Surgery Videos
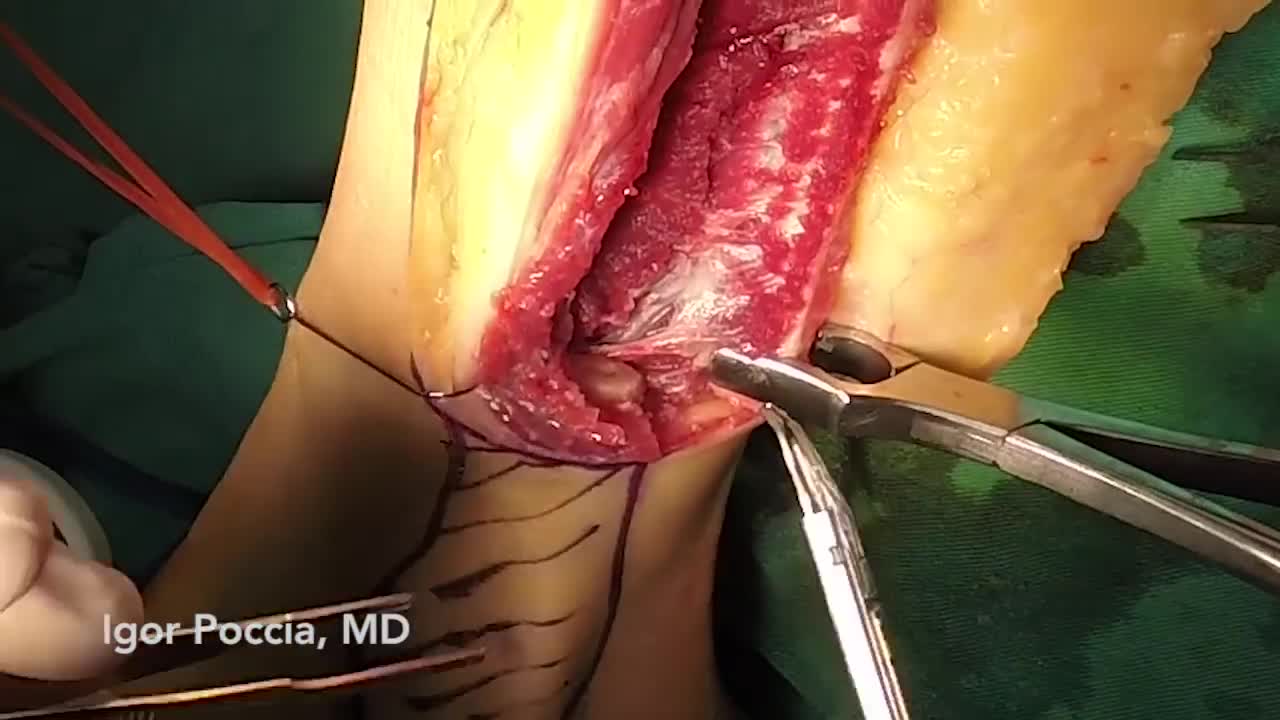
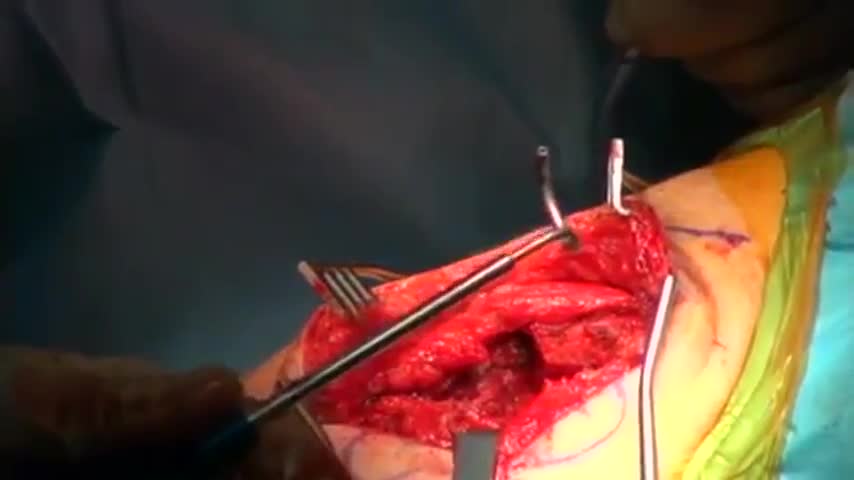
Both lower extremities must be evaluated to determine the presence or extent of any disease and to ascertain the pulse status of the patient. The feet are examined for signs of peripheral vascular disease and the anterior and posterior tibial pulses are palpated. Because an intact arch can supply retrograde flow to the major vessels of the foot, it can be helpful to put pressure on the anterior tibial artery when detecting the presence of a posterior tibial pulse and visa-versa. This "modified Allen's test" may detect proximal vessel obstruction masked by an intact foot arch. The need for preoperative angiography in young, healthy patients with a normal physical examination has been hotly debated. Our tendency has been to obtain preoperative angiograms as a guide. Although rare, we have seen lower extremities with a dominant peroneal artery nourishing the foot and distal anterior and posterior vessels, contraindicating sacrifice of the peroneal artery. MRI or CT angiography can also be used in many circumstances.
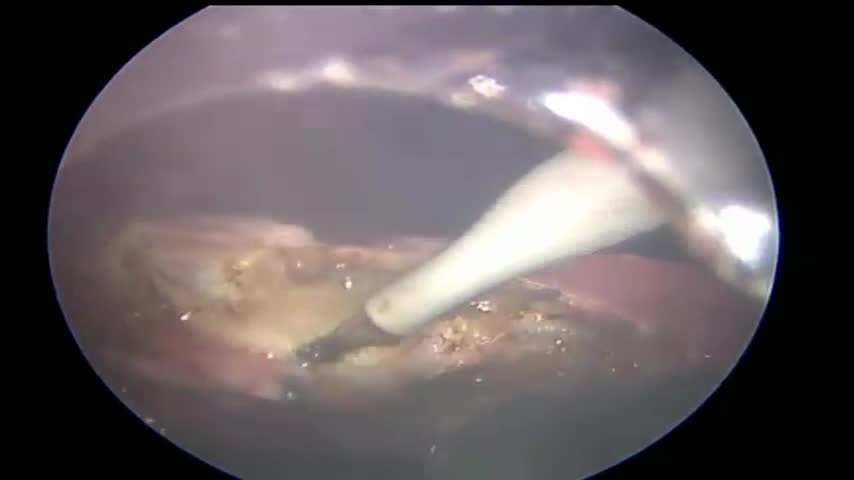
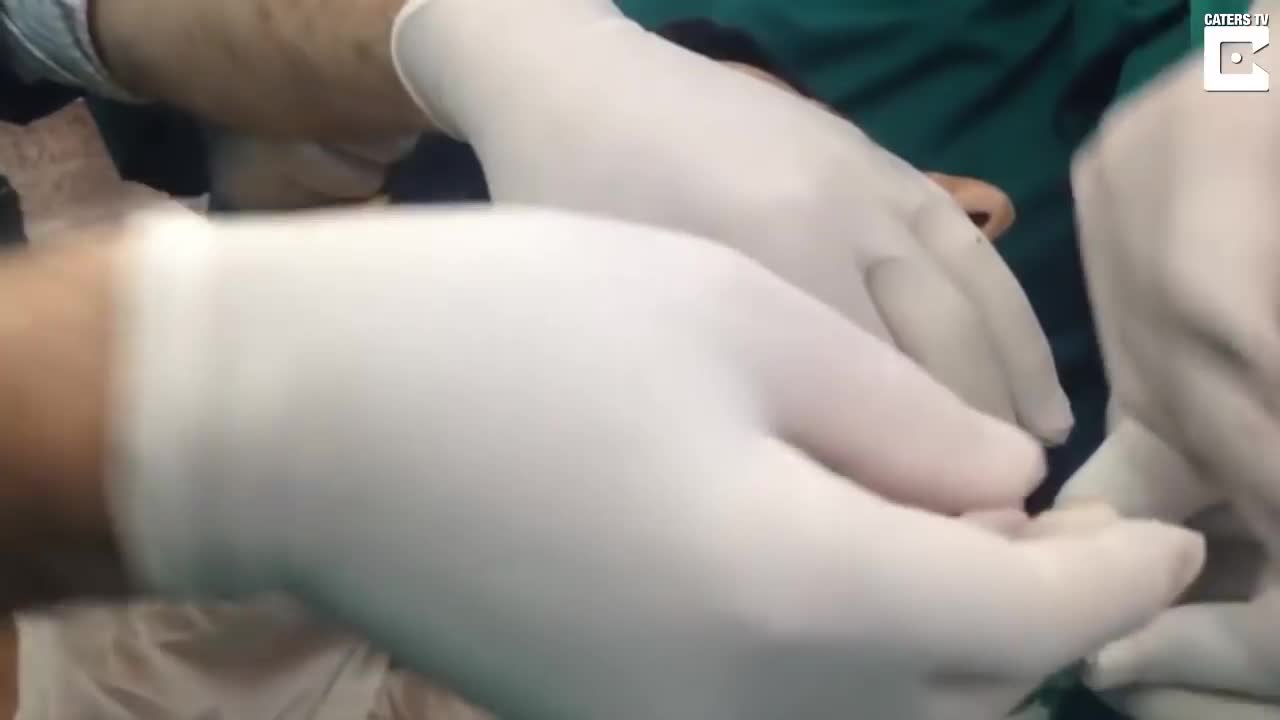
Simple microinstruments and a medical school laboratory microscope were used for anastomosis training. Chicken blood vessels were used as a material for this study. A long segment of blood vessel from the proximal brachial artery to the distal radial artery was used for training. End-to-side anastomosis was practiced first, and the training continued with end-to-end anastomosis of the appropriate segments.
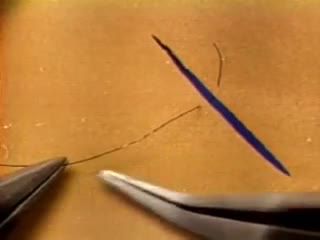
The needle should pass through the tissue at a perpendiculaPlace the tips of the left-hand forceps on the underside of the tissue at the point where the needle will enter, and gently push the edge upward. With the right hand, bring the needle into contact with the tissue, and press downward. These movements create eversion. Pass the needle through. Do not grab the tissue with your left hand forceps since it will damage the intima. If needed, you can pick up adventitia or a nearby suture to help with exposure and eversion. r.The needle must pass through the other side at a perpendicular, too. Bring the tip of the needle to the place where you intend to bring it out on the other side. Put the tip of your left-hand forceps on the upper surface of the tissue at the intended exit point. Press down with the left-hand forceps and push up with the needle to give you the correct eversion. The width of the bite should be about three times the thickness of the needle. The bites on both sides must be equal, and the needle should cross exactly in a straight line (not diagonally). Pull the needle through the tissue following the curve of the needle

At first, grasping the needle is difficult because it will have a tendency to want to jump around. What can oftentimes help is to get hold of the thread with the left-hand forceps at a point 2 to 3 cm away from the needle. Dangle the needle until it just comes to rest on the surface. This will then allow you to use the angulated needle holder to grab the needle easily. Your needle is in a stable position if it is set up to 90 degrees to the axis of the tips of the forceps. You can make minor corrections by touching the needle with your left-hand forceps, or by partially relaxing your grip and nudging the needle tip against another firm object. You should hold the needle just behind its midpoint (If you hold it too near the tip, it will point downward. If you hold it too near the thread end, it will point upward.).
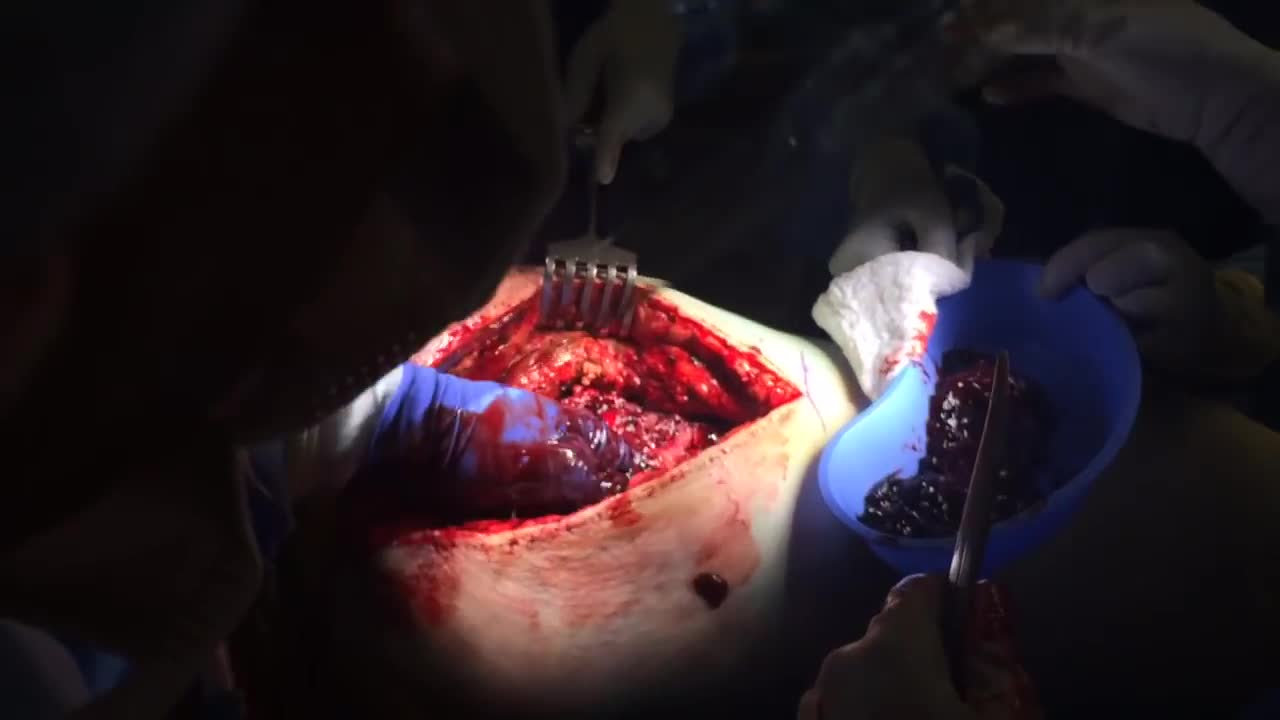
A hematoma is a common complication of surgical procedures. A large, expanding hematoma can result in necrosis of the overlying skin (1,2) or adjacent subcutaneous fat, increased incidence of infection, scarring, skin hyperpigmentation, tissue edema and a prolonged convalescence.