Orthopedics
A broken bone requires emergency medical care. Your child might have a broken (fractured) bone if he or she heard or felt a bone snap, has difficulty moving the injured part, or if the injured part moves in an unnatural way or is very painful to the touch. A sprain occurs when the ligaments, which hold bones together, are overstretched and partially torn. A strain is when a muscle or tendon is overstretched or torn. Sprains and strains generally cause swelling and pain, and there may be bruises around the injured area. Most sprains and strains, after proper medical evaluation, can be treated at home.
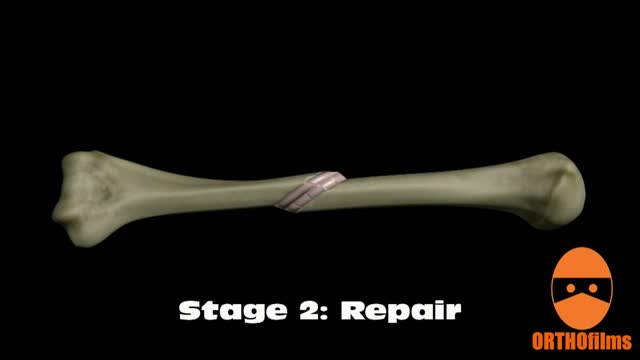
Bone healing can be divided into four stages: inflammation; soft callus formation; hard callus formation; remodeling.
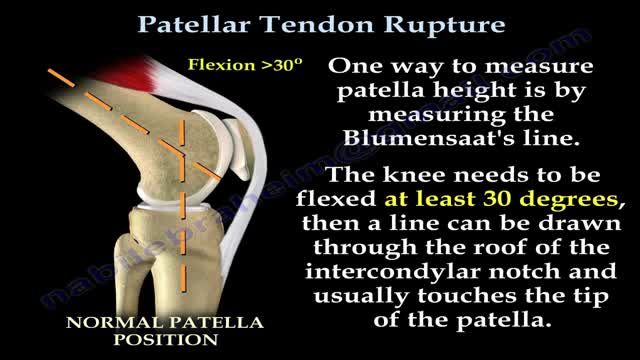
Patellar tendon rupture is a rupture of the tendon that connects the patella to the tibia. The superior portion of the patellar tendon attaches on the posterior portion of the patella, and the posterior portion of the patella tendon attaches to the tibial tubercle on the front of the tibia.
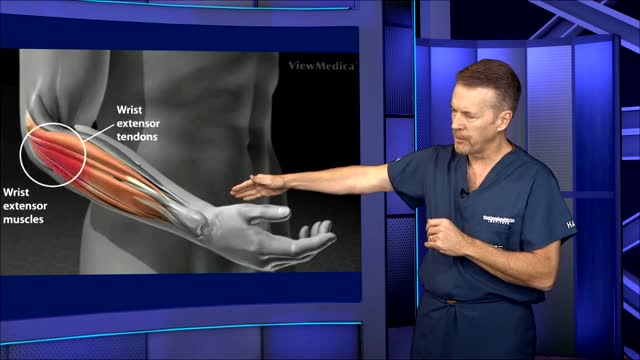
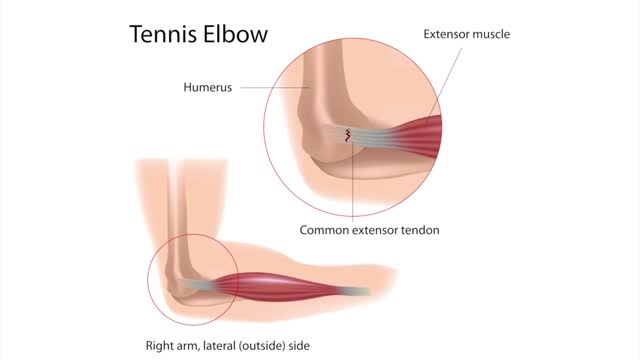
This video: Tennis elbow or lateral epicondylitis is a condition in which the outer part of the elbow becomes sore and tender. The forearm muscles and tendons become damaged from overuse — repeating the same strenuous motions again and again.
Tennis elbow or lateral epicondylitis is a condition in which the outer part of the elbow becomes sore and tender. The forearm muscles and tendons become damaged from overuse — repeating the same strenuous motions again and again.
Golfer's elbow causes pain that starts on the inside bump of the elbow, the medial epicondyle. Wrist flexors are the muscles of the forearm that pull the hand forward. The wrist flexors are on the palm side of the forearm. Most of the wrist flexors attach to one main tendon on the medial epicondyle.
Tendons are thick cords that join your muscles to your bones. When these tendons become irritated or inflamed, it is called tendinitis. This condition causes acute pain and tenderness, making it difficult to move the affected joint. Read more
Sciatica is often characterized by one or more of the following symptoms: Constant pain in only one side of the buttock or leg (rarely in both legs) Pain that is worse when sitting Leg pain that is often described as burning, tingling, or searing (versus a dull ache) Weakness, numbness, or difficulty moving the leg, foot, and/or toes A sharp pain that may make it difficult to stand up or walk Pain that radiates down the leg and possibly into the foot and toes (it rarely occurs only in the foot) Sciatica Causes and Treatments Video Watch: Sciatica Causes and Treatments Video Sciatic pain can vary from infrequent and irritating to constant and incapacitating. Symptoms are usually based on the location of the pinched nerve. While symptoms can be painful and potentially debilitating, it is rare that permanent sciatic nerve damage (tissue damage) will result, and spinal cord involvement is possible but rare.
Shoulder impingement syndrome, also called subacromial impingement, painful arc syndrome, supraspinatus syndrome, swimmer's shoulder, and thrower's shoulder, is a clinical syndrome which occurs when the tendons of the rotator cuff muscles become irritated and inflamed as they pass through the subacromial space ...
Treatment may include: Rest. Ice or heat. Nonsteroidal anti-inflammatory medications. Strengthening exercises. Ultrasound therapy. Corticosteroid injection. Surgery (for severe injuries)
A torn meniscus is one of the most common knee injuries. Any activity that causes you to forcefully twist or rotate your knee, especially when putting your full weight on it, can lead to a torn meniscus. Each of your knees has two menisci — C-shaped pieces of cartilage that act like a cushion between your shinbone and your thighbone. A torn meniscus causes pain, swelling and stiffness. You also might feel a block to knee motion and have trouble extending your knee fully. Conservative treatment — such as rest, ice and medication — is sometimes enough to relieve the pain of a torn meniscus and give the injury time to heal on its own. In other cases, however, a torn meniscus requires surgical repair.
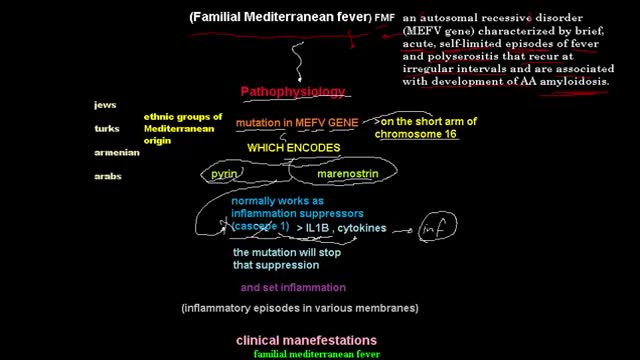
Familial Mediterranean fever is an inflammatory disorder that causes recurrent fevers and painful inflammation of your abdomen, lungs and joints. Familial Mediterranean fever is an inherited disorder that usually occurs in people of Mediterranean origin — including Sephardic Jews, Arabs, Greeks, Italians, Armenians and Turks. But it may affect any ethnic group. Familial Mediterranean fever is typically diagnosed during childhood. While there's no cure for this disorder, you may be able to relieve signs and symptoms of familial Mediterranean fever — or even prevent them altogether — by sticking to your treatment plan.
Rotationplasty is a type of autograft wherein a portion of a limb is removed, while the remaining limb below the involved portion is rotated and reattached. This procedure is used when a portion of an extremity is injured or involved with a disease, such as cancer. Typically, the ankle joint becomes the knee joint.
Most frozen shoulders get better on their own within 12 to 18 months. For persistent symptoms, your doctor may suggest: Steroid injections. Injecting corticosteroids into your shoulder joint may help decrease pain and improve shoulder mobility, especially in the early stages of the process. Joint distension. Injecting sterile water into the joint capsule can help stretch the tissue and make it easier to move the joint. Shoulder manipulation. In this procedure, you receive a general anesthetic, so you'll be unconscious and feel no pain. Then the doctor moves your shoulder joint in different directions, to help loosen the tightened tissue. Surgery. Surgery for frozen shoulder is rare, but if nothing else has helped, your doctor may recommend surgery to remove scar tissue and adhesions from inside your shoulder joint. Doctors usually perform this surgery with lighted, tubular instruments inserted through small incisions around your joint (arthroscopically).
Knee pain facts Knee pain is a common problem with many causes, from acute injuries to complications of medical conditions. Knee pain can be localized to a specific area of the knee or be diffuse throughout the knee. Knee pain is often accompanied by physical restriction. A thorough physical examination will usually establish the diagnosis of knee pain. The treatment of knee pain depends on the underlying cause. The prognosis of knee pain is usually good although it might require surgery or other interventions.
Psoriatic arthritis is a chronic arthritis. In some people, it is mild, with just occasional flare ups. In other people, it is continuous and can cause joint damage if it is not treated. Early diagnosis is important to avoid damage to joints. Psoriatic arthritis typically occurs in people with skin psoriasis, but it can occur in people without skin psoriasis, particularly in those who have relatives with psoriasis. Psoriatic arthritis typically affects the large joints, especially those of the lower extremities, distal joints of the fingers and toes, and also can affect the back and sacroiliac joints of the pelvis. For most people, appropriate treatments will relieve pain, protect the joints, and maintain mobility. Physical activity helps maintain joint movement. Psoriatic arthritis is sometimes misdiagnosed as gout, rheumatoid arthritis or osteoarthritis. - See more at: http://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Psoriatic-Arthritis#sthash.VsBTUw76.dpuf
Reactive arthritis can affect the heels, toes, fingers, low back, and joints, especially of the knees or ankles. Though it often goes away on its own, reactive arthritis can be prolonged and severe enough to require seeing a specialist. Effective treatment is available for reactive arthritis. Reactive arthritis tends to occur most often in men between ages 20 and 50. Most cases of reactive arthritis appear as a short episode. Occasionally, it becomes chronic. Reactive arthritis is a painful form of inflammatory arthritis (joint disease due to inflammation). It occurs in reaction to an infection by certain bacteria. Most often, these bacteria are in the genitals (Chlamydia trachomatis) or the bowel (Campylobacter, Salmonella, Shigella and Yersinia). Chlamydia most often transmits by sex. It often has no symptoms, but can cause a pus-like or watery discharge from the genitals. The bowel bacteria can cause diarrhea. If you develop arthritis within one month of diarrhea or a genital infection – especially with a discharge – see a health care provider. You may have reactive arthritis. - See more at: http://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Reactive-Arthritis#sthash.VNgDSOOY.dpuf
Ankylosing spondylitis is an inflammatory disease that, over time, can cause some of the vertebrae in your spine to fuse. This fusing makes the spine less flexible and can result in a hunched-forward posture. If ribs are affected, it can be difficult to breathe deeply. Ankylosing spondylitis affects men more often than women. Signs and symptoms typically begin in early adulthood. Inflammation also can occur in other parts of your body — most commonly, your eyes. There is no cure for ankylosing spondylitis, but treatments can lessen your symptoms and possibly slow progression of the disease.
The temporomandibular joint (TMJ), located just in front of the lower part of the ear, allows the lower jaw to move. The TMJ is a ball-and-socket joint, just like the hip or shoulder. When the mouth opens wide, the ball (called the condyle) comes out of the socket and moves forward, going back into place when the mouth closes. TMJ becomes dislocated when the condyle moves too far and gets stuck in front of a bony prominence called the articular eminence. The condyle can't move back into place. This happens most often when the ligaments that normally keep the condyle in place are somewhat loose, allowing the condyle to move beyond the articular eminence. The surrounding muscles often go into spasm and hold the condyle in the dislocated position.
The shoulder and arm receives its nerve supply through the brachial plexus. The brachial plexus is a complex network of nerves which come out of the neck, passes down to the front of the shoulder and then splits into many separate nerves to travel to different muscles and parts of the skin. Normally an arm movement is produced by initially thinking of the movement, then a message passes from the brain, down through the spinal cord to the appropriate nerve. Then the instruction to move is conveyed along the nerve to the specific arm muscle which then contracts and moves the arm.