Anaesthesia
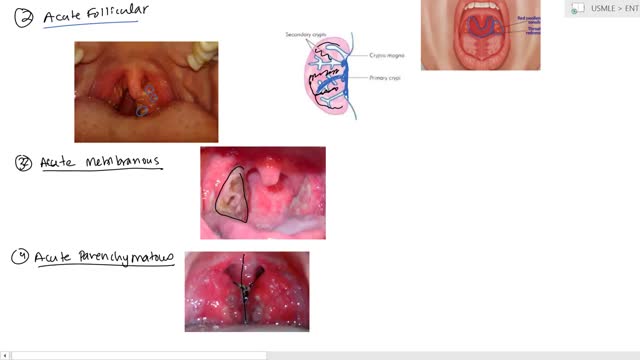
Tonsillitis is inflammation of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side. Signs and symptoms of tonsillitis include swollen tonsils, sore throat, difficulty swallowing and tender lymph nodes on the sides of the neck. Most cases of tonsillitis are caused by infection with a common virus, but bacterial infections also may cause tonsillitis. Because appropriate treatment for tonsillitis depends on the cause, it's important to get a prompt and accurate diagnosis. Surgery to remove tonsils, once a common procedure to treat tonsillitis, is usually performed only when bacterial tonsillitis occurs frequently, doesn't respond to other treatments or causes serious complications.

Pulmonary fibrosis is a lung disease that occurs when lung tissue becomes damaged and scarred. This thickened, stiff tissue makes it more difficult for your lungs to work properly. As pulmonary fibrosis worsens, you become progressively more short of breath. The scarring associated with pulmonary fibrosis can be caused by a multitude of factors. But in most cases, doctors can't pinpoint what's causing the problem. When a cause can't be found, the condition is termed idiopathic pulmonary fibrosis. The lung damage caused by pulmonary fibrosis can't be repaired, but medications and therapies can sometimes help ease symptoms and improve quality of life. For some people, a lung transplant might be appropriate.
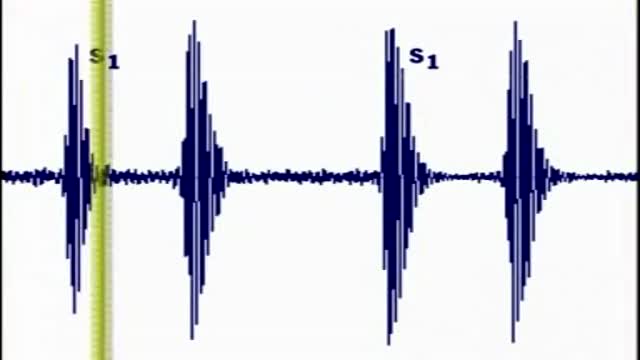
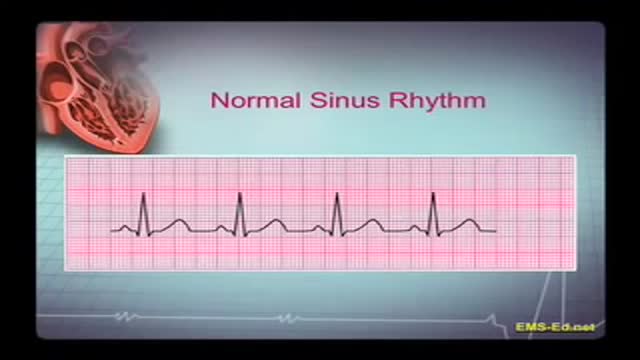
Heart sounds are the noises generated by the beating heart and the resultant flow of blood through it. Specifically, the sounds reflect the turbulence created when the heart valves snap shut. In cardiac auscultation, an examiner may use a stethoscope to listen for these unique and distinct sounds that provide important auditory data regarding the condition of the heart. In healthy adults, there are two normal heart sounds often described as a lub and a dub (or dup), that occur in sequence with each heartbeat. These are the first heart sound (S1) and second heart sound (S2), produced by the closing of the atrioventricular valves and semilunar valves, respectively. In addition to these normal sounds, a variety of other sounds may be present including heart murmurs, adventitious sounds, and gallop rhythms S3 and S4. Heart murmurs are generated by turbulent flow of blood, which may occur inside or outside the heart. Murmurs may be physiological (benign) or pathological (abnormal). Abnormal murmurs can be caused by stenosis restricting the opening of a heart valve, resulting in turbulence as blood flows through it. Abnormal murmurs may also occur with valvular insufficiency (regurgitation), which allows backflow of blood when the incompetent valve closes with only partial effectiveness. Different murmurs are audible in different parts of the cardiac cycle, depending on the cause of the murmur.

Pulmonary surfactant is a mixture of lipids and proteins that is produced by alveolar type II epithelial cells (AEC2) and secreted into the airspaces. Phospholipids are the major component of surfactant by weight, and are essential for lowering surface tension at the air-liquid interface, which prevents alveolar collapse at end-expiration. Four proteins highly expressed in the lung and found in surfactant are designated surfactant proteins (SP) A, B, C, and D. Additional proteins including ABCA3 and NKX2.1 are also important for the production of functional surfactant. The surfactant proteins are developmentally regulated, such that their expression increases in later gestation

Shut the front door: Scientists have finally found the perfect breasts. No, they weren't hiding in the Amazon or roving solo across the Sahara (although we have no doubt there are women in both the Amazon and the Sahara who have magnificent mammaries); it turns out these perfect breasts were hiding in a plastic surgeon's office this whole time! Now, before you get all worked up, the American Society of Plastic Surgeons (ASPS) would like you to know that the super-fake looking plastic breasts of yore are not actually what people think are most attractive now. According to a study published in the Journal of Plastic and Reconstructive Surgery—which involved asking over 1,300 people to look at pictures of naked boobies and rank them by hotness (stop laughing, this is serious research!)—people preferred a more "real" and "normal" look from their silicone, with the ideal breast shape having a 45:55 ratio. People said the best chests have 45 percent of the fullness above the nipple line and 55 percent of the fullness below, in a slightly teardrop shape. Researchers noted this preference remained consistent across gender, racial, and ethnic groups with the 45:55 ratio favored by 87 percent of women in their 30s, 90 percent of men, and 94 percent of plastic surgeons.
Men need to know that breast cancer is not limited to women. Possible symptoms of breast cancer to watch for include: A lump or swelling, which is usually (but not always) painless Skin dimpling or puckering Nipple retraction (turning inward) Redness or scaling of the nipple or breast skin Discharge from the nipple Sometimes a breast cancer can spread to lymph nodes under the arm or around the collar bone and cause a lump or swelling there, even before the original tumor in the breast tissue is large enough to be felt. These changes aren't always caused by cancer. For example, most breast lumps in men are caused by gynecomastia (a harmless enlargement of breast tissue). Still, if you notice any breast changes, you should see a health care professional as soon as possible.

The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. It can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy, the most common form of Guillain-Barré syndrome. Signs and symptoms CIDP typically starts insidiously and evolves slowly, in either a slowly progressive or a relapsing manner, with partial or complete recovery between recurrences; periods of worsening and improvement usually last weeks or months. Most experts consider the necessary duration of symptoms to be greater than 8 weeks for the diagnosis of CIDP to be made. Symptoms reported include the following: Preceding infection (infrequent) Initial limb weakness, both proximal and distal Sensory symptoms (eg, tingling and numbness of hands and feet) Motor symptoms (usually predominant) In about 16% of patients, a relatively acute or subacute onset of symptoms In children, usually a more precipitous onset of symptoms Symptoms of autonomic system dysfunction (eg, orthostatic dizziness) Pertinent physical findings are limited to the nervous system, except when the condition is associated with other diseases. Such findings may include the following. Signs of cranial nerve (CN) involvement (eg, facial muscle paralysis or diplopia) Gait abnormalities Motor deficits (eg, symmetric weakness of both proximal and distal muscles in upper and lower extremities) Diminished or absent deep tendon reflexes Sensory deficits (typically in stocking-glove distribution) Impaired coordination See Clinical Presentation for more detail. Diagnosis Laboratory studies that may be helpful include the following: Cerebrospinal fluid analysis: Elevated protein levels are common (80% of patients); 10% of patients also have mild lymphocytic pleocytosis and increased gamma globulin Complete blood count (CBC), erythrocyte sedimentation rate (ESR), antinuclear antibody (ANA) level, biochemistry profile, and serum and urine immunoelectrophoresis (to exclude associated systemic disorders) In certain instances, genetic testing Other tests and procedures that may be warranted are as follows: MRI of the spine with gadolinium enhancement Electromyography (EMG) is a critical test to determine whether the disorder is truly a peripheral neuropathy and whether the neuropathy is demyelinating Peripheral (sural) nerve biopsy (see the image below): This is considered when the diagnosis is not completely clear, when other causes cannot be excluded, or when profound axonal involvement is observed on EMG; biopsy was once commonly recommended for most patients before immunosuppressive therapy, but current guidelines no longer recommend it
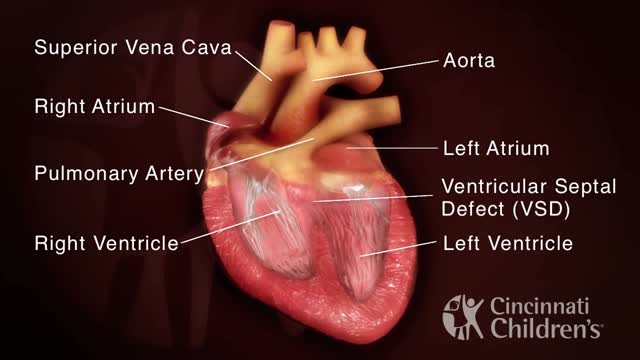
Tetralogy of Fallot (teh-TRAL-uh-jee of fuh-LOW) is a rare condition caused by a combination of four heart defects that are present at birth. These defects, which affect the structure of the heart, cause oxygen-poor blood to flow out of the heart and to the rest of the body. Infants and children with tetralogy of Fallot usually have blue-tinged skin because their blood doesn't carry enough oxygen. Tetralogy of Fallot is often diagnosed during infancy or soon after. However, tetralogy of Fallot might not be detected until later in life, depending on the severity of the defects and symptoms. With early diagnosis followed by appropriate surgical treatment, most children who have tetralogy of Fallot live relatively normal lives, though they'll need regular medical care and might have restrictions on exercise.

Interstitial cystitis is a clinical syndrome characterized by daytime and nighttime urinary frequency, urgency, and pelvic pain of unknown etiology. Interstitial cystitis has no clear etiology or pathophysiology, and diagnostic criteria for the syndrome remain undefined. Despite considerable research, universally effective treatments do not exist; therapy usually consists of various supportive, behavioral, and pharmacologic measures. Surgical intervention is rarely indicated. The International Continence Society has coined the term painful bladder syndrome (suprapubic pain with bladder filling associated with increased daytime and nighttime frequency, in the absence of proven urinary infection or other obvious pathology) and reserves the diagnosis of interstitial cystitis for patients with characteristic cystoscopic and histologic features of the condition.[1] An international consensus panel was able to generally agree on the following definition of interstitial cystitis/bladder pain syndrome (IC/BPS): unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder and associated with lower urinary tract symptoms of more than 6 weeks duration, in the absence of infection or other identifiable causes. American Urological Association (AUA) guidelines published in 2011 and amended in 2014 use an evidence-based approach to provide a clinical framework for the diagnosis and management of this condition.[2, 3, 4] In 1887, Skene initially described a condition characterized by inflammation that destroyed the urinary bladder "mucous membrane partly or wholly and extended to the muscular parietes." Guy Hunner popularized the disease with the description of characteristic bladder wall ulcers in association with a symptom complex of chronic bladder inflammation.[5] The first comprehensive epidemiologic description of interstitial cystitis is credited to Hand, who in 1949 described the widespread, small, submucosal bladder hemorrhages and the significant variation in bladder capacity characteristic of the condition. Despite years of intensive research, there are no specific clinical or urinary markers currently clinically available; no absolutely specific radiographic, laboratory, or serologic findings; and no biopsy patterns that are pathognomonic for interstitial cystitis. Some research suggests that the following may all play a role in the disease pathophysiology: (1) pelvic floor dyfunction, (2) dysregulated immune or inflammatory signals, (3) neural hypersensitivity, and (4) disruption of the proteoglycan/glycosaminoglycan (GAG) layer.[6] Interstitial cystitis, howerver, remains a diagnosis of exclusion (see Presentation, DDx, and Workup.) Intensive study has been done to attempt to identify biomarkers for IC/BPS. Some interesting studies have shown that bladder nitric oxide is an accurate marker for Hunner lesions, but these are not present in all patients, and the test requires specific equipment, which has limited widespread clinical use.[7] Differences in levels of cytokines and chemokines, specifically CXCL-10, have shown some ability to differentiate patients with and without Hunner lesions.[8] Other studies of ulcerative IC/BPS have shown that numerous other cytokines and chemokines are up-regulated as well, heralding a possible urinary test to identify patients.[9] An additional substance shown to be up-regulated in IC/BPS patients is antiproliferative factor (APF). This small 8–amino-acid peptide has been associated with suppression of cell growth, increases in transcellular permeability, and lowering of levels of proteins that form intercellular junctional complexes. It is synthesized and secreted from bladder epithelial cells from patients with IC/BPS and may play a key role in pathophysiology.[10] In vitro studies have shown that removal of APF from cell culture media restored cell proliferation and membrane integrity.[11] Studies have also suggested APF in the therapeutic effect of hydrodistension in patients with IC/BPS, although further confirmatory studies are necessary.[12] The most important element in treating patients with interstitial cystitis is education and emotional support. Periodic exacerbations are managed as they occur because no long-term therapy has been shown to prevent or delay recurrent episodes. Therefore, the purpose of treatment is to palliate and alleviate symptoms. Because no discrete pathognomonic pathologic criteria exist for assessing and monitoring disease severity, indications and goals for treatment are based on the degree of patient symptoms. Assessing patient response to treatment is also complicated because of the subjective nature of symptoms; the waxing and waning nature of symptoms without treatment; and the lack of objective serologic, physical, or histopathologic findings. Conservative measures and oral or intravesical treatments are considered first-line treatment. (See Treatment.)
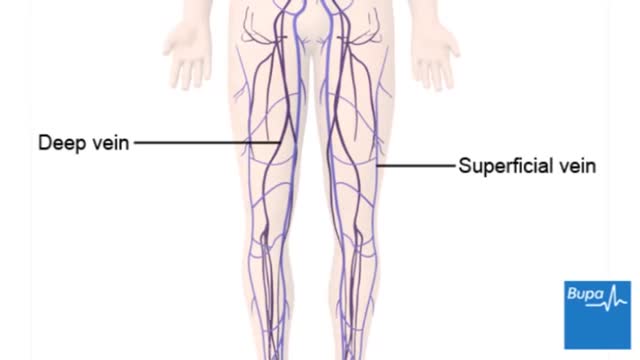
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs. Deep vein thrombosis can cause leg pain or swelling, but may occur without any symptoms. Deep vein thrombosis can develop if you have certain medical conditions that affect how your blood clots. Deep vein thrombosis can also happen if you don't move for a long time, such as after surgery, following an accident, or when you are confined to a hospital or nursing home bed.

Download Clash of Clans for free for mobile devices. http://supr.cl/ThisArmy
I don't know you, BigBuffetBoy85
But if you think you can humiliate me and take my gold, think again.
Oh, I am coming for you with lots of Barbarians and Dragons. I can't wait to destroy your village, while you beg for mercy, but you will get no mercy. I will have my revenge.