Cardiology
Atrial flutter is a type of abnormal heart rate, or arrhythmia. It occurs when the upper chambers of your heart beat too fast. When the chambers in the top of your heart (atria) beat faster than the bottom ones (ventricles), it complicates your heart rhythm
Atrial flutter (AFL) is a type of abnormal heart rate, or arrhythmia. It occurs when the upper chambers of your heart beat too fast. When the chambers in the top of your heart (atria) beat faster than the bottom ones (ventricles), it complicates your heart rhythm
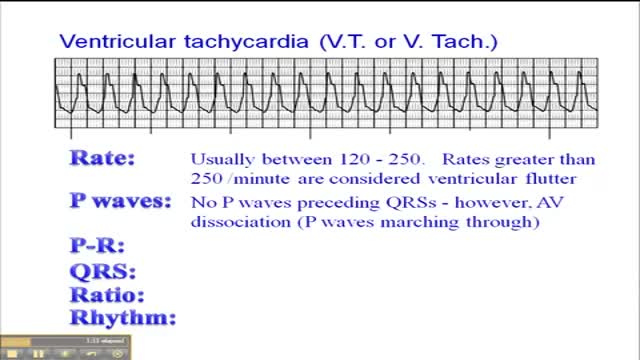
Ventricular tachycardia is a type of heart rhythm disorder (arrhythmia) in which the lower chambers of your heart (ventricles) beat very quickly because of a problem in your heart's electrical system. In ventricular tachycardia, your heart may not be able to pump enough blood to your body and lungs because the chambers are beating so fast that they don't have time to properly fill. Ventricular tachycardia may be brief — lasting for just seconds and often not causing symptoms — or it can last for much longer, and you can develop symptoms such as dizziness or lightheadedness, or you can even pass out. This condition usually occurs in people with other heart conditions, such as coronary artery disease, cardiomyopathy and some types of valvular heart disease. Ventricular tachycardia may lead to a condition in which your lower heart chambers quiver (ventricular fibrillation), which may cause your heart to stop (sudden cardiac arrest) and lead to death if not treated immediately. Ventricular tachycardia can also cause your heart to stop, especially if the heart is beating very quickly, if it's lasting for a long period, and if you have an underlying heart condition.
Ventricular fibrillation is a heart rhythm problem that occurs when the heart beats with rapid, erratic electrical impulses. This causes pumping chambers in your heart (the ventricles) to quiver uselessly, instead of pumping blood. Sometimes triggered by a heart attack, ventricular fibrillation causes your blood pressure to plummet, cutting off blood supply to your vital organs. Ventricular fibrillation, an emergency that requires immediate medical attention, causes the person to collapse within seconds. It's the most frequent cause of sudden cardiac death. Emergency treatment includes cardiopulmonary resuscitation (CPR) and shocks to the heart with a device called a defibrillator. Treatments for those at risk of ventricular fibrillation include medications and implantable devices that can restore a normal heart rhythm.
AFib is caused by abnormal electrical impulses in the atria, which are the upper chambers of the heart. The result is a rapid and irregular pumping of blood through the atria. These chambers fibrillate, or quiver, rapidly.
Atrial fibrillation (also called AFib or AF) is a quivering or irregular heartbeat (arrhythmia) that can lead to blood clots, stroke, heart failure and other heart-related complications. Some people refer to AF as a quivering heart. An estimated 2.7 million Americans are living with AF.
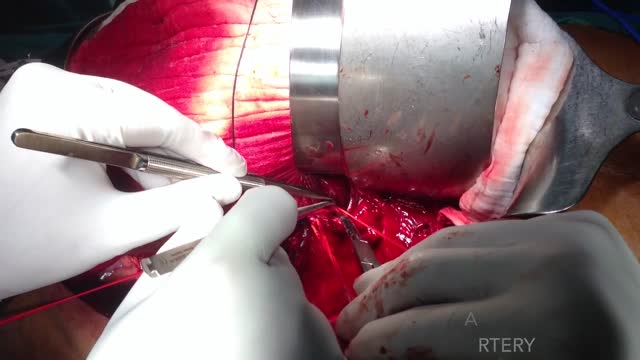
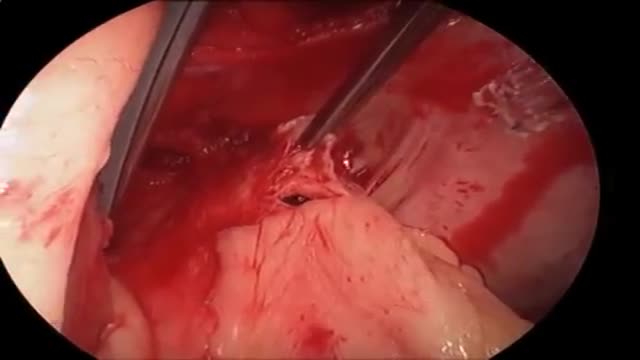
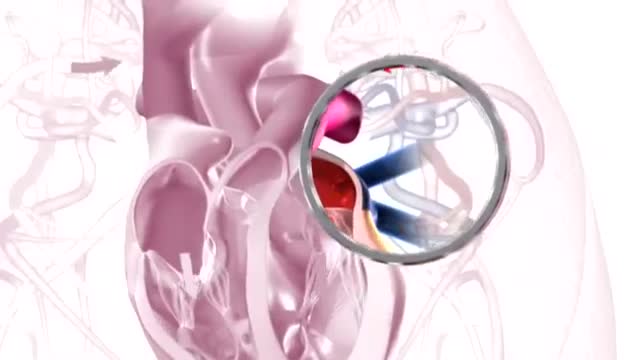
Catheter ablation is a minimally invasive procedure to treat atrial fibrillation. It can relieve symptoms and improve quality of life. During an ablation, the doctor destroys tiny areas in the heart that are firing off abnormal electrical impulses and causing atrial fibrillation. You will be given medicine to help you relax. A local anesthetic will numb the site where the catheter is inserted. Sometimes, general anesthesia is used. The procedure is done in a hospital where you can be watched carefully. Thin, flexible wires called catheters are inserted into a vein, typically in the groin or neck, and threaded up into the heart. There is an electrode at the tip of the wires. The electrode sends out radio waves that create heat. This heat destroys the heart tissue that causes atrial fibrillation or the heart tissue that keeps it happening. Another option is to use freezing cold to destroy the heart tissue. Sometimes, abnormal impulses come from inside a pulmonary vein and cause atrial fibrillation. (The pulmonary veins bring blood back from the lungs to the heart.) Catheter ablation in a pulmonary vein can block these impulses and keep atrial fibrillation from happening. View a slideshow of catheter ablation to see how the heart's electrical system works, how atrial fibrillation happens, and how ablation is done. Atrial Fibrillation: Should I Have Catheter Ablation? AV node ablation AV node ablation is a slightly different type of ablation procedure for atrial fibrillation. AV node ablation can control symptoms of atrial fibrillation in some people. It might be right for you if medicine has not worked, catheter ablation did not stop your atrial fibrillation, or you cannot have catheter ablation. With AV node ablation, the entire atrioventricular (AV) node is destroyed. After the AV node is destroyed, it can no longer send impulses to the lower chambers of the heart (ventricles). This controls atrial fibrillation symptoms. After AV node ablation, a permanent pacemaker is needed to regulate your heart rhythm. Nodal ablation can control your heart rate and reduce your symptoms, but it does not prevent or cure atrial fibrillation. AV node ablation helps about 9 out of 10 people.1 The procedure has a low risk of serious problems.2 View a slideshow of AV node ablation to see how the heart's electrical system works, how atrial fibrillation happens, and how AV node ablation is performed.
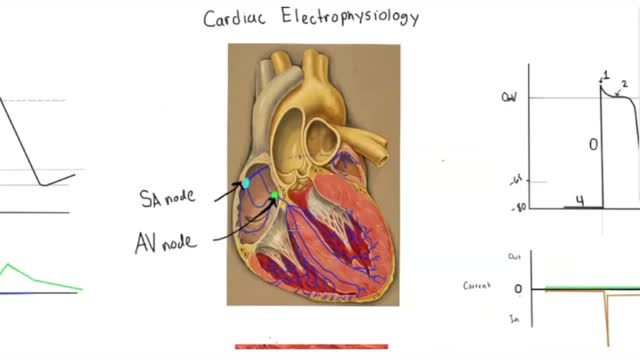
Electrophysiology studies test the electrical activity of your heart to find where an arrhythmia (abnormal heartbeat) is coming from. These results can help you and your doctor decide whether you need medicine, a pacemaker, an implantable cardioverter defibrillator (ICD), cardiac ablation or surgery.
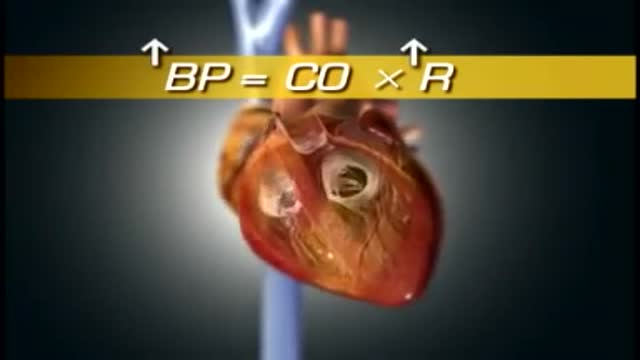
High blood pressure is a common condition in which the long-term force of the blood against your artery walls is high enough that it may eventually cause health problems, such as heart disease. Blood pressure is determined both by the amount of blood your heart pumps and the amount of resistance to blood flow in your arteries. The more blood your heart pumps and the narrower your arteries, the higher your blood pressure. You can have high blood pressure (hypertension) for years without any symptoms. Even without symptoms, damage to blood vessels and your heart continues and can be detected. Uncontrolled high blood pressure increases your risk of serious health problems, including heart attack and stroke. High blood pressure generally develops over many years, and it affects nearly everyone eventually. Fortunately, high blood pressure can be easily detected. And once you know you have high blood pressure, you can work with your doctor to control it.
Hypertensive emergencies encompass a spectrum of clinical presentations in which uncontrolled blood pressures lead to progressive or impending end-organ dysfunction. In these conditions, the BP should be lowered aggressively over minutes to hours. Neurologic end-organ damage due to uncontrolled BP may include hypertensive encephalopathy, cerebral vascular accident/cerebral infarction, subarachnoid hemorrhage, and/or intracranial hemorrhage.[1] Cardiovascular end-organ damage may include myocardial ischemia/infarction, acute left ventricular dysfunction, acute pulmonary edema, and/or aortic dissection. Other organ systems may also be affected by uncontrolled hypertension, which may lead to acute renal failure/insufficiency, retinopathy, eclampsia, or microangiopathic hemolytic anemia.[1] With the advent of antihypertensives, the incidence of hypertensive emergencies has declined from 7% to approximately 1% of patients with hypertension.[2] In addition, the 1-year survival rate associated with this condition has increased from only 20% (prior to 1950) to a survival rate of more than 90% with appropriate medical treatment
Hypertensive emergencies encompass a spectrum of clinical presentations in which uncontrolled blood pressures (BPs) lead to progressive or impending end-organ dysfunction. In these conditions, the BP should be lowered aggressively over minutes to hours. Neurologic end-organ damage due to uncontrolled BP may include hypertensive encephalopathy, cerebral vascular accident/cerebral infarction, subarachnoid hemorrhage, and/or intracranial hemorrhage.[1] Cardiovascular end-organ damage may include myocardial ischemia/infarction, acute left ventricular dysfunction, acute pulmonary edema, and/or aortic dissection. Other organ systems may also be affected by uncontrolled hypertension, which may lead to acute renal failure/insufficiency, retinopathy, eclampsia, or microangiopathic hemolytic anemia.[1] With the advent of antihypertensives, the incidence of hypertensive emergencies has declined from 7% to approximately 1% of patients with hypertension.[2] In addition, the 1-year survival rate associated with this condition has increased from only 20% (prior to 1950) to a survival rate of more than 90% with appropriate medical treatment
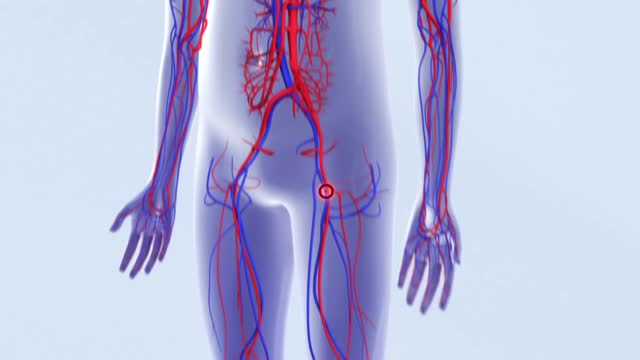
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs. Deep vein thrombosis can cause leg pain or swelling, but may occur without any symptoms. Deep vein thrombosis can develop if you have certain medical conditions that affect how your blood clots. Deep vein thrombosis can also happen if you don't move for a long time, such as after surgery, following an accident, or when you are confined to a hospital or nursing home bed. Deep vein thrombosis is a serious condition because blood clots in your veins can break loose, travel through your bloodstream and lodge in your lungs, blocking blood flow (pulmonary embolism).
The increased risk of thrombosis in patients with active cancer has multiple causes. Acute thrombosis of the aorta is an exceedingly rare but potentially devastating complication in patients with cancer receiving cisplatin-based chemotherapy. Prompt diagnosis and definitive treatment are imperative to decrease morbidity and mortality. Early diagnosis is difficult because initial presentation is often nonspecific, requiring a high degree of clinical suspicion. We report 4 cases of acute thrombosis of the abdominal aorta in patients with cancer receiving cisplatin-based chemotherapy. We review the clinical aspects, recommended investigation, and treatment of this potentially fatal complication.
Pulmonary embolism symptoms can vary greatly, depending on how much of your lung is involved, the size of the clots, and whether you have underlying lung or heart disease. Common signs and symptoms include: Shortness of breath. This symptom typically appears suddenly and always gets worse with exertion. Chest pain. You may feel like you're having a heart attack. The pain may become worse when you breathe deeply (pleurisy), cough, eat, bend or stoop. The pain will get worse with exertion but won't go away when you rest. Cough. The cough may produce bloody or blood-streaked sputum. Other signs and symptoms that can occur with pulmonary embolism include: Leg pain or swelling, or both, usually in the calf Clammy or discolored skin (cyanosis) Fever Excessive sweating Rapid or irregular heartbeat Lightheadedness or dizziness
Any independent vertical movement of the transducer or the patient will affect the hydrostatic column of this fluid-filled system and thus alter the pressure measurements. At some time before or after PAC insertion, the system must therefore be zeroed to ambient air pressure. The reference point for this is the midpoint of the left atrium (LA), estimated as the fourth intercostal space in the midaxillary line with the patient in the supine position. With the transducer at this height, the membrane is exposed to atmospheric pressure, and the monitor is then adjusted to zero. Calibration Once zeroed, the monitoring system must be calibrated for accuracy. Currently, most monitors perform an automated electronic calibration. Two methods are used to manually calibrate and check the system. If the catheter has not been inserted, the distal tip of the PAC is raised to a specified height above the LA. For example, raising the tip 20 cm above the LA should produce a reading of approximately 15 mm Hg if the system is working properly (1 mm Hg equals 1.36 cm H 2 O). Alternatively, pressure can be applied externally to the transducer and adjusted to a known level using a mercury or aneroid manometer. The monitor then is adjusted to read this pressure, and the system is calibrated. Dynamic tuning Central pressures are dynamic waveforms (ie, they vary from systole to diastole) and thus have a periodic frequency. To monitor these pressures accurately, the system requires an appropriate frequency response. A poorly responsive system produces inaccurate pressure readings, and differentiating waveforms (eg, PA from pulmonary capillary wedge pressure [PCWP]) can become difficult. When signal energy is lost, the pressure waveform is dampened. Common causes of this are air bubbles (which are compressible), long or compliant tubing, vessel wall impingement, intracatheter debris, transducer malfunction, and loose connections in the tubing. A qualitative test of the frequency response is performed by flicking the catheter and observing a brisk high-frequency response in the waveform. After insertion, the system can be checked by using the rapid flush test. When flushed, an appropriately responsive system shows an initial horizontal straight line with a high-pressure reading. Once the flushing is terminated, the pressure drops immediately, which is represented by a vertical line that plunges below the baseline. A brief and well-defined oscillation occurs, followed by return of the PA waveform. A dampened system will not overshoot or oscillate, and causes a delay in returning to the PA waveform.
The average time from symptom onset to diagnosis has been reported to be approximately 2 years. Despite recent attempts at increasing the awareness of pulmonary arterial hypertension (PAH), especially associated PAH (APAH), this delay in diagnosis has not changed appreciably in recent years. Early symptoms are nonspecific. Often, neither the patient nor the physician recognizes the presence of the disease, which leads to delays in diagnosis. Complicating matters, idiopathic PAH (IPAH) requires an extensive workup in an attempt to elucidate an identifiable cause of the elevated pulmonary artery pressure. The most common symptoms and their frequency, reported in a national prospective study, are as follows: Dyspnea (60% of patients) Weakness (19%) Recurrent syncope (13%) Additional symptoms include fatigue, lethargy, anorexia, chest pain, and right upper quadrant pain. Cough, hemoptysis, and hoarseness are less common symptoms. Women are more likely to be symptomatic than men.
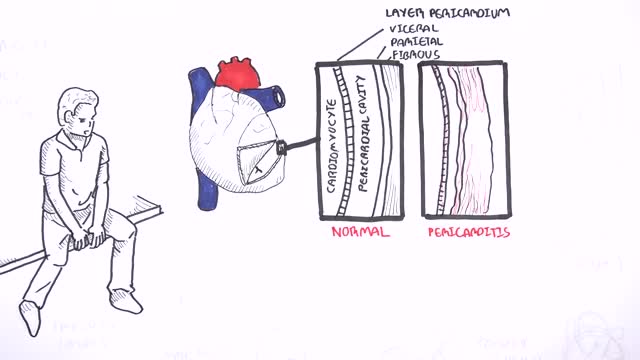
This video: Pericarditis is swelling and irritation of the pericardium, the thin sac-like membrane surrounding your heart. Pericarditis often causes chest pain and sometimes other symptoms. The sharp chest pain associated with pericarditis occurs when the irritated layers of the pericardium rub against each other. Pericarditis usually begins suddenly but doesn't last long (acute). When symptoms develop more gradually or persist, pericarditis is considered chronic. Most cases are mild and usually improve on their own. Treatment for more-severe cases may include medications and, rarely, surgery. Early diagnosis and treatment may help to reduce the risk of long-term complications from pericarditis.
How do you make a working human heart? Scientists can turn stem cells into beating heart cells, but getting them to organize into a 3D heart requires a scaffold. At the Massachusetts General Hospital in Boston, Harald Ott and his team are reusing the scaffold that nature provides. They’re stripping away all the living cells from dead hearts, before filling in the leftover matrix with healthy new cells. In this video, Brendan Maher finds out how the technique could be used to develop parts of the heart, like the aortic root and valve, for transplant.
The key difference between monophasic and biphasic defibrillator is that the monophasic defibrillator is a type of defibrillation waveform where a shock is delivered to the heart from one vector as shown below. Whereas, in biphasic defibrillation, shock is delivered to the heart via two vectors.
What Causes Chest Pain ?