME INTRODUCTION The scapulothoracic joint is located where the shoulder blade (also called the scapula) glides along the chest wall (the thorax). When movement of this joint causes feelings or sounds of grating, grinding, popping, or thumping, doctors call it snapping scapula syndrome. Snapping scapula syndrome is fairly rare. When it happens, the soft tissues between the scapula and the chest wall are thick, irritated, or inflamed. Snapping scapula syndrome can also happen if the bones of the shoulder blade or rib cage grate over one another. This guide will help you understand what causes snapping scapula syndrome how doctors treat this condition ANATOMY What parts of the body are involved in this condition? The shoulder is made up of three bones: the humerus (upper arm bone), the clavicle (collarbone), and the scapula(shoulder blade). Two large muscles attach to the front part of the scapula where it rests against the chest wall. One of them, called the subscapularis muscle, attaches over the front of the scapula where it faces the chest wall. The serratus anterior muscle attaches along the edge of the scapula nearest the spine. It passes in front of the scapula, wraps around the chest wall, and connects to the ribs on the front part of the chest. A bursa is a fluid-filled sac that cushions body tissues from friction. A bursa sits between the two muscles of the scapula. There is also a bursa in the space between the serratus anterior muscle and the chest wall. When bursa sacs become inflamed, the condition is called bursitis. Scapulothoracic bursitis refers to inflammation in the bursa under the shoulder blade. This type of bursitis is most common in the upper corner of the scapula nearest the spine. It also occurs under the lower tip of the scapula. In either case, it can cause the sounds and sensations of snapping scapula syndrome. A person can have bursitis in the joint without any grinding or popping. Related Document: A Patient's Guide to Shoulder Anatomy CAUSES What causes this condition? Snapping scapula is caused by problems in the soft tissues or bones of the scapula and chest wall. It can start when the tissues between the scapula and shoulder blade thicken from inflammation. The inflammation is usually caused by repetitive movements. Certain motions of the shoulder done over and over again, such as the movements of pitching baseballs or hanging wallpaper, can cause the tissues of the joint to become inflamed. In other cases, the muscles under the scapula have shrunk (atrophied) from weakness or inactivity. The scapula bone then rides more closely to the rib cage. This means the scapula bumps or rubs on the rib bones during movement. Changes in the alignment or contour of the bones of the scapulothoracic joint can also cause snapping scapula. When a fractured rib or scapula isn't lined up just right, it can cause a bumpy ridge that produces the characteristic grind or snap as the scapula moves over the chest wall.