Cardiology
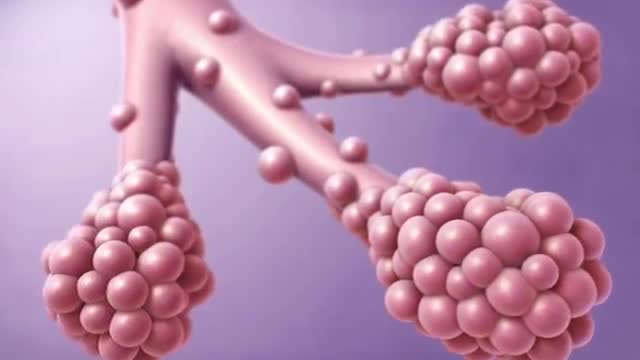
Idiopathic pulmonary fibrosis (IPF) is defined as a specific form of chronic, progressive fibrosing interstitial pneumonia of unknown cause, primarily occurring in older adults, limited to the lungs, and associated with the histopathologic and/or radiologic pattern of usual interstitial pneumonia (UIP).[1] Signs and symptoms The clinical symptoms of idiopathic pulmonary fibrosis are nonspecific and can be shared with many pulmonary and cardiac diseases. Most patients present with a gradual onset (often >6 mo) of exertional dyspnea and/or a nonproductive cough. Approximately 5% of patients have no presenting symptoms when idiopathic pulmonary fibrosis is serendipitously diagnosed.
Tuberculosis (TB) is a disease caused by bacteria called Mycobacterium tuberculosis. The bacteria usually attack the lungs, but they can also damage other parts of the body. TB spreads through the air when a person with TB of the lungs or throat coughs, sneezes, or talks. If you have been exposed, you should go to your doctor for tests. You are more likely to get TB if you have a weak immune system. Symptoms of TB in the lungs may include A bad cough that lasts 3 weeks or longer Weight loss Loss of appetite Coughing up blood or mucus Weakness or fatigue Fever Night sweats
The Most Important Heart Tests for Those Being Evaluated for Heart Disease To be sure, there are a number of good cardiac screening tests that should be included in any comprehensive preventive and diagnostic cardiac assessment. From all the options available in the massive cardiologist toolbox to assess basic heart function, these are the tests I recommend: Electrocardiogram (EKG) Echocardiogram Exercise/Nuclear Stress Test Holter Monitoring BNP Test
Use lifestyle changes Quit smokingQuit smoking. Avoid secondhand smoke too. ... Exercise . There are lots of ways that exercise boosts your heart health. ... Eat a heart-healthy diet . The way you eat can help you control your cholesterol and blood pressure. Stay at a healthy weight .
An increased prevalence of cardiovascular disease (CVD) has been found in women of childbearing age,[1] with the presence of CVD in pregnant women posing a difficult clinical scenario in which the responsibility of the treating physician extends to the unborn fetus. Profound changes occur in the maternal circulation that have the potential to adversely affect maternal and fetal health, especially in the presence of underlying heart conditions. Up to 4% of pregnancies may have cardiovascular complications despite no known prior disease. The European Society of Cardiology has published guidelines on the management of cardiovascular disease during pregnancy.[
each type of heart problem requires different treatment but may share similar warning signs. It is important to see your doctor so that you can receive a correct diagnosis and prompt treatment. Learn to recognize the symptoms that may signal heart disease. Call your doctor if you begin to have new symptoms or if they become more frequent or severe. Symptoms of Coronary Artery Disease The most common symptom of coronary artery disease is angina, or chest pain. Angina can be described as a discomfort, heaviness, pressure, aching, burning, fullness, squeezing, or painful feeling in your chest. It can be mistaken for indigestion or heartburn. Angina may also be felt in the shoulders, arms, neck, throat, jaw, or back. Other symptoms of coronary artery disease include: Shortness of breath Palpitations (irregular heart beats, or a "flip-flop" feeling in your chest) A faster heartbeat Weakness or dizziness Nausea Sweating
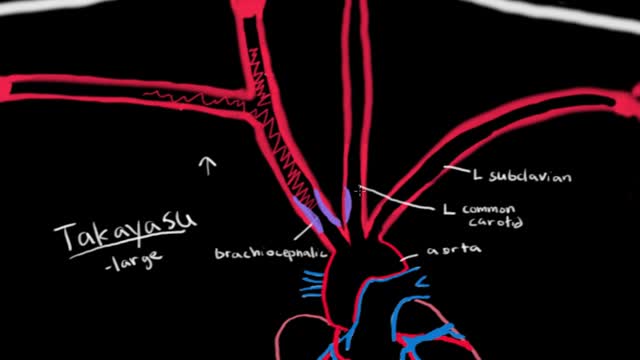
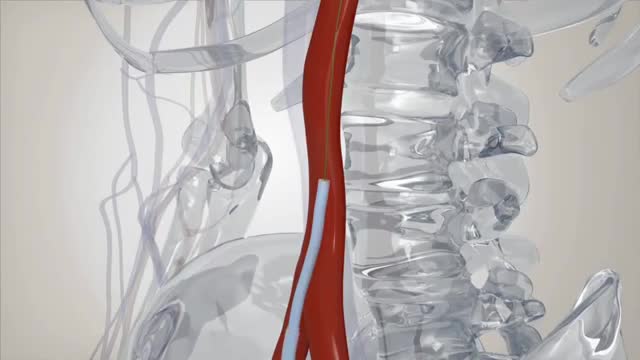
Takayasu's arteritis (tah-kah-YAH-sooz ahr-tuh-RIE-tis) is a rare type of vasculitis, a group of disorders that cause blood vessel inflammation. In Takayasu's arteritis, the inflammation damages the aorta — the large artery that carries blood from your heart to the rest of your body — and its main branches. The disease can lead to blockages or narrowed arteries (stenosis) or abnormally dilated arteries (aneurysms). Takayasu's arteritis can also lead to arm or chest pain and high blood pressure and eventually to heart failure or stroke. If you don't have symptoms, you may not need treatment. Or you may need medications to control the inflammation in the arteries and prevent complications. But even with treatment, relapses are common.
Giant cell arteritis is an inflammation of the lining of arteries. Most often, it affects the arteries in your head, especially those in your temples. For this reason, giant cell arteritis is sometimes called temporal arteritis. Giant cell arteritis frequently causes headaches, scalp tenderness, jaw pain and vision problems. If left untreated, it can lead to stroke or blindness. Prompt treatment with corticosteroid medications usually relieves symptoms of giant cell arteritis and may prevent loss of vision. You'll likely begin to feel better within days of starting treatment. But even with treatment, relapses are common. You'll need to visit your doctor regularly for checkups and treatment of any side effects from taking corticosteroids.
Polyarteritis nodosa Email this page to a friend Email this page to a friend Facebook Twitter Google+ Polyarteritis nodosa is a serious blood vessel disease. The small and medium-sized arteries become swollen and damaged. Causes Arteries are the blood vessels that carry oxygen-rich blood to organs and tissues. The cause of polyarteritis nodosa is unknown. The condition occurs when certain immune cells attack the affected arteries. More adults than children get this disease. The tissues that are fed by the affected arteries do not get the oxygen and nourishment they need. Damage occurs as a result. People with active hepatitis B or hepatitis C may develop this disease.
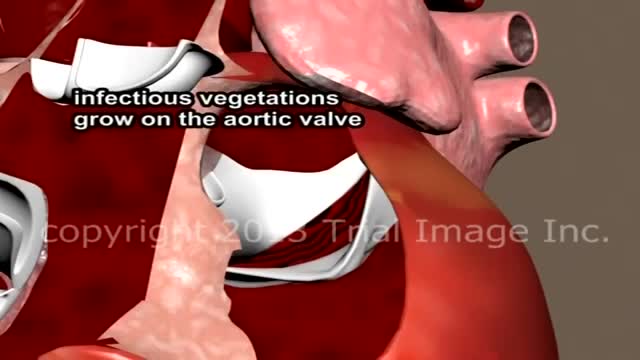
Endocarditis is an infection of the inner lining of your heart (endocardium). Endocarditis generally occurs when bacteria or other germs from another part of your body, such as your mouth, spread through your bloodstream and attach to damaged areas in your heart. Left untreated, endocarditis can damage or destroy your heart valves and can lead to life-threatening complications. Treatments for endocarditis include antibiotics and, in certain cases, surgery. Endocarditis is uncommon in people with healthy hearts. People at greatest risk of endocarditis have damaged heart valves, artificial heart valves or other heart defects.
Thoracic outlet syndrome is a disorders that occur when blood vessels or nerves in the space between your collarbone and your first rib (thoracic outlet) are compressed. This can cause pain in your shoulders and neck and numbness in your fingers. Common causes of thoracic outlet syndrome include physical trauma from a car accident, repetitive injuries from job- or sports-related activities, certain anatomical defects (such as having an extra rib), and pregnancy. Sometimes doctors can't determine the cause of thoracic outlet syndrome. Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures. Most people improve with these approaches. In some cases, however, your doctor may recommend surgery.
Thoracic outlet syndrome is a group of disorders that occur when blood vessels or nerves in the space between your collarbone and your first rib (thoracic outlet) are compressed. This can cause pain in your shoulders and neck and numbness in your fingers. Common causes of thoracic outlet syndrome include physical trauma from a car accident, repetitive injuries from job- or sports-related activities, certain anatomical defects (such as having an extra rib), and pregnancy. Sometimes doctors can't determine the cause of thoracic outlet syndrome. Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures. Most people improve with these approaches. In some cases, however, your doctor may recommend surgery.
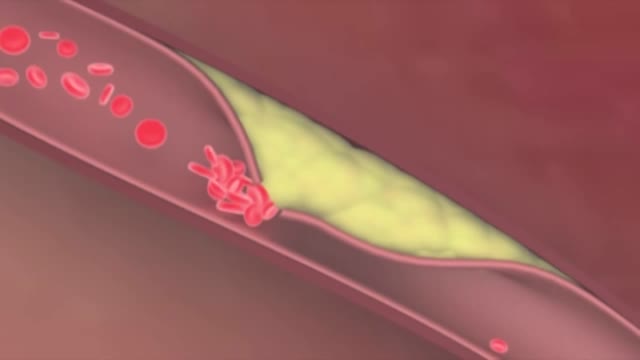
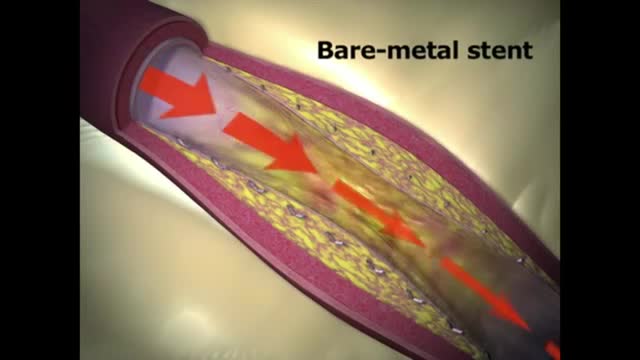
Peripheral artery disease (P.A.D.) is a disease in which plaque builds up in the arteries that carry blood to your head, organs, and limbs. Plaque is made up of fat, cholesterol, calcium, fibrous tissue, and other substances in the blood. When plaque builds up in the body's arteries, the condition is called atherosclerosis. Over time, plaque can harden and narrow the arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body. P.A.D. usually affects the arteries in the legs, but it also can affect the arteries that carry blood from your heart to your head, arms, kidneys, and stomach. This article focuses on P.A.D. that affects blood flow to the legs.
An arteriovenous fistula is an abnormal connection or passageway between an artery and a vein. It may be congenital, surgically created for hemodialysis treatments, or acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm.
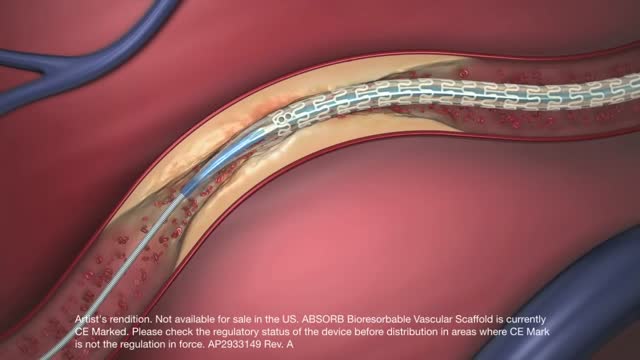
If you have a blocked artery, your doctor may need to open the blockage and restore blood flow using a small mesh tube called a stent. The stent is inserted in your artery during an angioplasty procedure. Until now, stents were permanent. Now there is a fully dissolving stent available to treat blockages.
INDICATIONS The Absorb GT1 Bioresorbable Vascular Scaffold (BVS) is a temporary scaffold that will fully resorb over time and is indicated for improving coronary luminal diameter in patients with ischemic heart disease due to de novo native coronary artery lesions (length ≤ 24 mm) with a reference vessel diameter of ≥ 2.5 mm and ≤ 3.75 mm WHAT ARE THE POTENTIAL RISKS AND COMPLICATIONS? Treatment options for CAD have become increasingly common but, as with any invasive procedure, there are potential risk factors and complications. Serious complications do not occur often, and research is ongoing to make these procedures even safer and more effective. The risk of complications from percutaneous treatment methods may be higher for individuals: 75 years of age and older Who are women Who have kidney disease or diabetes Who have serious heart disease Who have had prior cardiac interventions
When the arteries in your heart become blocked, the condition is called coronary artery disease. It can be a serious condition if not treated. Coronary artery disease puts you at risk for a heart attack. Be sure you pay attention to your symptoms and manage your heart health risks.
Aortic valve replacement is a procedure in which a patient's failing aortic valve is replaced with an artificial heart valve. The aortic valve can be affected by a range of diseases; the valve can either become leaky (aortic insufficiency / regurgitation) or partially blocked (aortic stenosis).
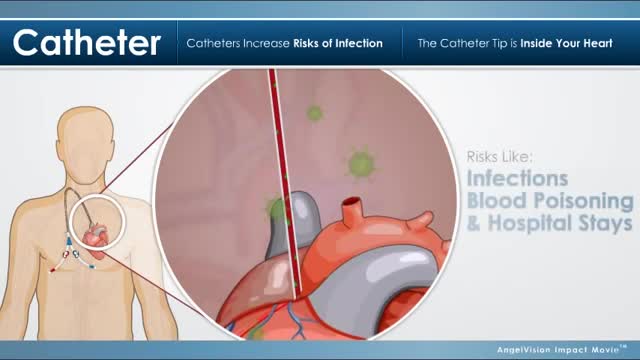
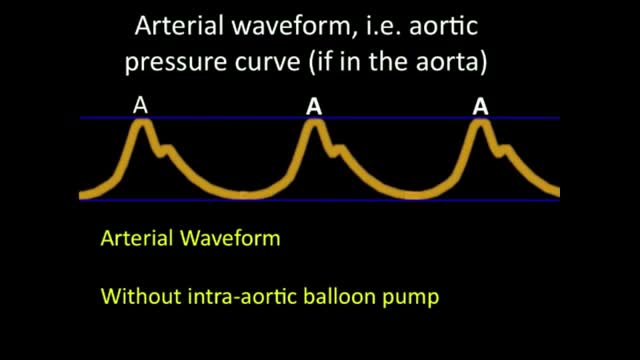
An intra-aortic balloon pump (IABP) is a mechanical device that helps the heart pump blood. This device is inserted into the aorta, the body's largest artery. It is a long, thin tube called a catheter with a balloon on the end of it. If you are hospitalized, your doctor may insert an IABP. Your doctor will numb an area of your leg and thread the IABP through the femoral artery in your leg into your aorta. He or she then positions the IABP at the center of your aorta, below your heart. The doctor will use an X-ray machine during this procedure to help accurately position the IABP. Why is it used? An IABP might be used to stabilize a person who is in the hospital for acute mitral valve regurgitation or severe heart failure. An IABP is only used for a short period of time (hours to days). A long-term treatment will likely be needed, such as valve surgery or the insertion of a left ventricular assist device (LVAD).
Rapid Algorithm Review Ventricular Fibrillation