Orthopedics

Arthrocentesis involves both the puncture of a joint and the aspiration of its synovial fluid. It is typically used to make an accurate diagnosis of a painful, warm, swollen joint. Removal of excess fluid can be therapeutic. Analysis of the removed fluid helps to decipher its etiology. [1]
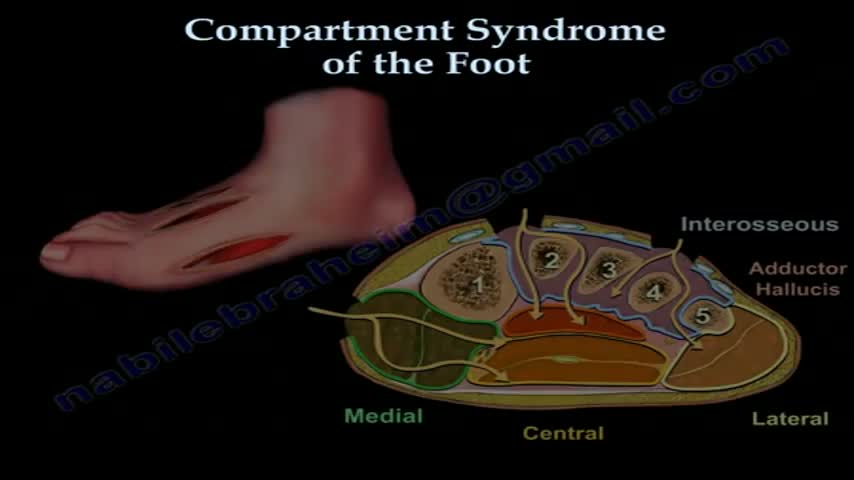
Compartment syndrome can develop in the foot following crush injury or closed fracture. Following some critical threshold of bleeding and/or swelling into the fixed space compartments, arterial pulse pressure is insufficient to overcome the osmotic tissue pressure gradient, leading to cell death. The complicating factor is related to the magnitude of the force of the crush injury. The amount of swelling or bleeding has to be sufficient to impair arterial inflow, while not being of sufficient magnitude to produce an open injury, which decompresses the pressure within the affected compartments. When the injury is open, we then attribute the late disability primarily to the crushing injury to the involved muscles.
Some of these advancements include the use of robots to perform the surgery and the use of computer mapping scanners and software and even 3D printers to make the artificial knee implant. We are also seeing a lot of different advances being made by the medical device manufacturers.Some of these changes are designed to make the devices more durable than the 10 to 20 years they are currently rated to last. This is important when younger patients who are years away from being considered elderly have a total knee replacement, they will typically need another artificial knee implanted at a later date since they are likely to outlive the implant, which doesn’t always happen with elderly patients.
A total knee replacement implant. The lower end of the femur. The metal femoral component curves around the end of the femur (thighbone). ... The top surface of the tibia. The tibial component is typically a flat metal platform with a cushion of strong, durable plastic, called polyethylene. ... The back surface of the patella.

Knee replacement surgery advances are improving patients' experiences and outcomes. Knee surgery -- or even partial knee replacement -- is often the solution for advanced knee arthritis. Today you can regain significant mobility and flexibility after knee replacement thanks to advances in orthopedic surgery technology, materials and techniques. Knee replacement recovery times also have improved. This knee replacement surgery video covers what you can expect out of these knee joint replacement advances. Knee replacement surgery has been around for more than 30 years and is an incredibly successful operation. In the past the past, when a person had bad arthritis of the knee, they were pretty much out of luck other than taking aspirin. They'd be debilitated and limited in their activities. So, when a person has pain, stiffness, and their life is becoming restricted by that, that's when it's time to consider knee replacement. We always do non-surgical treatment first. When that doesn't work anymore, then it's time to consider knee replacement. About 500,000 a year are done, and most patients who have gone through this basically say that they wish they had done it sooner.

The MAKOplasty® procedure is an FDA-cleared treatment option for patients who suffer from osteoarthritis damage in the medial (inner) portion of the knee. ... Only the diseased portion of your knee is removed, leaving the healthy bone and tissue surrounding it untouched.

If your knee is severely damaged by arthritis or injury, it may be hard for you to perform simple activities, such as walking or climbing stairs. You may even begin to feel pain while you are sitting or lying down. If nonsurgical treatments like medications and using walking supports are no longer helpful, you may want to consider total knee replacement surgery. Joint replacement surgery is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume normal activities. Knee replacement surgery was first performed in 1968. Since then, improvements in surgical materials and techniques have greatly increased its effectiveness. Total knee replacements are one of the most successful procedures in all of medicine. According to the Agency for Healthcare Research and Quality, more than 600,000 knee replacements are performed each year in the United States. Whether you have just begun exploring treatment options or have already decided to have total knee replacement surgery, this article will help you understand more about this valuable procedure.
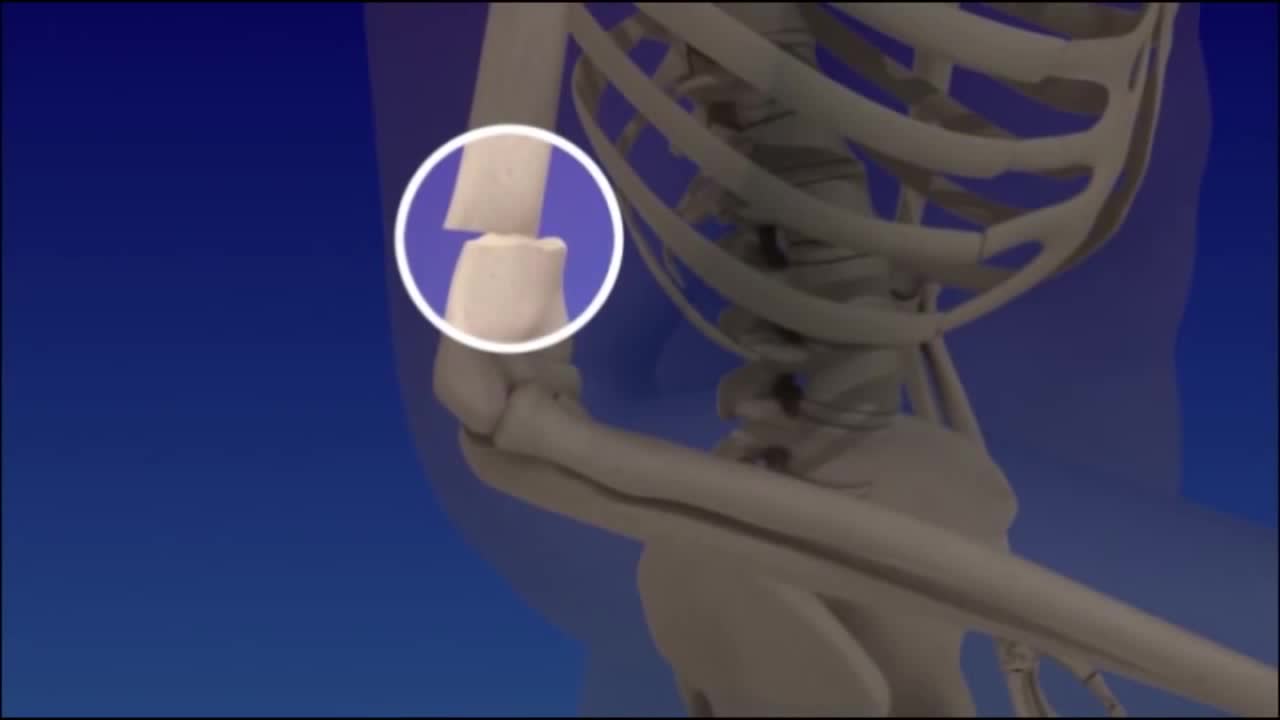
Distal Humerus Fractures of the Elbow. A distal humerus fracture is a break in the lower end of the upper arm bone (humerus), one of the three bones that come together to form the elbow joint. A fracture in this area can be very painful and make elbow motion difficult or impossible.

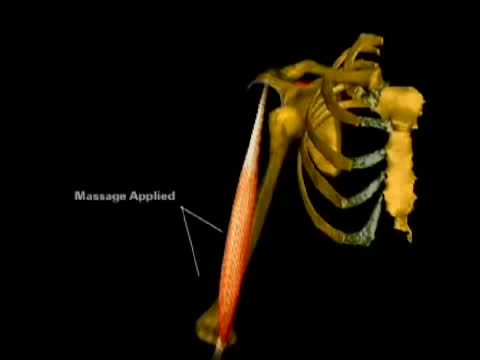
Reduction techniques can vary in terms of required force, time, equipment, and staff. [7] No single reduction method is successful in every instance; therefore, the clinician should be familiar with several reduction techniques. Techniques commonly used to reduce anterior shoulder dislocations include the following [35, 36, 37, 38, 39] : Stimson maneuver Scapular manipulation External rotation Milch technique Spaso technique Traction-countertraction
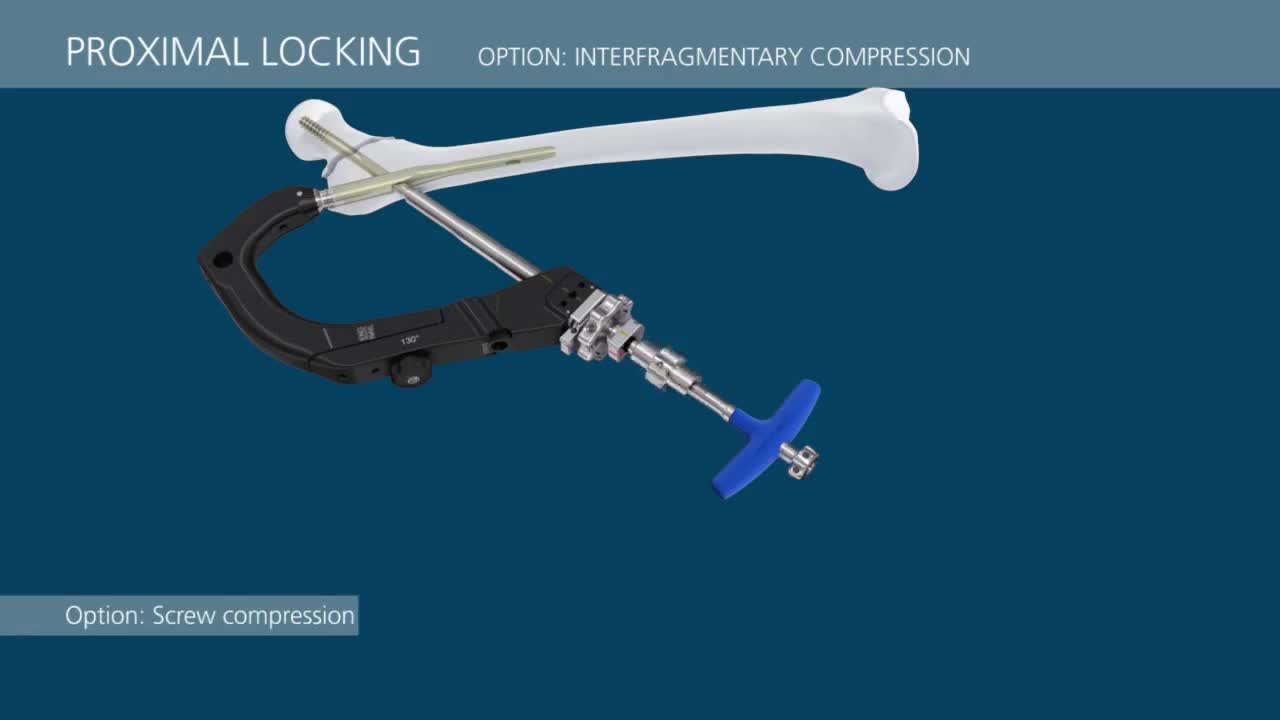
The Distal Femoral Osteotomy System utilizes the same principles of design featured in the Tibial Osteotomy System. Specifically designed femoral osteotomy plates take into account the anatomical differences between the distal femur and proximal tibia.

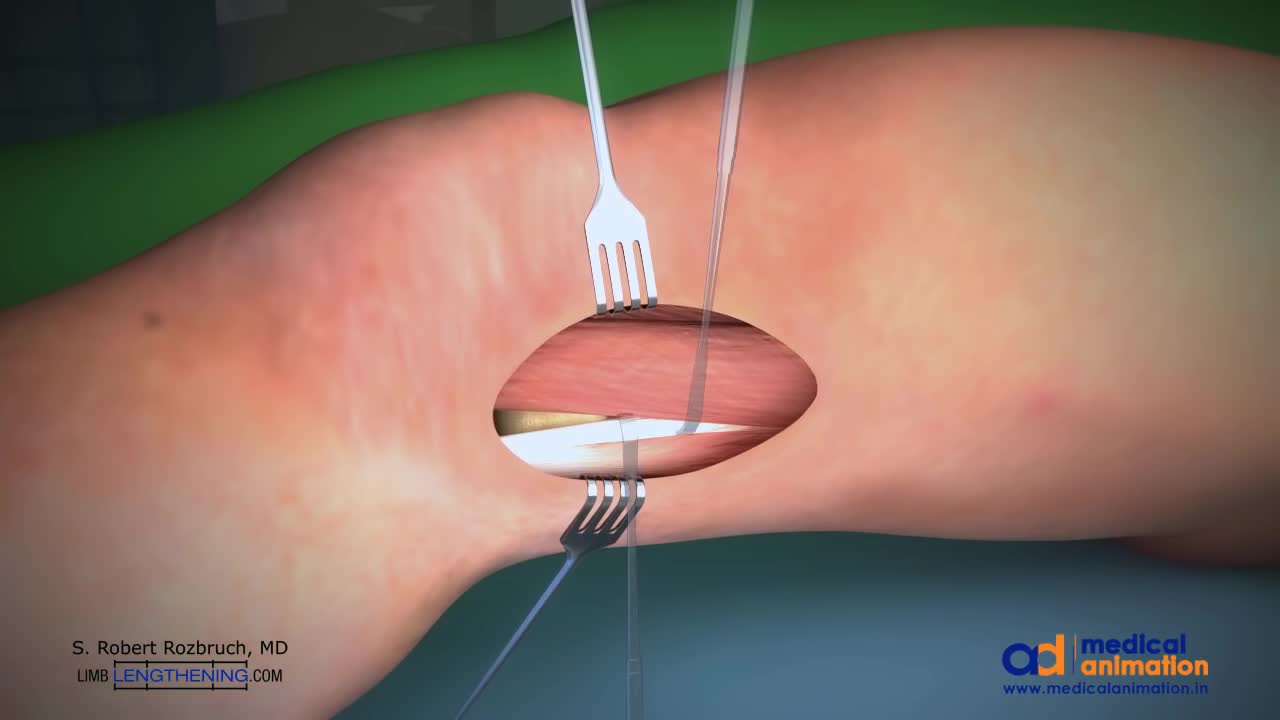
This is a technique of correcting knock knee (genu valgum) deformity by surgery. Highligh of the technique is that the bone is not cut, but merely weakened. The advantage is that it provides accuracy to the surgeon, and rapid healing. Once corrected, the bone is held in place with a special plate (Tomofix), which permits walking with crutches the very next day.