Surgery Videos
Hemorrhoidectomy Operation Video
Hemorrhoidectomy Ligasure
Mechanical Anopexy
Hemorrhoidectomy
Complete perineal tear reconstruction Video Surgery
Complete perineal tear reconstruction video surgery
Laparoscopic repair of hernia with mesh
Mesenteric Vessel Ligation Operation
Aneurysm of Splenic Artery from Cairo College of Medicine Hospitals
Median Sternotomy
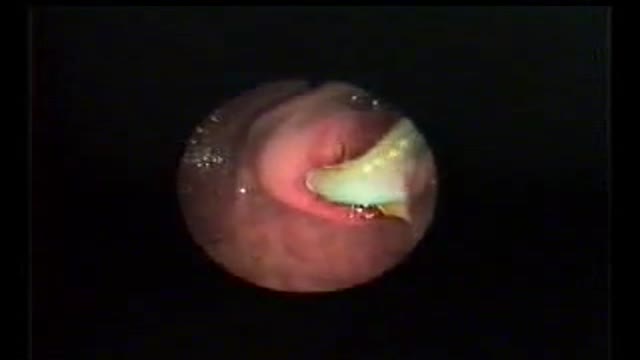
A 30 YEAR WOMEN WITH INTRACTABLE BILIARY COLIC CASE REPORT: This 30 year women developed severe pain right upper quadrant for last 10 days. She sought many consultations and was given intravenous analgesics both (nonnarcortic and narcotic). Pain did not subside and she sought my consultation. Examination revealed her to be in agony with severe upper abdominal pain. General physical examination was otherwise unremarkable. Abdominal examination revealed mild tenderness in right hypochondrium with doubtful Murphy's sign. Urgent abdominal ultrasound showed a linear structure in bile ducts making slow writhing movements. The structure had an anechoic tube (alimentary canal) inside suggestive of a large Ascarid. Urgent ERCP was performed and bile duct and pancreatic duct cannulated selectively. Pancreatic duct was normal. Bile ducts contained a long linear filling defect extending from lower end of common bile duct to right intrahepatic duct (see image gallery for ERCP plate). A basket was introduced in the duct (see video clip) and the linear structure was engaged with soft closure and extracted out of the bile duct. Accompanying the basket was a 25 cm thick highly motile Ascarid. To recover the worm, endoscope was withdrawn along with the basket and the friendly catch. While the endoscope was being withdrawn and the basket was in the duodenum with the worm out of bile duct, patient indicated of relief of abdominal pain. A relook cholangiogram showed no more structures in the duct. She was given antihelmintic therapy and passed hundreds of worms with the feces. The worms recovered form stools were both male and female population and varied in length and size. However the lone worm recovered form bile ducts was the longest and the thickest male worm. The phenomenal behavior of this ubiquitous infection remains unexplained. (Source Records from Dr. Khuroo's Medical Clinic. Review prepared by Mehnaaz Sultan Khuroo Host website www.drkhuroo.org , E-mail: mkhuroo@yahoo.com ).
Transurethral resection of the prostate (also known as TURP, plural TURPs and as a transurethral prostatic resection TUPR) is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, it is performed by visualising the prostate through the urethra and removing tissue by electrocautery or sharp dissection. This is considered the most effective treatment for BPH. This procedure is done with spinal or general anesthetic. A large triple lumen catheter is inserted through the urethra to irrigate and drain the bladder after the surgical procedure is complete. Outcome is considered excellent for 80-90% of BPH patients. Because of bleeding risks associated with the surgery, TURP is not considered safe for many patients with cardiac problems. As with all invasive procedures, the patient should first discuss medications they are taking with their doctor, most especially blood thinners or anticoagulants, such as warfarin (Coumadin), or aspirin. These may need to be discontinued prior to surgery. Postop complications include bleeding (most common), clotting and hyponatremia (due to bladder irrigation).
Additionally, transurethral resection of the prostate is associated with low but important morbidity and mortality.
A video showing surgery for hydrocele
A laparoscopic view of the diaphragmatic hernia
A German video showing varicocele surgery
Open Inguinal Hernia Operation (German)
Laparoscopic fixation of intraabdominal testis into the scrotum in a case of undescended testis.
Bandaging a freshly above the knee amputated limb
A 54 year old man with a left leg tumor, a vascular malformation, undergoes resection (removal) of the tumor.
ENDOSCOPIC (NON-SURGICAL) REMOVAL OF MULTIPLE LARGE TUMORS FROM STOMACH IN A PATIENT WITH PEUTZ-JEGHERS SYNDROME
PEUTZ-JEGHERS SYNDROME: Peutz-Jeghers syndrome (PJS) is a familial syndrome consisting of mucocutaneous pigmentation, gastrointestinal polyposis and cancers of gut & other sites like breast, ovary, and testes. PJS has an autosomal dominant inheritance with variable and incomplete penetrance. Germline mutations of STK11/LKB1 gene on 19p cause this syndrome. Mucocutaneous pigmentation may be noted in early infancy. These deposits of melanin are most commonly found around the mouth, nose, lips, buccal mucosa, hands, and feet, and may also be present in perianal and genital areas. PJS polyps may be found in stomach, small intestine, or colon, but they tend to be prominent in the small intestine. These polyps may increase in size and cause small intestinal obstruction or intussusceptions that may occur in early infancy. Acute upper gastrointestinal bleeding and chronic faecal blood may complicate the disease.
PATIENT: The patient was a 25 yr male who had mucocutaneous pigmentation and multiple polyps in the stomach and duodenum. He presented with bleeding from gastric polyps. As the polyps in stomach were numerous, (more than 20 in number) and were large in size (some equal to small egg size), he had been advised to undergo surgery. Surgery planned was total gastrectomy.
PROCEDURE: The patient underwent video-endoscopy of the esophagus, stomach and duodenum. All polyps were examined for size and presence or absence of stalk. A plan to remove all the gastric polyps at endoscopy was made in the same sitting. He received light conscious sedation. Flat polyps were raised form the gastric wall by injection of saline in to polyp base to let these lesions have a stalk. This was done by needle injector. Each polyp was engaged in a snare and the polyp stalk was cut by coagulation cutting current. The cuts were clean without any bleeding. All polyps were recovered for histology. The histology revealed all polyps to be hamartomous lesions. None of the polyps were cancerous. Patient has been followed up for over one year and is doing fine without any further bleeding or pain.
Video shows the procedure of videoendoscpy and endoscopic removal of polyps.