Cardiology
Heart Attack vs Cardiac Arrest vs Stroke
Cardiac arrest is the abrupt loss of heart function in a person who may or may not have diagnosed heart disease. The time and mode of death are unexpected. It occurs instantly or shortly after symptoms appear. Each year, more than 350,000 emergency medical services-assessed out-of-hospital cardiac arrests occur in the United States
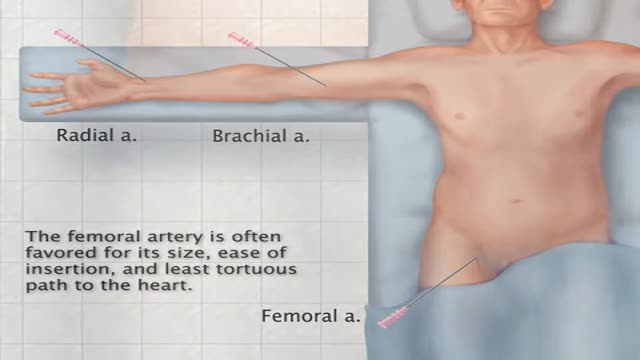
The preferred route of access for temporary transvenous pacing is the internal jugular vein followed by subclavian and femoral veins. However, all the major venous access sites (internal and external jugular, subclavian, brachial, femoral) have been used and each is associated with particular problems.
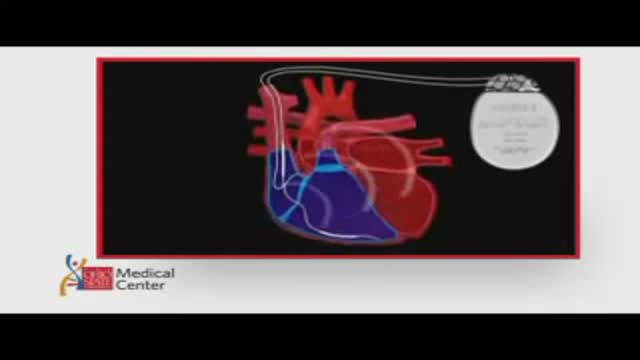
ICDs are useful in preventing sudden death in patients with known, sustained ventricular tachycardia or fibrillation. Studies have shown ICDs to have a role in preventing cardiac arrest in high-risk patients who haven't had, but are at risk for, life-threatening ventricular arrhythmias. View an animation of an ICD. Newer-generation ICDs may have a dual function which includes the ability to serve as a pacemaker. The pacemaker feature would stimulate the heart to beat if the heart rate is detected to be too slow. What is an Implantable Cardioverter Defibrillator (ICD)? An ICD is a battery-powered device placed under the skin that keeps track of your heart rate. Thin wires connect the ICD to your heart. If an abnormal heart rhythm is detected the device will deliver an electric shock to restore a normal heartbeat if your heart is beating chaotically and much too fast. ICDs have been very useful in preventing sudden death in patients with known, sustained ventricular tachycardia or fibrillation. Studies have shown that they may have a role in preventing cardiac arrest in high-risk patients who haven't had, but are at risk for, life-threatening ventricular arrhythmias.
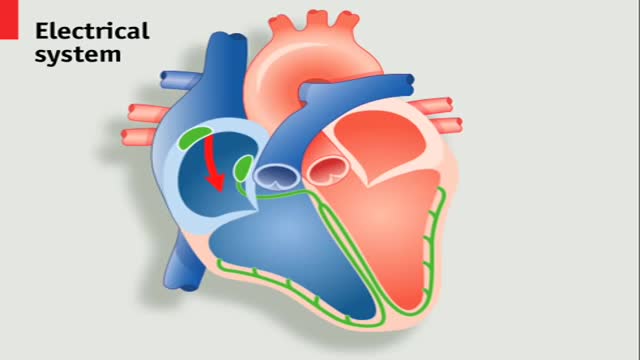
A pacemaker is a small device that's placed in the chest or abdomen to help control abnormal heart rhythms. This device uses electrical pulses to prompt the heart to beat at a normal rate. Pacemakers are used to treat arrhythmias (ah-RITH-me-ahs). Arrhythmias are problems with the rate or rhythm of the heartbeat.Feb 28, 2012
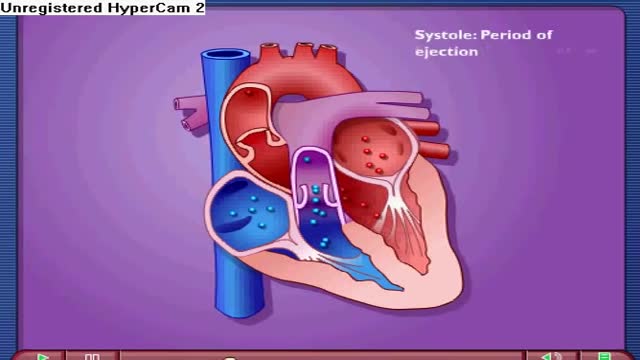
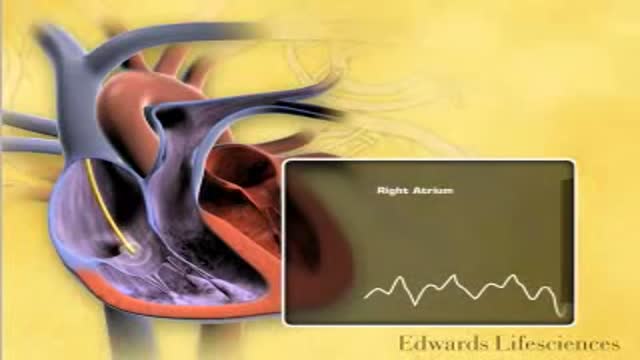
Near the end of diastole, the ventricles nearly fill with blood, and then the atria contract, adding even more volume to the ventricles. The volume of blood in the ventricles at the end of diastole is referred to as the end-diastolic volume. The other phase of the cardiac cycle is called systole.
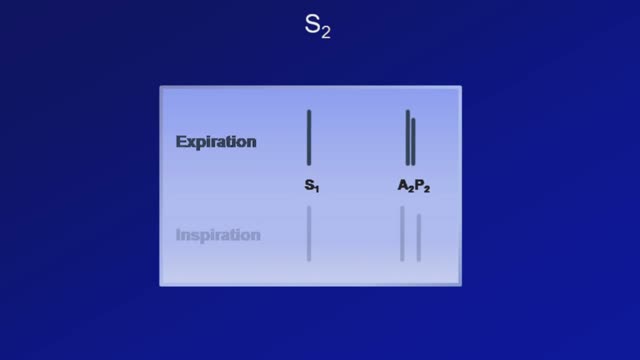
Heart sounds are the noises generated by the beating heart and the resultant flow of blood through it. Specifically, the sounds reflect the turbulence created when the heart valves snap shut. In cardiac auscultation, an examiner may use a stethoscope to listen for these unique and distinct sounds that provide important auditory data regarding the condition of the heart. In healthy adults, there are two normal heart sounds often described as a lub and a dub (or dup), that occur in sequence with each heartbeat. These are the first heart sound (S1) and second heart sound (S2), produced by the closing of the atrioventricular valves and semilunar valves, respectively. In addition to these normal sounds, a variety of other sounds may be present including heart murmurs, adventitious sounds, and gallop rhythms S3 and S4.
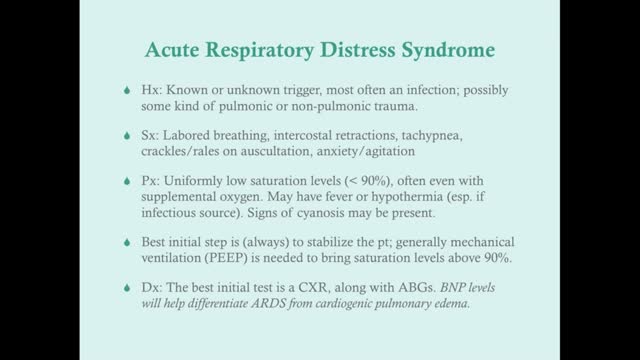
Acute respiratory distress syndrome (ARDS) occurs when fluid builds up in the tiny, elastic air sacs (alveoli) in your lungs. More fluid in your lungs means less oxygen can reach your bloodstream. This deprives your organs of the oxygen they need to function. ARDS typically occurs in people who are already critically ill or who have significant injuries. Severe shortness of breath — the main symptom of ARDS — usually develops within a few hours to a few days after the original disease or trauma. Many people who develop ARDS don't survive. The risk of death increases with age and severity of illness. Of the people who do survive ARDS, some recover completely while others experience lasting damage to their lungs.
Finding a donor heart can be difficult. The heart must be donated by someone who is brain-dead but is still on life support. The donor heart must be matched as closely as possible to your tissue type to reduce the chance that your body will reject it. You are put into a deep sleep with general anesthesia, and a cut is made through the breastbone. Your blood flows through a heart-lung bypass machine while the surgeon works on your heart. This machine does the work of your heart and lungs while they are stopped, and supplies your body with blood and oxygen. Your diseased heart is removed and the donor heart is stitched in place. The heart-lung machine is then disconnected. Blood flows through the transplanted heart, which takes over supplying your body with blood and oxygen. Tubes are inserted to drain air, fluid, and blood out of the chest for several days, and to allow the lungs to fully re-expand.
An abdominal aortic aneurysm is an enlarged area in the lower part of the aorta, the major blood vessel that supplies blood to the body. The aorta, about the thickness of a garden hose, runs from your heart through the center of your chest and abdomen. Because the aorta is the body's main supplier of blood, a ruptured abdominal aortic aneurysm can cause life-threatening bleeding. Depending on the size and the rate at which your abdominal aortic aneurysm is growing, treatment may vary from watchful waiting to emergency surgery. Once an abdominal aortic aneurysm is found, doctors will closely monitor it so that surgery can be planned if it's necessary. Emergency surgery for a ruptured abdominal aortic aneurysm can be risky.
Transfemoral Cardiac Catheterization
Transradial Cardiac Catheterization
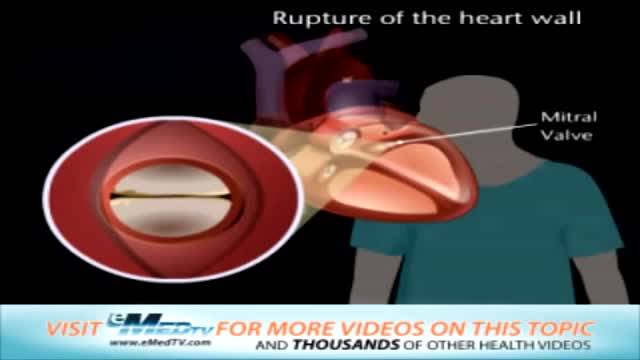
Mitral valve surgery is surgery to either repair or replace the mitral valve in your heart. Blood flows from the lungs and enters a pumping chamber of the heart called the left atrium. The blood then flows into the final pumping chamber of the heart called the left ventricle. The mitral valve is located between these two chambers. It makes sure that the blood keeps moving forward through the heart. You may need surgery on your mitral valve if: The mitral valve is hardened (calcified). This prevents blood from moving forward through the valve. The mitral valve is too loose. Blood tends to flows backward when this occurs. Minimally invasive mitral valve surgery is done through several small cuts. Another type of operation, open mitral valve surgery requires a larger cut.
Rupture of the Heart Wall and Mitral Valve Replacement
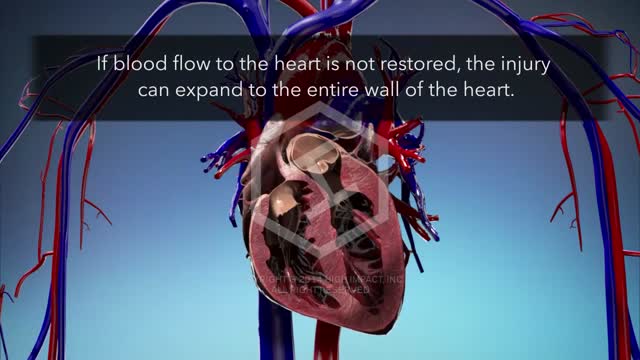
Blunt injury to the heart ranges from contusion to disruption. This report comprises 14 patients seen during a 6-year period with cardiac rupture secondary to blunt trauma. Eight patients were injured in automobile accidents, two patients were injured in auto-pedestrian accidents, two were kicked in the chest by ungulates, and two sustained falls. Cardiac tamponade was suspected in ten patients. Five patients presented with prehospital cardiac arrest or arrested shortly after arrival. All underwent emergency department thoracotomy without survival. Two patients expired in the operating room during attempted cardiac repair; both had significant extracardiac injury. Seven patients survived, three had right atrial injuries, three had right ventricular injuries, and one had a left atrial injury. Cardiopulmonary bypass was not required for repair of the surviving patients. There were no significant complications from the cardiac repair.
Myocardial rupture occurs in the setting of acute myocardial infarction (AMI), blunt and penetrating cardiac trauma, primary cardiac infection, primary and secondary cardiac tumors, infiltrative diseases of the heart, and aortic dissection. Myocardial rupture (or perforation) may also occur iatrogenically during percutaneous cardiac procedures (including device implantation) or open heart surgery (particularly valve replacement). Recently, myocardial rupture has been reported in the setting of stress cardiomyopathy (Takotsubo or regional ventricular ballooning syndrome). The clinical presentation of myocardial rupture depends on the mechanism and site of injury and the hemodynamic effects of the rupture. Mortality is extremely high unless early diagnosis is made and urgent surgical intervention is provided.
Pulmonary capillary wedge pressure (PCWP) provides an indirect estimate of left atrial pressure (LAP). Although left ventricular pressure can be directly measured by placing a catheter within the left ventricle, it is not feasible to advance this catheter back into the left atrium. LAP can be measured by placing a special catheter into the right atrium then punching through the interatrial septum; however, for obvious reasons, this is not usually performed because of damage to the septum and potential harm to the patient.
Pulmonary edema is almost always treated in the emergency room or hospital. You may need to be in an intensive care unit (ICU). Oxygen is given through a face mask or tiny plastic tubes are placed in the nose. A breathing tube may be placed into the windpipe (trachea) so you can be connected to a breathing machine (ventilator) if you cannot breathe well on your own. The cause of edema should be identified and treated quickly. For example, if a heart attack has caused the condition, it must be treated right away. Medicines that may be used include: Diuretics that remove excess fluid from the body Medicines that strengthen the heart muscle, control the heartbeat, or relieve pressure on the heart
Pulmonary edema Email this page to a friend Email this page to a friend Facebook Twitter Google+ Pulmonary edema is an abnormal buildup of fluid in the lungs. This buildup of fluid leads to shortness of breath. Causes Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs. As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs. This fluid reduces normal oxygen movement through the lungs. These two factors combine to cause shortness of breath.
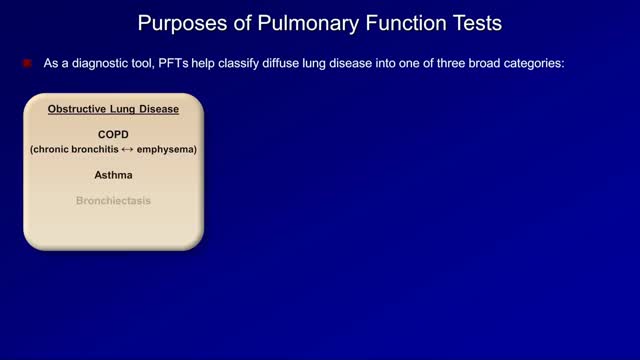
Pulmonary function tests are a broad range of tests that measure how well the lungs take in and exhale air and how efficiently they transfer oxygen into the blood. Spirometry measures how well the lungs exhale.