Surgery Videos

Whereas it is true that no operation has been profoundly affected by the advent of laparoscopy than cholecystectomy has, it is equally true that no procedure has been more instrumental in ushering in the laparoscopic age than laparoscopic cholecystectomy has. Laparoscopic cholecystectomy has rapidly become the procedure of choice for routine gallbladder removal and is currently the most commonly performed major abdominal procedure in Western countries.[1] A National Institutes of Health consensus statement in 1992 stated that laparoscopic cholecystectomy provides a safe and effective treatment for most patients with symptomatic gallstones and has become the treatment of choice for many patients.[2] This procedure has more or less ended attempts at noninvasive management of gallstones. The initial driving force behind the rapid development of laparoscopic cholecystectomy was patient demand. Prospective randomized trials were late and largely irrelevant because advantages were clear. Hence, laparoscopic cholecystectomy was introduced and gained acceptance not through organized and carefully conceived clinical trials but through acclamation. Laparoscopic cholecystectomy decreases postoperative pain, decreases the need for postoperative analgesia, shortens the hospital stay from 1 week to less than 24 hours, and returns the patient to full activity within 1 week (compared with 1 month after open cholecystectomy).[3, 4] Laparoscopic cholecystectomy also provides improved cosmesis and improved patient satisfaction as compared with open cholecystectomy. Although direct operating room and recovery room costs are higher for laparoscopic cholecystectomy, the shortened length of hospital stay leads to a net savings. More rapid return to normal activity may lead to indirect cost savings.[5] Not all such studies have demonstrated a cost savings, however. In fact, with the higher rate of cholecystectomy in the laparoscopic era, the costs in the United States of treating gallstone disease may actually have increased. Trials have shown that laparoscopic cholecystectomy patients in outpatient settings and those in inpatient settings recover equally well, indicating that a greater proportion of patients should be offered the outpatient modality
Emphysema gradually damages the air sacs (alveoli) in your lungs, making you progressively more short of breath. Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease Smoking is the leading cause of emphysema. Your lungs' alveoli are clustered like bunches of grapes. In emphysema, the inner walls of the air sacs weaken and eventually rupture — creating one larger air space instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream. When you exhale, the damaged alveoli don't work properly and old air becomes trapped, leaving no room for fresh, oxygen-rich air to enter. Treatment may slow the progression of emphysema, but it can't reverse the damage.
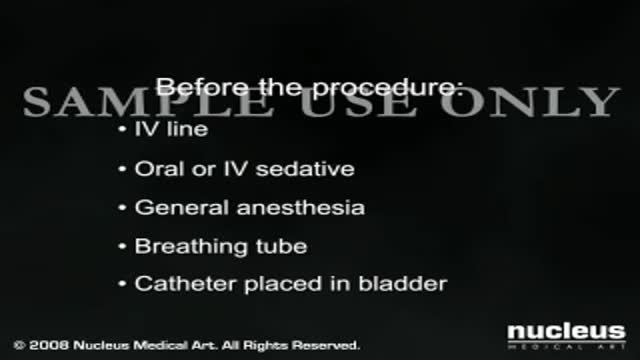
Coronary artery bypass graft surgery (CABG) is a procedure used to treat coronary artery disease. Coronary artery disease (CAD) is the narrowing of the coronary arteries – the blood vessels that supply oxygen and nutrients to the heart muscle. CAD is caused by a build-up of fatty material within the walls of the arteries. This build-up narrows the inside of the arteries, limiting the supply of oxygen-rich blood to the heart muscle. One way to treat the blocked or narrowed arteries is to bypass the blocked portion of the coronary artery with a piece of a healthy blood vessel from elsewhere in the body. Blood vessels, or grafts, used for the bypass procedure may be pieces of a vein from the legs or an artery in the chest. An artery from the wrist may also be used. One end of the graft is attached above the blockage and the other end is attached below the blockage. Blood is routed around, or bypasses, the blockage by going through the new graft to reach the heart muscle. This is called coronary artery bypass surgery. Traditionally, to bypass the blocked coronary artery, a large incision is made in the chest and the heart is temporarily stopped so that the surgeon can perform the delicate procedure. To open the chest, the breastbone (sternum) is cut in half and spread apart. Once the heart is exposed, tubes are inserted into the heart so that the blood can be pumped through the body by a cardiopulmonary bypass machine (heart-lung machine). The bypass machine is necessary to pump blood while the heart is stopped and kept still in order for the surgeon to perform the bypass operation. While the traditional "open heart" procedure is still commonly done and often preferred in many situations, less invasive techniques have been developed to bypass blocked coronary arteries. "Off-pump" procedures, in which the heart does not have to be stopped, were developed in the 1990's. Other minimally invasive procedures, such as keyhole surgery (performed through very small incisions) and robotic procedures (performed with the aid of a moving mechanical device), may be used.
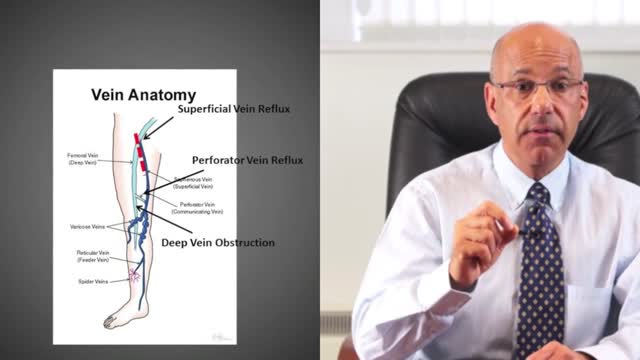
A leg ulcer is simply a break in the skin of the leg, which allows air and bacteria to get into the underlying tissue. This is usually caused by an injury, often a minor one that breaks the skin. In most people such an injury will heal up without difficulty within a week or two. However, when there is an underlying problem the skin does not heal and the area of breakdown can increase in size. This is a chronic leg ulcer.
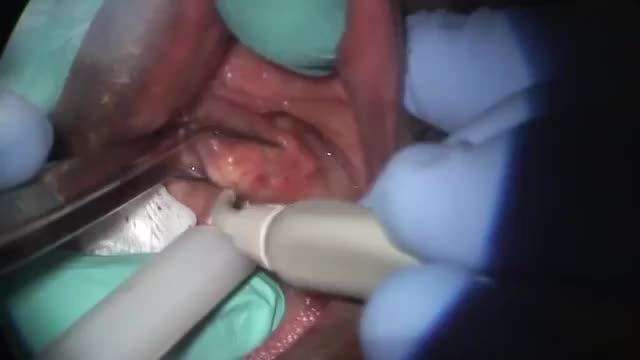
A salivary gland stone -- also called salivary duct stone -- is a calcified structure that may form inside a salivary gland or duct. It can block the flow of saliva into the mouth. The majority of stones affect the submandibular glands located at the floor of the mouth. Less commonly, the stones affect the parotid glands, located on the inside of the cheeks, or the sublingual glands, which are under the tongue. Many people with the condition have multiple stones. Salivary Gland Stone Causes and Symptoms Salivary stones form when chemicals in the saliva accumulate in the duct or gland. They mostly contain calcium. The exact cause is not known. But factors contributing to less saliva production and/or thickened saliva may be risk factors for salivary stones. These factors include: dehydration, poor eating, and use of certain medications (such as antihistamines), blood pressure drugs, psychiatric drugs, and bladder control drugs. Trauma to the salivary glands may also raise the risk for salivary stones. The stones cause no symptoms as they form, but if they reach a size that blocks the duct, saliva backs up into the gland, causing pain and swelling. You may feel the pain off and on, and it may get progressively worse. Inflammation and infection within the affected gland may follow. Salivary Gland Stones Diagnosis and Treatments If you have symptoms of a salivary gland stone, your doctor will first check for stones with a physical exam. Sometimes tests may also be ordered, such as X-ray, CT scan, or ultrasound.

Plantar warts are hard, grainy growths that usually appear on the heels or balls of your feet, areas that feel the most pressure. This pressure also may cause plantar warts to grow inward beneath a hard, thick layer of skin (callus). Plantar warts are caused by the human papillomavirus (HPV). The virus enters your body through tiny cuts, breaks or other weak spots on the bottom of your feet. Most plantar warts aren't a serious health concern and may not require treatment. But plantar warts can cause discomfort or pain. If self-care treatments for plantar warts don't work, you may want to see your doctor to have them removed.
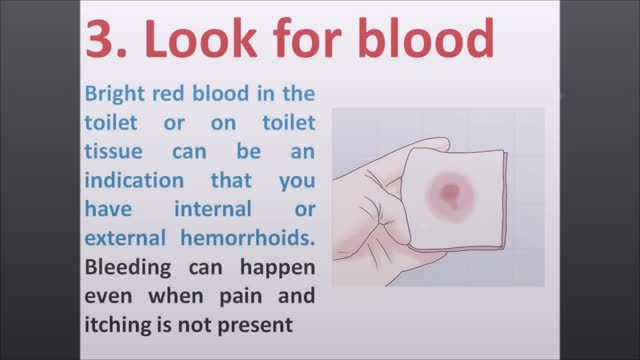
Most of the time, treatment for hemorrhoids involves steps that you can take on your own, such as lifestyle modifications. But sometimes medications or surgical procedures are necessary. Medications If your hemorrhoids produce only mild discomfort, your doctor may suggest over-the-counter creams, ointments, suppositories or pads. These products contain ingredients, such as witch hazel or hydrocortisone, that can relieve pain and itching, at least temporarily. Don't use an over-the-counter cream or other product for more than a week unless directed by your doctor. These products can cause side effects, such as skin rash, inflammation and skin thinning. Minimally invasive procedures If a blood clot has formed within an external hemorrhoid, your doctor can remove the clot with a simple incision, which may provide prompt relief. For persistent bleeding or painful hemorrhoids, your doctor may recommend another minimally invasive procedure. These treatments can be done in your doctor's office or other outpatient setting. Rubber band ligation. Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation. The hemorrhoid withers and falls off within a week. This procedure — called rubber band ligation — is effective for many people. Hemorrhoid banding can be uncomfortable and may cause bleeding, which might begin two to four days after the procedure but is rarely severe. Injection (sclerotherapy). In this procedure, your doctor injects a chemical solution into the hemorrhoid tissue to shrink it. While the injection causes little or no pain, it may be less effective than rubber band ligation. Coagulation (infrared, laser or bipolar). Coagulation techniques use laser or infrared light or heat. They cause small, bleeding, internal hemorrhoids to harden and shrivel. While coagulation has few side effects, it's associated with a higher rate of hemorrhoids coming back (recurrence) than is the rubber band treatment. Surgical procedures If other procedures haven't been successful or you have large hemorrhoids, your doctor may recommend a surgical procedure. Surgery can be performed on an outpatient basis or you may need to stay in the hospital overnight. Hemorrhoid removal. During a hemorrhoidectomy, your surgeon removes excessive tissue that causes bleeding. Various techniques may be used. The surgery may be done with a local anesthetic combined with sedation, a spinal anesthetic or a general anesthetic. Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications may include temporary difficulty emptying your bladder and urinary tract infections associated with this problem. Most people experience some pain after the procedure. Medications can relieve your pain. Soaking in a warm bath also may help. Hemorrhoid stapling. This procedure, called stapled hemorrhoidectomy or stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. Stapling generally involves less pain than hemorrhoidectomy and allows an earlier return to regular activities. Compared with hemorrhoidectomy, however, stapling has been associated with a greater risk of recurrence and rectal prolapse, in which part of the rectum protrudes from the anus. Talk with your doctor about what might be the best option for you.
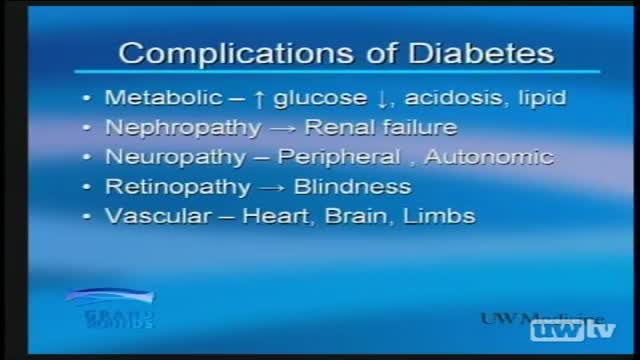
A pancreas transplant is a surgical procedure to place a healthy pancreas from a deceased donor into a person whose pancreas no longer functions properly. Your pancreas is an organ that lies behind the lower part of your stomach. One of its main functions is to make insulin, a hormone that regulates the absorption of sugar (glucose) into your cells. If your pancreas doesn't make enough insulin, blood sugar levels can rise to unhealthy levels, resulting in type 1 diabetes. Most pancreas transplants are done to treat type 1 diabetes. A pancreas transplant offers a potential cure for this condition. But it is typically reserved for those with serious diabetes complications, because the side effects of a pancreas transplant are significant. In some cases, pancreas transplants may also treat type 2 diabetes. Rarely, pancreas transplants may be used in the treatment of pancreatic, bile duct or other cancers. A pancreas transplant is often done in conjunction with a kidney transplant in people whose kidneys have been

Barbed sutures first received US Food and Drug Administration approval for soft tissue approximation in 2005 and early adopters readily embraced this device to develop new techniques. It has become apparent that the advantages are more than just "skin deep." Superficial and deep fascia, cartilage, tendon, joint capsule, and fibrous periprosthetic capsules can also be manipulated. Barbed sutures have revolutionized our approach to facial rejuvenation and body contouring by enhancing our ability to quilt and powerfully lift tissue. The elimination of surgical drains and shorter surgical times has made this a true boon for plastic surgeons as well as many other surgical specialists. This article summarizes some of the current and evolving applications of this exciting new tool.

Proper placement of sutures enhances the precise approximation of the wound edges, which helps minimize and redistribute skin tension. Wound eversion is essential to maximize the likelihood of good epidermal approximation. Eversion is desirable to minimize the risk of scar depression secondary to tissue contraction during healing. Usually, inversion is not desirable, and it probably does not decrease the risk of hypertrophic scarring in an individual with a propensity for hypertrophic scars. The elimination of dead space, the restoration of natural anatomic contours, and the minimization of suture marks are also important to optimize the cosmetic and functional results.
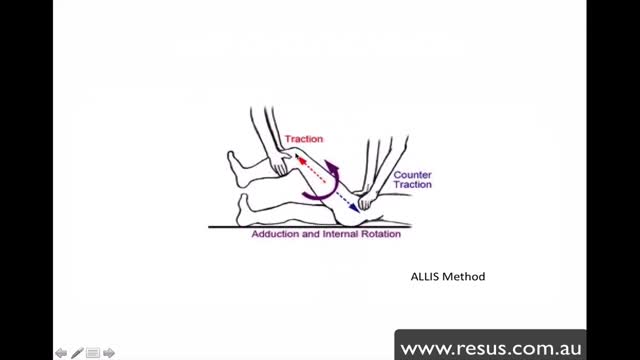
The hip joint is formed between the 'ball' of the femoral head and the 'socket' of the acetabulum and a cartilaginous labrum. Strong supporting muscles, the fibrous joint capsule and ischiofemoral ligament make this a stable joint. Hip dislocations are either congenital or traumatic. Congenital dislocation of the hip is caused by dysplasia of the femoral head or acetabulum and is covered in the separate article Developmental Dysplasia of the Hip. This remainder of this article deals with traumatic dislocation. Traumatic hip dislocation is an orthopaedic emergency. Large forces are required to cause hip dislocation (except in prosthetic hips) and this means that such injury may be associated with other life-threatening injuries and other fractures. The condition is extremely painful. Accurate and swift diagnosis means appropriate management can reduce morbidity.

Tracheotomy is a surgical procedure which consists of making an incision on the anterior aspect of the neck and opening a direct airway through an incision in the trachea (windpipe). The resulting stoma (hole), or tracheostomy, can serve independently as an airway or as a site for a tracheostomy tube to be inserted; this tube allows a person to breathe without the use of his or her nose or mouth. Both surgical and percutaneous techniques are widely used in current surgical practice. It is among the oldest described procedures.

An amputation is the removal of an extremity or appendage from the body. Amputations in the upper extremity can occur as a result of trauma, or they can be performed in the treatment of congenital or acquired conditions. Although successful replantation represents a technical triumph to the surgeon, the patient's best interests should direct the treatment of amputations. The goals involved in the treatment of amputations of the upper extremity include the following : Preservation of functional length Durable coverage Preservation of useful sensibility Prevention of symptomatic neuromas Prevention of adjacent joint contractures Early return to work Early prosthetic fitting These goals apply differently to different levels of amputation. Treatment of amputations can be challenging and rewarding. It is imperative that the surgeon treat the patient with the ultimate goal of optimizing function and rehabilitation and not become absorbed in the enthusiasm of the technical challenge of the replantation, which could result in poorer outcome and greater financial cost due to lost wages, hospitalization, and therapy.

Skin Cysts Cysts are noncancerous, closed pockets of tissue that can be filled with fluid, pus, or other material. Cysts are common on the skin and can appear anywhere. They feel like large peas under the surface of the skin. Cysts can develop as a result of infection, clogging of sebaceous glands (oil glands), or around foreign bodies, such as earrings.