Orthopedics
Whether you have just begun exploring treatment options or have already decided to undergo hip replacement surgery, this information will help you understand the benefits and limitations of total hip replacement. This article describes how a normal hip works, the causes of hip pain, what to expect from hip replacement surgery, and what exercises and activities will help restore your mobility and strength, and enable you to return to everyday activities. If your hip has been damaged by arthritis, a fracture, or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff, and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting. If medications, changes in your everyday activities, and the use of walking supports do not adequately help your symptoms, you may consider hip replacement surgery. Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities. First performed in 1960, hip replacement surgery is one of the most successful operations in all of medicine. Since 1960, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of total hip replacement. According to the Agency for Healthcare Research and Quality, more than 300,000 total hip replacements are performed each year in the United States.
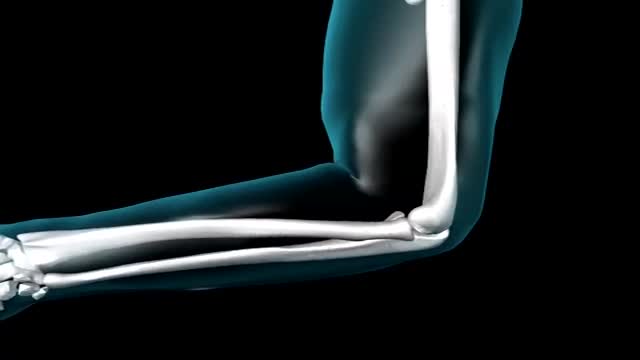
Elbow. In primates, including humans, the elbow joint is the synovial hinge joint between the humerus in the upper arm and the radius and ulna in the forearm which allows the hand to be moved towards and away from the body.
Recovery can take 4 to 6 months, depending on the size of the tear and other factors. You may have to wear a sling for 4 to 6 weeks after surgery. Pain is usually managed with medicines. Physical therapy can help you regain the motion and strength of your shoulder.
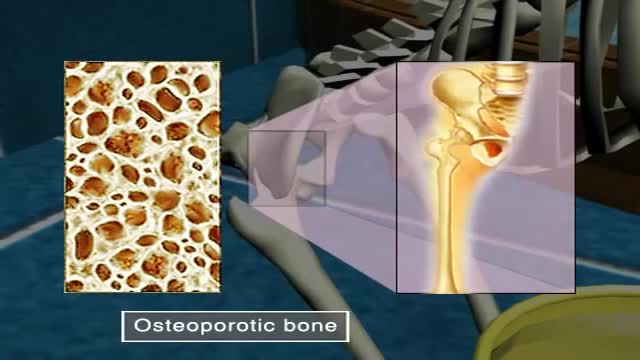
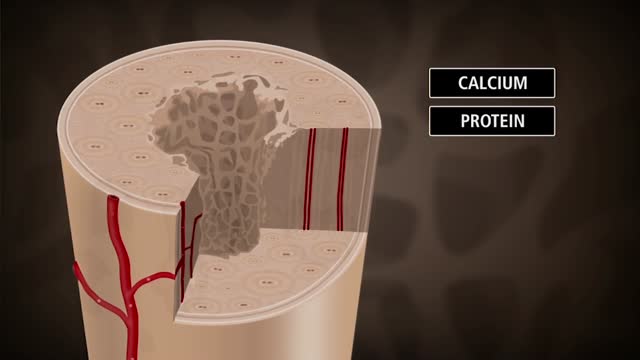
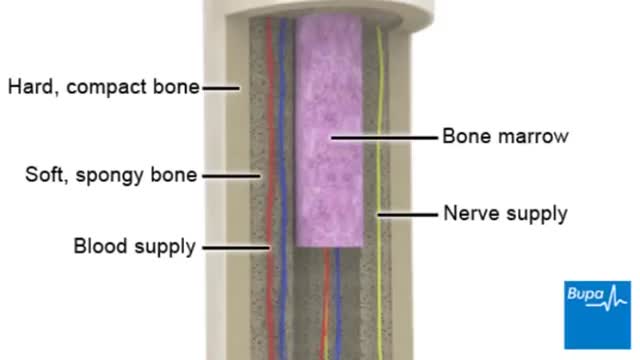
Osteoporosis, which literally means porous bone, is a disease in which the density and quality of bone are reduced. As bones become more porous and fragile, the risk of fracture is greatly increased. The loss of bone occurs silently and progressively. Often there are no symptoms until the first fracture occurs.
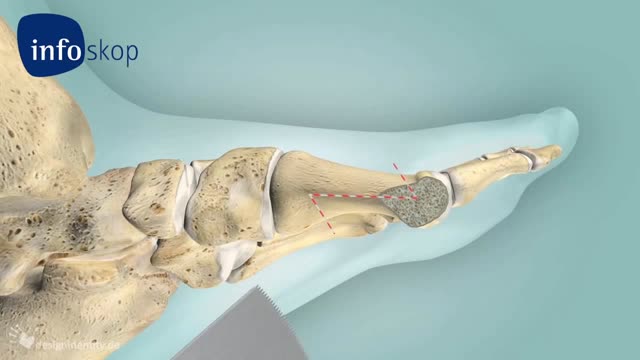
Knee osteotomy is commonly used to realign your knee structure if you have arthritic damage on only one side of your knee. The goal is to shift your body weight off the damaged area to the other side of your knee, where the cartilage is still healthy. When surgeons remove a wedge of your shinbone from underneath the healthy side of your knee, the shinbone and thighbone can bend away from the damaged cartilage. Imagine the hinges on a door. When the door is shut, the hinges are flush against the wall. As the door swings open, one side of the door remains pressed against the wall as space opens up on the other side. Removing just a small wedge of bone can "swing" your knee open, pressing the healthy tissue together as space opens up between the thighbone and shinbone on the damaged side so that the arthritic surfaces do not rub against each other. Osteotomy is also used as an alternative treatment to total knee replacement in younger and active patients. Because prosthetic knees may wear out over time, an osteotomy procedure can enable younger, active osteoarthritis patients to continue using the healthy portion of their knee. The procedure can delay the need for a total knee replacement for up to ten years.
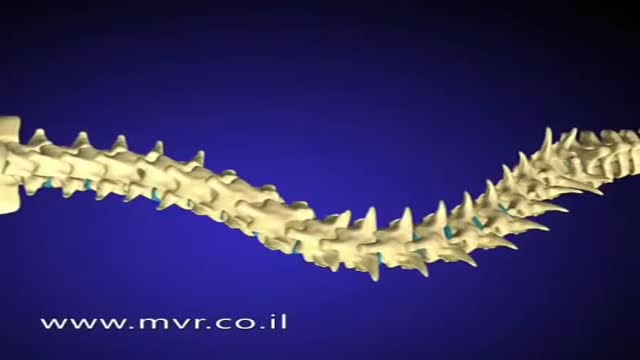
There are several approaches to scoliosis surgery, but all use modern instrumentation systems in which hooks and screws are applied to the spine to anchor long rods. The rods are then used to reduce and hold the spine while bone that is added fuses together with existing bone.
Knee replacement, also called arthroplasty, is a surgical procedure to resurface a knee damaged by arthritis. Metal and plastic parts are used to cap the ends of the bones that form the knee joint, along with the kneecap. This surgery may be considered for someone who has severe arthritis or a severe knee injury.
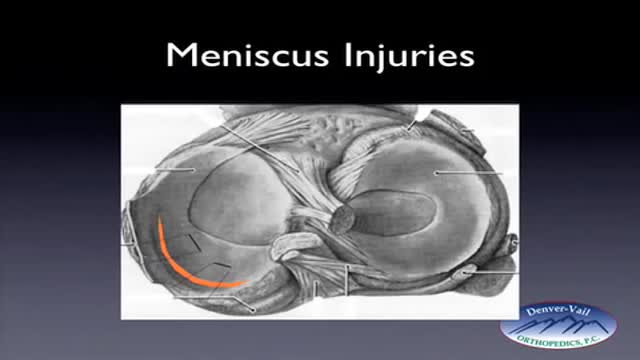
Rehabilitation time for a meniscus repair is about 3 months. A meniscectomy requires less time for healing — approximately 3 to 4 weeks. Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
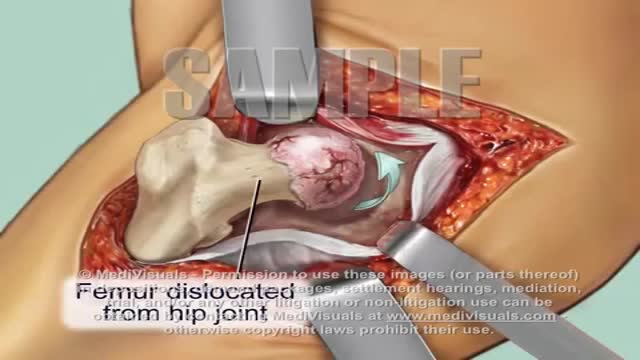
On September 28, 1940 at Columbia Hospital in Columbia, South Carolina, Dr. Austin T. Moore (1899–1963), an American surgeon, reported and performed the first metallic hip replacement surgery. In a total hip replacement (also called total hip arthroplasty), the damaged bone and cartilage is removed and replaced with prosthetic components. The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur.
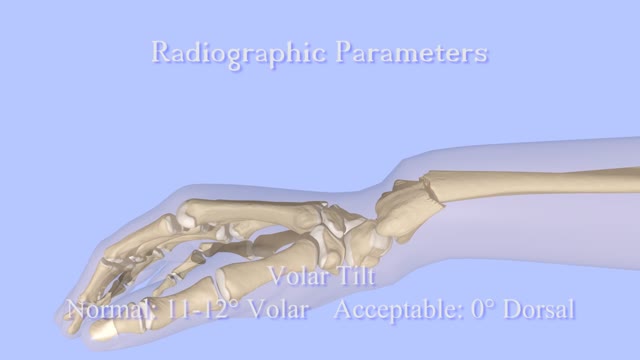
A distal radius fracture almost always occurs about 1 inch from the end of the bone. The break can occur in many different ways, however. One of the most common distal radius fractures is a Colles fracture, in which the broken fragment of the radius tilts upward. This fracture was first described in 1814 by an Irish surgeon and anatomist, Abraham Colles -- hence the name "Colles" fracture.
Closed Reduction of Distal Radius Fractures - Discussion: (distal radius fracture menu) - closed reduction & immobilization in plaster cast remains accepted method of treatment for majority of stable distal radius frx; - unstable fractures will often lose reduction in the cast and will slip back to the pre-reduction position; - patients should be examined for carpal tunnel symptoms before and after reduction; - carpal tunnel symptoms that do not resolve following reduction will require carpal tunnel release; - cautions: - The efficacy of closed reduction in displaced distal radius fractures. - Technique: - anesthesia: (see: anesthesia menu) - hematoma block w/ lidocaine; - w/ hematoma block surgeon should look for "flash back" of blood from hematoma, prior to injection; - references: - Regional anesthesia preferable for Colles' fracture. Controlled comparison with local anesthesia. - Neurological complications of dynamic reduction of Colles' fractures without anesthesia compared with traditional manipulation after local infiltration anesthesia. - methods of reduction: - Jones method: involves increasing deformity, applying traction, and immobilizing hand & wrist in reduced position; - placing hand & wrist in too much flexion (Cotton-Loder position) leads to median nerve compression & stiff fingers; - Bohler advocated longitudinal traction followed by extension and realignment; - consider hyper-extending the distal fragment, and then translating it distally (while in extended position) until it can be "hooked over" proximal fragment; - subsequently, the distal fragment can be flexed (or hinged) over the proximal shaft fragment; - closed reduction of distal radius fractures is facilitated by having an assistant provide counter traction (above the elbow) while the surgeon controls the distal fragment w/ both hands (both thumbs over the dorsal surface of the distal fragment); - flouroscopy: - it allows a quick, gentle, and complete reduction; - prepare are by prewrapping the arm w/ sheet cotton and have the plaster or fibroglass ready; - if flouroscopy is not available, then do not pre-wrap the extremity w/ cotton; - it will be necessary to palpate the landmarks (outer shaped of radius, radial styloid, and Lister's tubercle, in order to judge success of reduction; - casting: - generally, the surgeon will use a pre-measured double sugar sugar tong splint, which is 6-8 layers in thickness; - more than 8 layers of plaster can cause full thickness burns: - reference: Setting temperatures of synthetic casts. - position of immobilization - follow up: - radiographs: - repeat radiographs are required weekly for 2-3 weeks to ensure that there is maintenance of the reduction; - a fracture reduction that slips should be considered to be unstable and probably require fixation with (pins, or ex fix ect.) - there is some evidence that remanipulation following fracture displacement in cast is not effective for these fractures; - ultimately, whether or not a patient is satisfied with the results of non operative treatment depends heavily on th
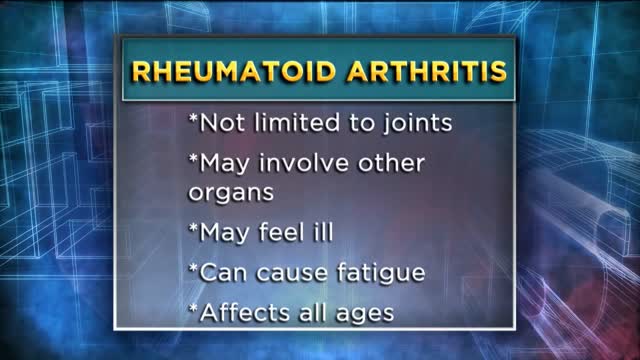
Arthritis is inflammation of one or more of your joints. The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. The most common types of arthritis are osteoarthritis and rheumatoid arthritis. Osteoarthritis causes cartilage — the hard, slippery tissue that covers the ends of bones where they form a joint — to break down. Rheumatoid arthritis is an autoimmune disorder that first targets the lining of joints (synovium). Uric acid crystals, infections or underlying disease, such as psoriasis or lupus, can cause other types of arthritis. Treatments vary depending on the type of arthritis. The main goals of arthritis treatments are to reduce symptoms and improve quality of life.
Bone is not a static part of the body — it's constantly being resorbed (broken down) and formed throughout your life. Your entire skeleton is replaced about every decade, according to the NIH. During your childhood and teenage years, bone formation occurs more quickly than bone resorption, resulting in growth. You reach your maximum bone density and strength around age 30, after which bone resorption slowly overtakes bone formation. Osteoporosis develops when there's an abnormal imbalance between bone resorption and formation — that is, resorption occurs too quickly, or formation too slowly.
Osteoporosis is a disease in which bones become brittle and fragile due to low bone mass and bone tissue loss. It's the most common type of bone disease, according to the National Institutes of Health (NIH), and increases your risk of fractures, particularly of the hips, spine, and wrists. Prevalence In the United States, nearly 54 million people ages 50 and older were living with osteoporosis or osteopenia (low bone mass ) in 2010, according to a 2014 article in the Journal of Bone and Mineral Research. More specifically, 10.2 million adults had osteoporosis, and 43.4 million adults had osteopenia, which puts a person at high risk for osteoporosis.
The ACL is one of the four main ligaments within the knee that connect the femur to the tibia. The knee is essentially a hinged joint that is held together by the medial collateral (MCL), lateral collateral (LCL), anterior cruciate (ACL) and posterior cruciate (PCL) ligaments.
The vertebrae are the bony building blocks of the spine. Between each of the largest parts (bodies) of the vertebrae are the discs. Ligaments are situated around the spine and discs. The spine has seven vertebrae in the neck (cervical vertebrae), 12 vertebrae in the mid-back (thoracic vertebrae), and five vertebrae in the low back (lumbar vertebrae). In addition, in the mid-buttock, beneath the fifth lumbar vertebra, is the sacrum, followed by the tailbone (coccyx).
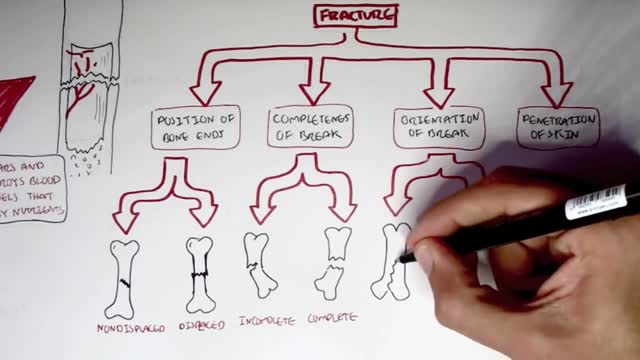
Common types of fractures include: Stable fracture. The broken ends of the bone line up and are barely out of place. Open, compound fracture. The skin may be pierced by the bone or by a blow that breaks the skin at the time of the fracture. ... Transverse fracture. ... Oblique fracture. ... Comminuted fracture.
Osteomyelitis is an infection in a bone. Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Infections can also begin in the bone itself if an injury exposes the bone to germs. In children, osteomyelitis most commonly affects the long bones of the legs and upper arms. Adults are more likely to develop osteomyelitis in the bones that make up the spine (vertebrae). People who have diabetes may develop osteomyelitis in their feet if they have foot ulcers. Once considered an incurable condition, osteomyelitis can be successfully treated today. Most people require surgery to remove parts of the bone that have died — followed by strong antibiotics, often delivered intravenously, typically for at least four to six weeks.
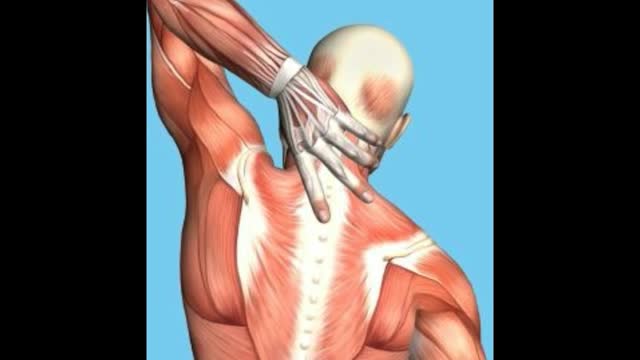
Rhomboid muscle strain and spasm causes upper back pain between the shoulder blades. Some patients describe the muscle spasms and discomfort as knots in the back. Early treatment is important to speed healing and recovery. Ice therapy for the first few days followed by moist heat can help relieve symptoms.Oct 12, 2015
This video: Rhomboid muscle strain and spasm causes upper back pain between the shoulder blades. Some patients describe the muscle spasms and discomfort as knots in the back. Early treatment is important to speed healing and recovery. Ice therapy for the first few days followed by moist heat can help relieve symptoms.Oct 12, 2015