Surgery Videos
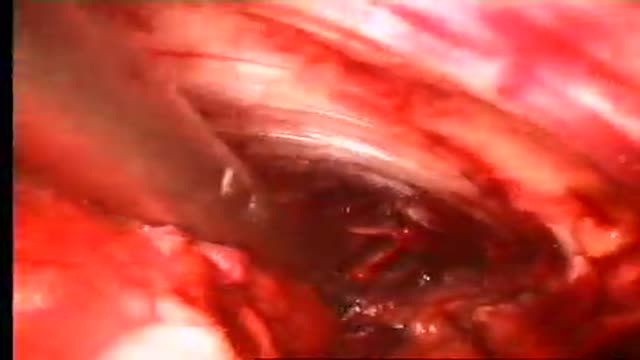
Purpose The complication rate in patients treated with the Linton procedure was unacceptably high. SEPS is minimal invasive treatment modality for chronic venous insufficiency and venous ulcers. Materials and Methods252 limbs of 229 patients who underwent SEPS procedure and/or safenous vein ablati...on from May 2003 to January 2008. Tourniquet was not used and two-port technique was preferred for operation. Skin graft was not used. Honeysoft (medical honey) was used for wound care in selected cases. Results According to CEAP clinical Classification 112 limbs were class 6, 70 limbs (class 5), 70 limbs (Class4) respectively. Greater saphenous vein stripping and/or high ligation, and varicose vein excision accompanied SEPS in 241limbs who had combined Sapheno-femoral junction and perforator vein insufficiencyand SEPS was performed alone 23 limbs who had recanalised deep venous thrombosis (19) and PVI alone(4). Mean patient follow-up was 35 months. No early deaths or thromboembolism occurred. Complications included severe subcutaneous emphysema(1), neuralgia (7), 1 year later cellulites (1). Ulcers healed in 124 limbs in two months and 58 limbs in 3 months. ulcer recurrence was seen on 12(%6.6) limbs. Clinical severity and disability scores improved significantly after surgery. Conclusion All venous ulcers healed with SEPS combined or not ablation of superficial venous reflux and remain healed 5 year period and symptom-free except recurrent ulcers during the long-term follow-up. SEPS is an effective and safety treatment modality.
Cholecystectomy
Surgical technique: A 3cm skin incision under spinal or general anesthesia, depending on the patients’ preference, starts half way the line between the superior anterior iliac spine towards the midline in a 30° angle to the pubic tubercle. Scarpa’s fascia is opened as well as the external obliq...ue aponeurosis. By using this skin line incision the internal ring will be immediately visualized. Although it is important to look for both direct and indirect hernias evaluating the groin, we do not taper the cord and directly evaluate the ring for indirect hernias. In case of an indirect hernia the sac is reduced or resected according to the preference of the surgeon and the preperitoneal space is entered bluntly through the dilated internal ring. In case of a direct hernia the approach slightly differs. One could prefer to open the transversalis fascia through the internal ring over a few centimeters or you can open the fascia more medially, at the site of the direct hernia. As primary point of concern the epigastric vessels should be identified and retracted softly upwards. Then a gauze can be introduced into the preperitoneal space and by doing so most of the space needed medially will be created. Then one can already palpate Cooper’s ligament and the pubic bone. Laterally to the internal ring more digital dissection is needed to create just the appropriate space for the mesh. By placing the mesh it is important not to introduce the mesh too medially. Laterally of the internal ring an adequate overlap of the mesh is necessary, especially in indirect hernias. No splitting of the mesh seems necessary. The patient will be asked to strain and push on the ring to control its place and to check adequate spreading of the mesh to cover the whole myopectineum of Fruchaud. One single stitch of vicryl 3/0 is placed taking both the fascia transversalis and the mesh.
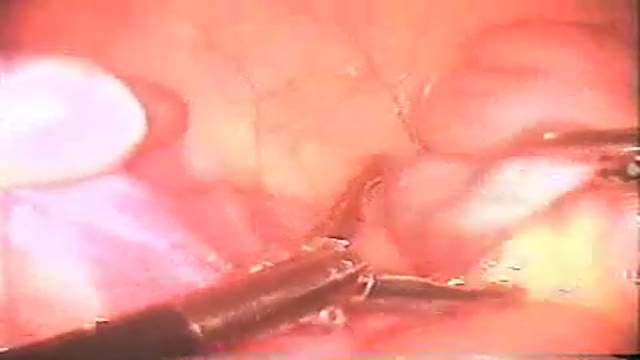
Laparoscopic Appendicectomy
Truncal Vagotomy and Pyloroplasty
Appendectomy with corpus Luteal rupture
Esophagomyotomy for Achalasia
Splenectomy surgery video
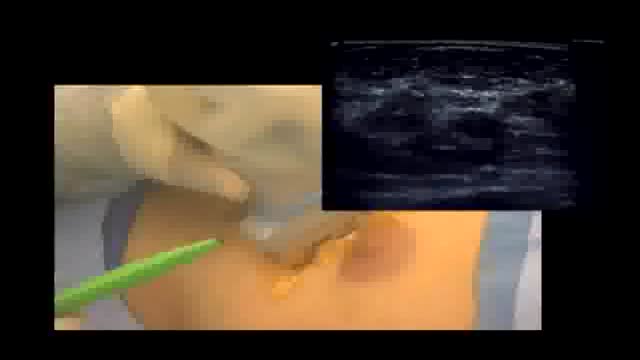
Excision of breast cancer that is visible only on mammogram. diagnosis is typically established on stereotactic biospy and excision is done with wire localization. This techniques involves localization by sonography of the hematoma that is left behind at the time of biopsy. It provides not only accu...rate location of the tumor but ensures adequate margins of excision.
What is a Whipple procedure?
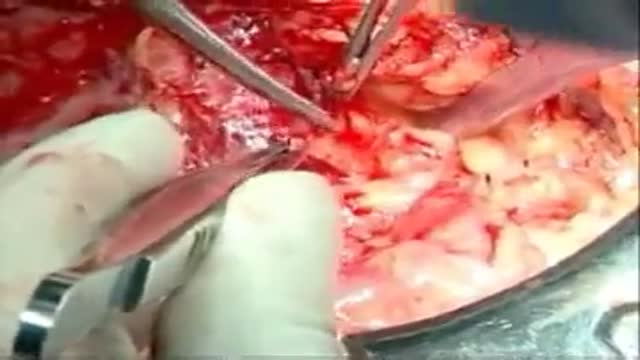
Also called a pancreaticoduodenectomy, the Whipple procedure is performed to address chronic pancreatitis and cancer of the pancreas, ampulla of Vater, duodenum, and the distal bile duct. The Whipple procedure involves removing the cancerous parts of the pancreas, duodenum, common bile duct, and if required, part of the stomach.
Various laparoscopic techniques have been described for the insertion of peritoneal dialysis catheters. However, most use 3 to 4 ports, thus multiplying the potential risk for abdominal wall complications (hemorrhage, hernia, leaking). With the technique presented herein a Tenckhoff catheter is plac...ed laparoscopically, using just 1 port, in 13 consecutive patients with end-stage renal failure. The catheter is fixed in the abdominal cavity with no additional ports for this purpose. The simplicity and the rapidity of the method justifies serious consideration for its use as the standard Tenckhoff catheter placement.
Hand Assisted Nephrectomy
Lichtenstein mesh repair of hernia
Mesh repair is based on the anatomical principle with associated complications of a foreign body and recurrence. Use of an un-detached strip of the external oblique aponeurosis in place of mesh between the muscle arch and the inguinal ligament gives a strong and physiologically dynamic posterior wal...l that gives radical cure.
Recommendations for clipping in endoscopic stomach surgery
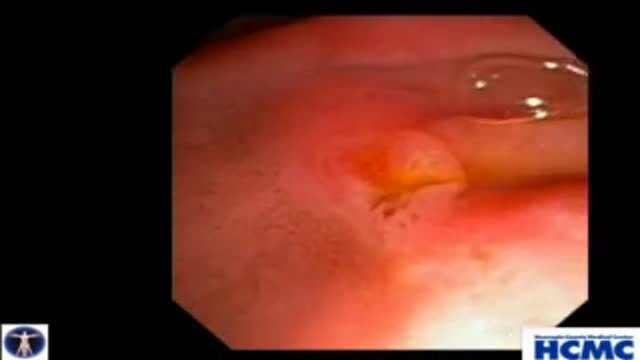
Colon - Polypectomy, Saline lift, Adenomas
This 38 year old woman has increasingly intractable RUQ pain after cholecystectomy done one year prior. LFTs and pancreatic enzymes have been normal, and ducts are non-dilated, thus she is a Type III possible SOD patient. Initial goal is to define course of pancreatic duct for manometry. 5-4-3 Co...ntour catheter (Boston Scientific) is used to perform the pancreatogram which shows a small straight distal duct. The aspirating triple lumen manometry catheter (Wilson Cook) is used to cannulate the pancreatic duct, with continuous aspiration of fluid once the duct is entered. Careful stationed pullthrough manometry shows markedly abnormal basal pressures in both leads in the pancreatic sphincter. Plan is dual pancreatic and biliary sphincterotomy. Biliary manometry will not now change our plan therefore is omitted. Our first goal is to access the pancreatic duct so we can guarantee wire access for placement of a small caliber pancreatic stent which is critical for safety. Contrast is injected as the 0.018in Roadrunner wire (Wilson Cook) is advanced in order to outline the course of main duct. A separate biliary orifice is clearly seen, unusual in SOD patients. A soft 4Fr 3cm single inner flange pancreatic stent (Hobbs Medical) is placed. We did not want to use our typical 9cm long unflanged stent as even a 3 or 4 French stent might be traumatic to the tiny caliber of this duct out in the body of the gland. Next the bile duct is cannulated with a papillotome (Autotome 39, Boston Scientific), showing a small perhaps 6mm bile duct. Biliary sphincterotomy is performed in very careful stepwise fashion as landmarks are unclear and perforation is higher risk in small duct SOD patients. On the other hand, inadequate sphincterotomies offer limited chance of symptom relief. You can see here a patulous sphincterotomy. Next a pancreatic sphincterotomy is performed with the needle knife (Boston Scientific) over the pancreatic stent. Again this is performed cautiously due to the small size of the pancreatic duct. We are reaching along the stent and cutting the fibers deeply. This is a limited pancreatic sphincterotomy due to small pancreatic duct size, and concern for scarring of the pancreatic duct. It is important to document passage of the stent by xray or remove it endoscopically with two weeks or so. We and many other specialized centers perform dual sphincterotomies at the first ERCP in all SOD patients with abnormal pancreatic manometry and frequent or intractable symptoms based on the belief that response rates are better than for biliary sphincterotomy alone.
Next to esophagojejunostomy stapling for the reconstruction following total gastrectomy, several silk stitches anchoring the jejunum to endoabdominal fascia are made to restore the function of phrenoesophageal ligament.
anchoring suture reduces the impairment of the anastomotic blood flow that is caused by gravitational tension and so is useful to protect the esophagojejunostomy after total gastrectomy.
Stapled hemorrhoidectomy for acute hemorrhoidal crisis could be undertaken under local anathesia with early recovery, short hospital stay and minimal postoperative pain
Appendectomy (midline caecum)