Surgery Videos
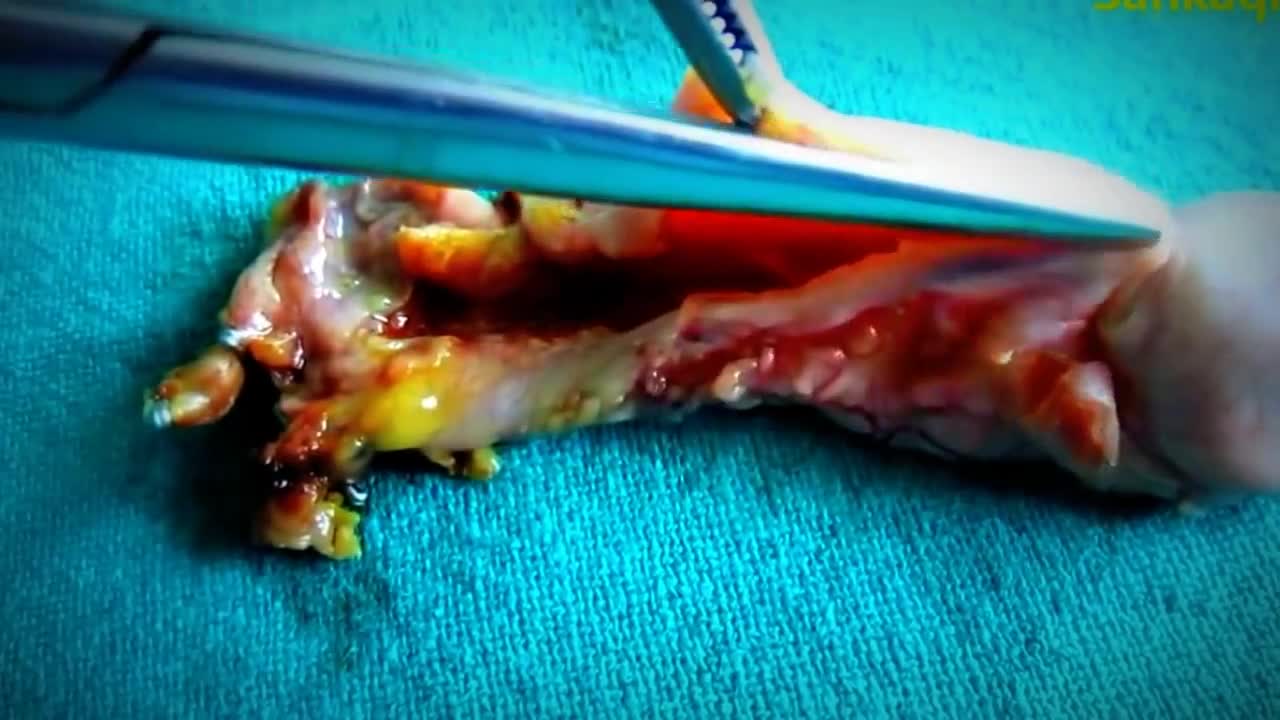
Hematoma Removal! Surgery, Blood, Popping
Simple interrupted suturing is the most basic and most important of the suturing techniques.
Head Cyst watch to see more
Huge Abscess On Man's Jaw surgery
Huge CYST in Abdomin
Usually a sebaceous cyst grows very slowly and doesn't cause pain. However, they can become inflamed or infected, with the overlying skin becoming red, tender, and sore. Sometimes, they occur on a site that is constantly irritated, such as a cyst on your neck that rubs against your collar.
GIANT CELL TUMOR REMOVAL Plastic, Cosmetic and Reconstructive
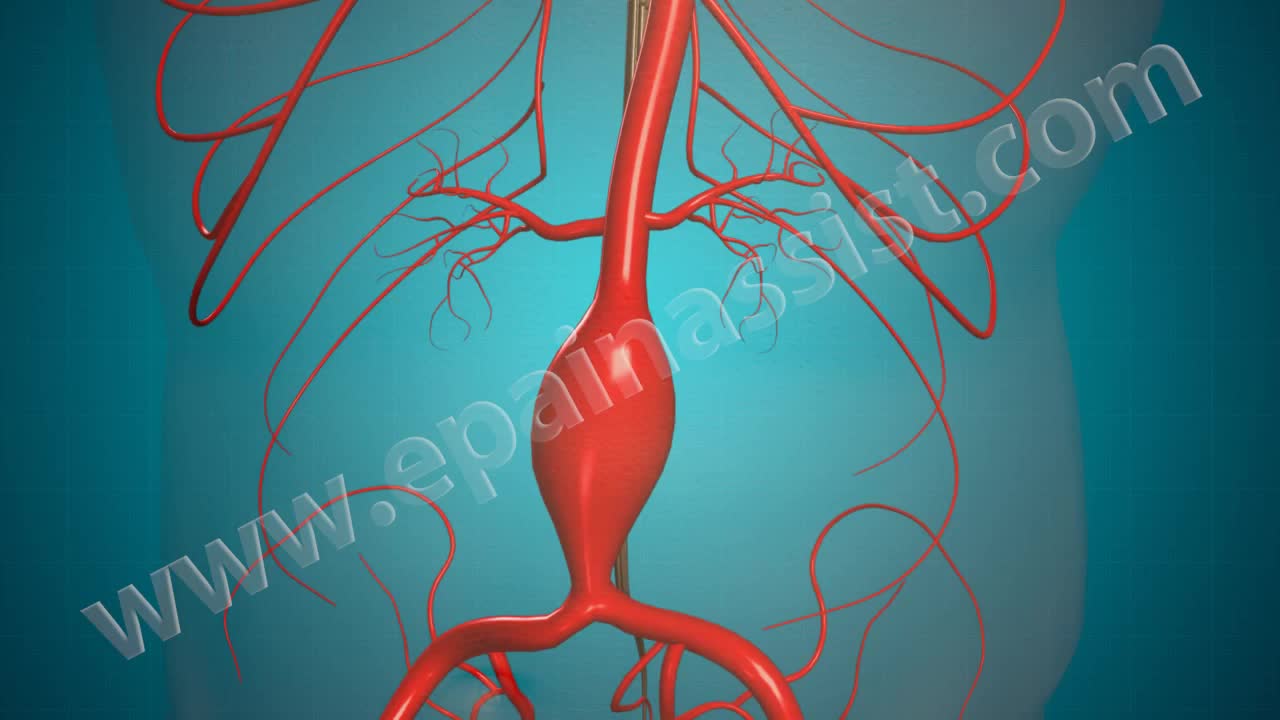
Open Abdominal Aortic and Endovascular Aneurysm Repair Surgery
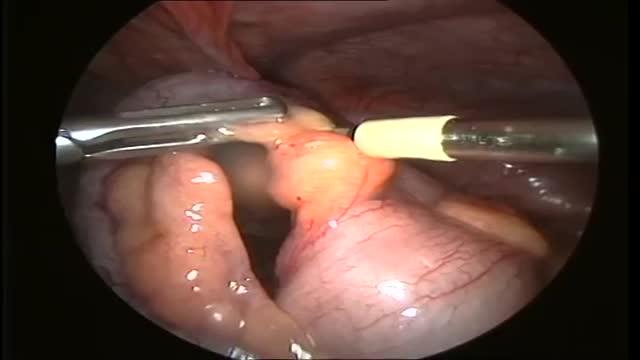
Your body needs bile, but if it has too much cholesterol in it, that makes gallstones more likely. It can also happen if your gallbladder can't empty properly. Pigment stones are more common in people with certain medical conditions, such as cirrhosis (a liver disease) or blood diseases such as sickle cell anemia.
SPIDER Surgery-- Single Incision Gallbladder Removal
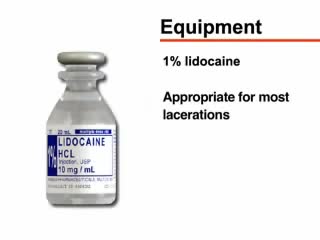
A nonsurgical method of treating a ganglion is to drain the fluid from (aspirate) the ganglion sac. Your doctor can do this in the office using the following procedure: The ganglion area is cleaned with an antiseptic solution. A local anesthetic is injected into the ganglion area to numb the area. When the area is numb, the ganglion sac is punctured with a sterile needle. The fluid is drawn out of the ganglion sac. The ganglion collapses. A bandage and, in some cases, a splint are used for a few days to limit movement and prevent the ganglion sac from filling again. Treating a ganglion by draining the fluid with a needle may not work because the ganglion sac remains intact and can fill again, causing the ganglion to return. For this reason, your doctor may puncture the sac with the needle 3 or 4 times so the sac will collapse completely. Even then, the ganglion is likely to come back.
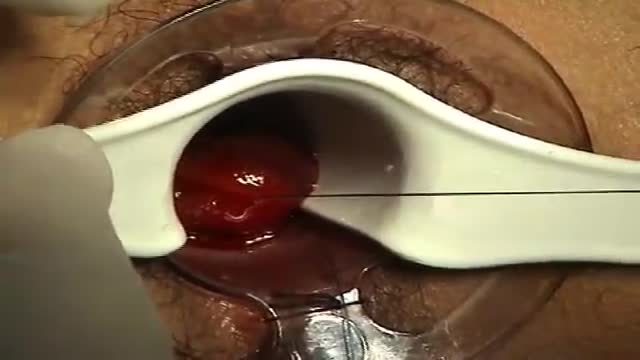
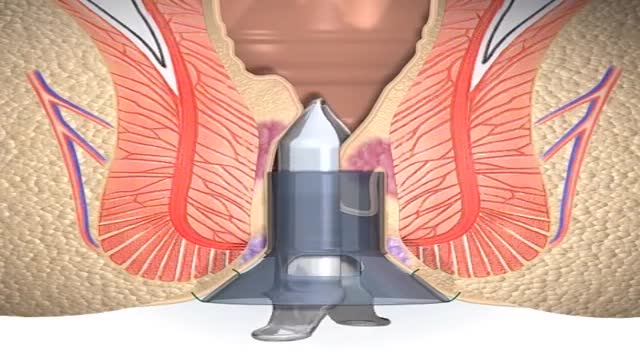
minimally invasive procedure is the new gold standard for hemorrhoidectomy, according to American and European experts in the field. The procedure, known as PPH (procedure for prolapse and hemorrhoids) stapled hemorrhoidectomy, combines hemorrhoidal devascularization and repositioning to return the veins to the anal canal. “This year, this is the revolutionary new procedure in the United States,” Gary Hoffman, MD, clinical faculty member in general and colorectal surgery, Cedars-Sinai Medical Center, Los Angeles, told General Surgery News after moderating a live PPH telesurgery at the 2003 annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
One thing we do know: We can live without it, without apparent consequences. Appendicitis is a medical emergency that requires prompt surgery to remove the appendix. Left untreated, an inflamed appendix will eventually burst, or perforate, spilling infectious materials into the abdominal cavity.
A Chinese hospital in the process of creating a human ear almost entirely through the human anatomy alone.
knife spoon and toothbrush removed from stomach
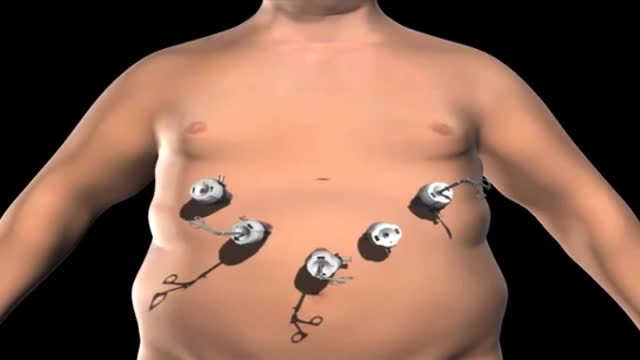
Super Obese individuals (people with a Body Mass Index over 45) have an increased risk during any surgery. And the longer the time under anesthesia, the greater the risk. Gastric bypass surgery can last over 2 hours. Duodenal switch surgery often takes over 4 hours. That’s a long time to be under anesthesia.
Haemorrhoids is one of the most common problems seen in surgical OPD. Open haemorrhoidectomy has remained the gold standard for a long time with a high post-operative morbidity. The quest for a better understanding of the pathology of haemorrhoids resulted in the evolvement of stapler haemorrhoidopexy. Our aim is to study the efficacy of stapler haemorrhoidopexy with regards to role of immediate post-operative morbidity. A prospective study of 50 patients (n = 50) with the second- and third-degree symptomatic haemorrhoids was done. The mean age of the patients was 44.1 years. Fourteen patients had co-morbid conditions. The average duration of the operation was 29 min. Patients with the second-degree haemorrhoids had higher rate of complication. The complication rate was 32%. Three patients had urinary retention. Two patients had minor bleeding, and one patient experienced transient discharge. The mean analgesic requirement was 2.4 tramadol, 50 mg injections. Ten patients had significant post-operative pain. Average length of hospital stay was 2.7 days. There were no symptomatic recurrences till date.
A stapled haemorrhoidopexy is an operation to return the haemorrhoids to a normal. position inside the rectum (back passage). A circular shaped stapling device is gently. inserted in the back passage. The surgeon is then able to use the device to remove.
Dumping syndrome is a condition that can develop after surgery to remove all or part of your stomach or after surgery to bypass your stomach to help you lose weight. Also called rapid gastric emptying, dumping syndrome occurs when food, especially sugar, moves from your stomach into your small bowel too quickly.Diet: Eating too much sugar can cause sugars to pass into the colon, making the bacteria there get all excited and cause diarrhea. Other things like sorbitol, a sweetener in some sugarless candy, can also cause diarrhea through osmosis. Malabsorption: Some people don't digest sugars or fats properly.
Mesenteric cyst is one of the rarest abdominal tumours, with approximately 820 cases reported since 1507. The incidence varies from 1 per 100,000 to 250,000 admissions. The lack of characteristic clinical features and radiological signs may present great diagnostic difficulties.