Otorhinolaryngology
Terrifying Sinus Infection - Disturbing - Must Watch
A peritonsillar abscess forms in the tissues of the throat next to one of the tonsils. An abscess is a collection of pus that forms near an area of infected skin or other soft tissue. The abscess can cause pain, swelling, and, if severe, blockage of the throat. If the throat is blocked, swallowing, speaking, and even breathing become difficult. When an infection of the tonsils (known as tonsillitis) spreads and causes infection in the soft tissues, a peritonsillar abscess may result. Peritonsillar abscesses are generally uncommon. When they do occur they are more likely among young adults, adolescents, and older children.
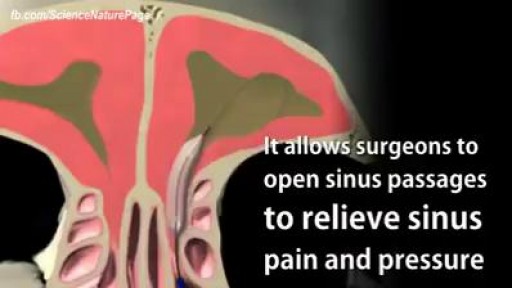
Balloon Sinuplasty for Sinus Infection
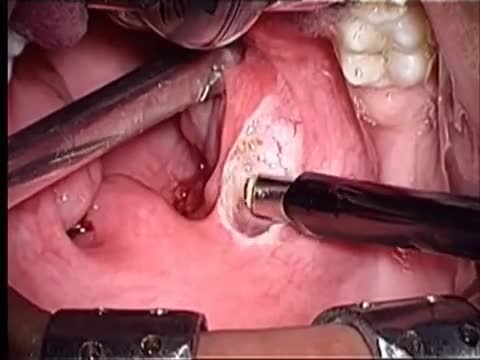
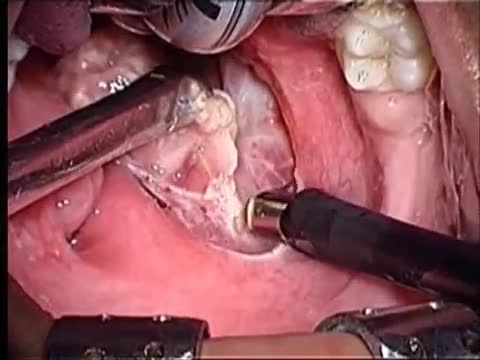
Surgical procedure of Tonsillectomy and Adenoidectomy
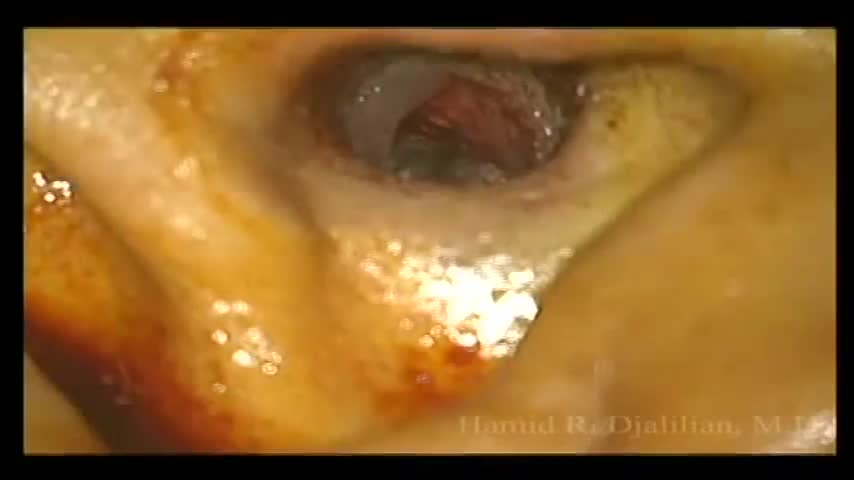
GIANT EAR WAX REMOVAL By using the elephant ear device.It's very useful video for medical students.Please share it!
Sinus infections caused by viruses can use home (over-the-counter, OTC) treatments such as pain and fever medications (acetaminophen [Tylenol]), decongestants, and mucolytics. In addition, some health-care professionals suggest nasal irrigation or a sinus rinse solution to help relieve symptoms of sinus infections, even chronic sinusitis symptoms.
Think you're supposed to tilt your head to the sky when you have a nosebleed? Not so fast. Follow these steps instead:
Removing a hump from the bridge is one of the most common things people want addressed during their rhinoplasty. Nasal humps can range widely in size. Perhaps you just have a small bump that you'd like refined? Or maybe you have more of a Roman Nose with a more dominating, distracting large hump? No matter if your nose falls on one of these extremes or somewhere in between rhinoplasty surgery can be used to reshape your nose. For anyone considering having a rhinoplasty to reduce a hump on their bridge there are several things to consider before having surgery.
A salivary gland stone -- also called salivary duct stone -- is a calcified structure that may form inside a salivary gland or duct. It can block the flow of saliva into the mouth. The majority of stones affect the submandibular glands located at the floor of the mouth.
Tonsil stones are hard yellow or white formations that are located on or within the tonsils. It’s common for people with tonsil stones to not even realize they have them. Tonsil stones aren’t always easily visible and they can range from rice- to pea-sized. Tonsil stones rarely cause larger health complications. However, sometimes they can grow into larger tonsilloliths which can cause your tonsils to swell
Sialendoscopy can be both diagnostic and therapeutic. It is complementary to diagnostic techniques such as plain radiography, ultrasonography, computed tomography (CT), magnetic resonance sialography, and conventional sialography, all of which are traditional, time-tested methods for evaluating the salivary ductal system
This procedure, and other types of soft palate surgery, targets the back of the roof of your mouth. It involves removing and repositioning excess tissue in the throat to make the airway wider. The surgeon can trim down your soft palate and uvula, remove your tonsils, and reposition some of the muscles of the soft palate. UPPP and other soft palate procedures are the most common type of surgery for sleep apnea. But UPPP alone is unlikely to cure moderate to severe sleep apnea. It may be combined with surgeries that target other sites in the upper airway.
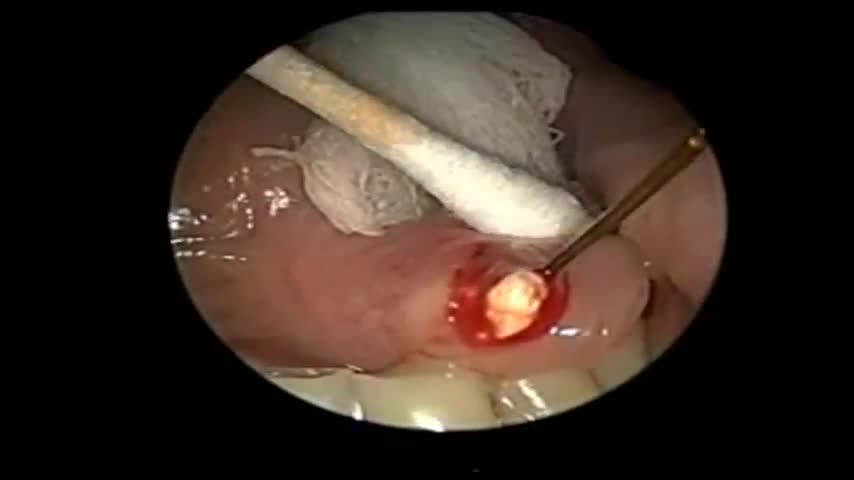
This is a surgery showing the removal of a large exostosis. Exostoses are bony growths in the ear canal from chronic exposure to cold water/air, most commonly from surfing. This patient had growths in both ears, which were completely obstructing the ear canals. This patient had a single exostosis that was blocking this side (the right side).
This video demonstrates how bronchoscopy and vocal cord mass injections can be performed under endoscopic guidance in a patient without any sedation. Only topical and local anesthesia is used for patient comfort.
Tonsillectomy using coblation technique by wand Evac 70
we use a single, tapered PDT dilator and kit . All the equipment and supplies listed must be present at the bed-side, because there is no time to go looking for supplies if an airway emergency occurs during the procedure. Two teams are used simultaneously. One team manages the endo-tracheal tube, and the other manages the placement of the tracheostomy tube
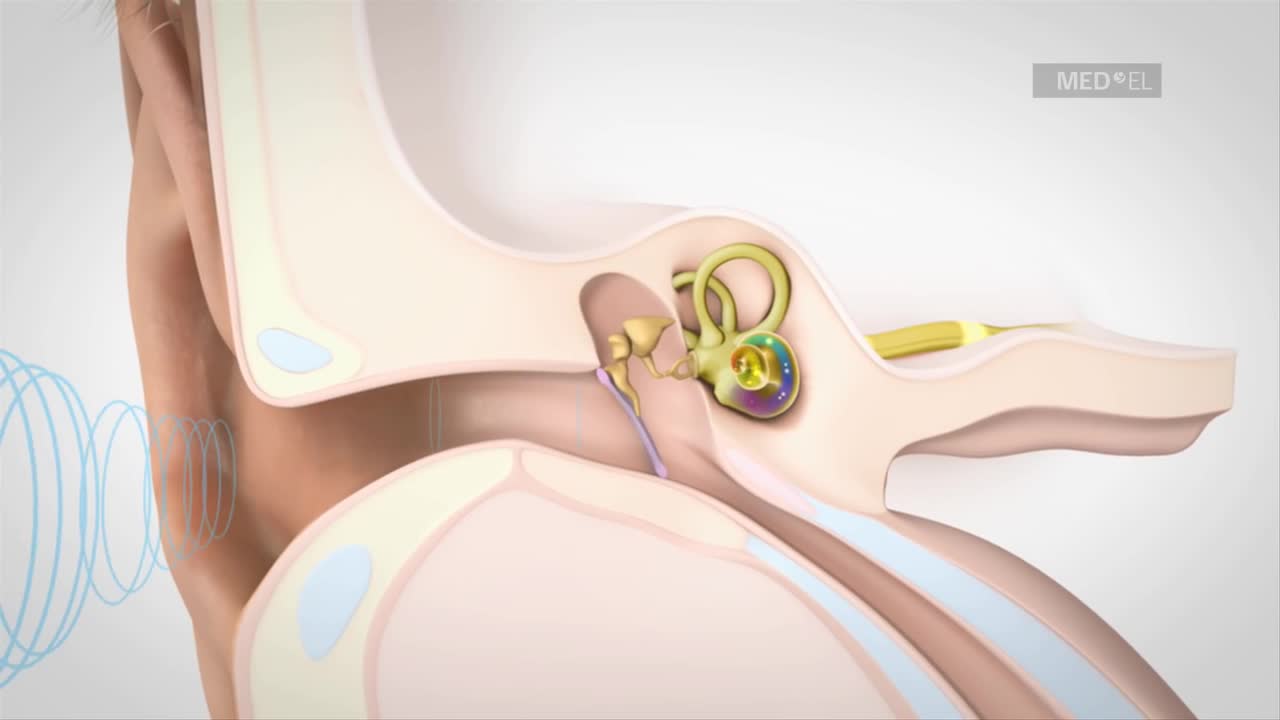
Video to help understand hearing loss and hearing impairment by explaining how hearing works. Cochlear implants can help children and adults with hearing loss
The treatment of peritonsillar abscess requires both the selection of appropriate antibiotics and the best procedure to remove the abscessed material. Individualized treatment modalities will result in more successful outcomes. The choice of antibiotics is highly dependent on both the gram stain and culture of the fluid obtained from the needle aspiration. Penicillin used to be the antibiotic of choice for the treatment of peritonsillar abscess, but in recent years the emergence of beta-lactamase-producing organisms has required a change in antibiotic choice.15 Results of studies16,17 suggest that 500 mg of clindamycin administered twice daily or a second- or third-generation oral cephalosporin be used instead of penicillin. Another study1 recommends using penicillin as the first-line agent, and, if there is no response within the first 24 hours, adding 500 mg of metronidazole administered twice daily to the regimen. All specimens should be examined by culture for antibiotic sensitivity to ensure appropriate antibiotic coverage. Three main surgical procedures are available for the treatment of peritonsillar abscess: needle aspiration, incision and drainage, and immediate tonsillectomy. Three recent studies have compared needle aspiration with incision and drainage for the treatment of peritonsillar abscess.16–18 In one study,16 52 consecutive patients who had a positive needle aspiration of a peritonsillar abscess were randomized into two groups comparing needle aspiration alone with incision and drainage.8 There were no significant differences between the two groups in duration of symptoms or initial treatment failure. The results indicated that no further surgical management for peritonsillar abscess was required following the initial needle aspiration. Another study17 conducted in 1991 reported similar results.
Microsurgical bipolar cautery tonsillectomy compares favorably with traditional techniques in terms of intraoperative bleeding, postoperative pain, otalgia, and hemorrhage. This technique combines the hemostatic advantage of cautery dissection, the excellent visualization achieved by a microscope, and, with the use of a video, greatly improves the physician's ability to teach how to perform a tonsillectomy.
Tonsillectomy (ton-sih-LEK-tuh-me) is the surgical removal of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side. A tonsillectomy was once a common procedure to treat infection and inflammation of the tonsils (tonsillitis). Today, a tonsillectomy is usually performed for sleep-disordered breathing but may still be a treatment when tonsillitis occurs frequently or doesn't respond to other treatments. A tonsillectomy may also be necessary to treat breathing and other problems related to enlarged tonsils and to treat rare diseases of the tonsils.