Cardiology
Is My Chest Pain a Sign Of a Heart Attack?
Dilated cardiomyopathy is a disease of the heart muscle, usually starting in your heart's main pumping chamber (left ventricle). The ventricle stretches and thins (dilates) and can't pump blood as well as a healthy heart can. The term "cardiomyopathy" is a general term that refers to the abnormality of the heart muscle itself. Dilated cardiomyopathy might not cause symptoms, but for some people it can be life-threatening. A common cause of heart failure — the heart's inability to supply the body with enough blood — dilated cardiomyopathy can also contribute to irregular heartbeats (arrhythmias), blood clots or sudden death. The condition affects people of all ages, including infants and children, but is most common in men ages 20 to 60.
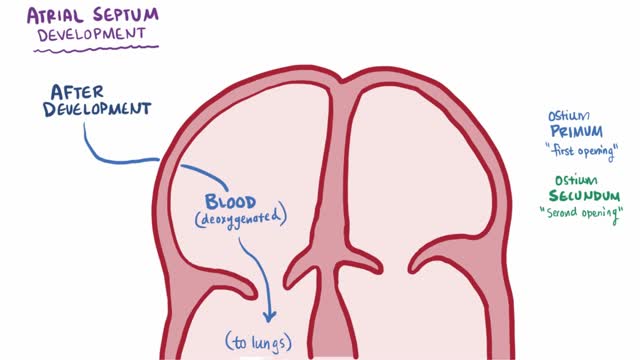
An atrial septal defect (ASD) is a hole in the wall between the two upper chambers of your heart (atria). The condition is present from birth (congenital). Small atrial septal defects may close on their own during infancy or early childhood. Large and long-standing atrial septal defects can damage your heart and lungs. Small defects may never cause a problem and may be found incidentally. An adult who has had an undetected atrial septal defect for decades may have a shortened life span from heart failure or high blood pressure that affects the arteries in the lungs (pulmonary hypertension). Surgery may be necessary to repair atrial septal defects to prevent complications.
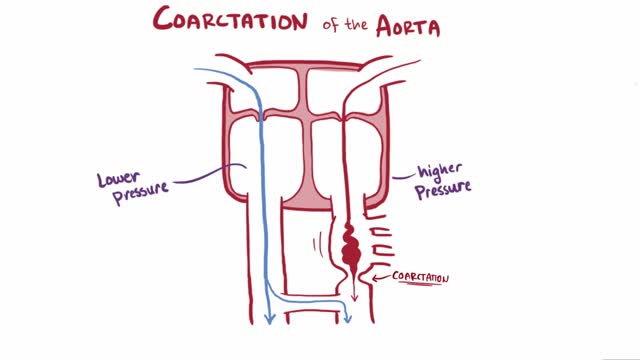
Coarctation of the aorta (CoA[1][2] or CoAo), also called aortic narrowing, is a congenital condition whereby the aorta is narrow, usually in the area where the ductus arteriosus (ligamentum arteriosum after regression) inserts. The word “coarctation” means narrowing. Coarctations are most common in the aortic arch. The arch may be small in babies with coarctations. Other heart defects may also occur when coarctation is present, typically occurring on the left side of the heart. When a patient has a coarctation, the left ventricle has to work harder. Since the aorta is narrowed, the left ventricle must generate a much higher pressure than normal in order to force enough blood through the aorta to deliver blood to the lower part of the body. If the narrowing is severe enough, the left ventricle may not be strong enough to push blood through the coarctation, thus resulting in lack of blood to the lower half of the body. Physiologically its complete form is manifested as interrupted aortic arch
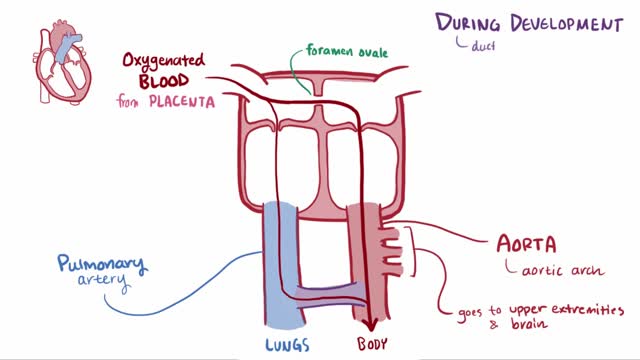
Patent ductus arteriosus (PDA) is a persistent opening between two major blood vessels leading from the heart. The opening, called the ductus arteriosus, is a normal part of a baby's circulatory system before birth that usually closes shortly after birth. If it remains open, however, it's called a patent ductus arteriosus. A small patent ductus arteriosus often doesn't cause problems and might never need treatment. However, a large patent ductus arteriosus left untreated can allow poorly oxygenated blood to flow in the wrong direction, weakening the heart muscle and causing heart failure and other complications. Treatment options for a patent ductus arteriosus include monitoring, medications and closure by cardiac catheterization or surgery.
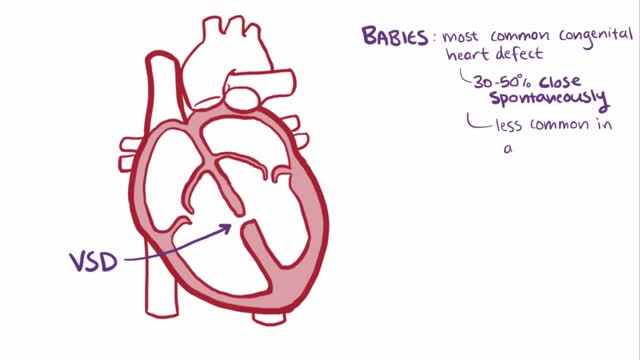
A ventricular septal defect (VSD), a hole in the heart, is a common heart defect that's present at birth (congenital). The hole occurs in the wall that separates the heart's lower chambers (septum) and allows blood to pass from the left to the right side of the heart. The oxygen-rich blood then gets pumped back to the lungs instead of out to the body, causing the heart to work harder. A small ventricular septal defect may cause no problems, and many small VSDs close on their own. Larger VSDs need surgical repair early in life to prevent complications.
Pulmonary hypertension is a type of high blood pressure that affects the arteries in your lungs and the right side of your heart. In one form of pulmonary hypertension, tiny arteries in your lungs, called pulmonary arterioles, and capillaries become narrowed, blocked or destroyed. This makes it harder for blood to flow through your lungs, and raises pressure within your lungs' arteries. As the pressure builds, your heart's lower right chamber (right ventricle) must work harder to pump blood through your lungs, eventually causing your heart muscle to weaken and fail. Some forms of pulmonary hypertension are serious conditions that become progressively worse and are sometimes fatal. Although some forms of pulmonary hypertension aren't curable, treatment can help lessen symptoms and improve your quality of life. Pulmonary hypertension care at Mayo Clinic
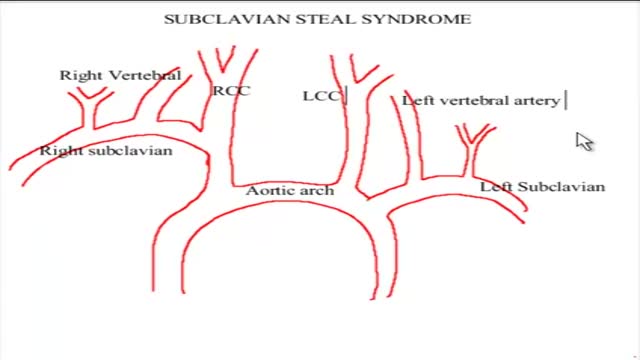
The term subclavian steal describes retrograde blood flow in the vertebral artery associated with proximal ipsilateral subclavian artery stenosis or occlusion, usually in the setting of subclavian artery occlusion or stenosis proximal to the origin of the vertebral artery. Alternatively, innominate artery disease has also been associated with retrograde flow in the ipsilateral vertebral artery, particularly where the subclavian artery origin is involved. Subclavian steal is frequently asymptomatic and may be discovered incidentally on ultrasound or angiographic examination for other indications, or it may be prompted by a clinical examination finding of reduced unilateral upper limb pulse or blood pressure. In some cases, patients may develop upper limb ischemic symptoms due to reduced arterial flow in the setting of subclavian artery occlusion, or they may develop neurologic symptoms due to posterior circulation ischemia associated with exercise of the ipsilateral arm.[1] Treatment has traditionally consisted of open subclavian artery revascularization, typically via carotid-subclavian bypass or subclavian artery transposition, which are generally durable procedures. Newer, less invasive options include endovascular intervention with recanalization as appropriate and angioplasty and stenting if required. The clinical relevance of subclavian steal was described in 1961 by Reivich, Holling and Roberts; however, the recognition of retrograde vertebral artery flow dates back another 100 years to Harrison and Smyth. Some papers, including a previous version of this article, advocate restricting the term subclavian steal to patients with neurologic symptoms only, but this is incorrect in view of the substantial literature using this term to describe the hemodynamic scenario of retrograde vertebral flow and proximal subclavian artery disease.
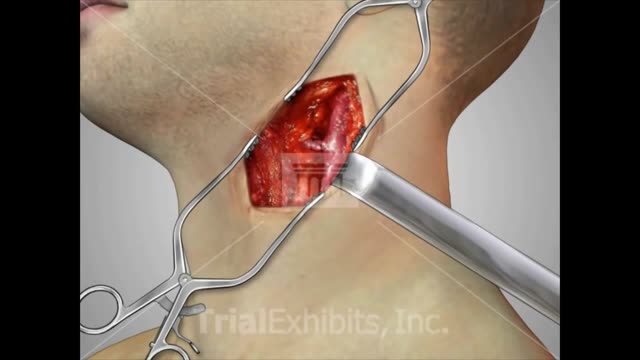
A carotid endarterectomy is performed in a sterile surgical suite or standard operating room. You may go home the same day or stay 1–2 nights after the procedure depending on your medical condition. You receive a local anesthetic or general anesthesia. Your vascular surgeon makes an incision at the front of your neck. After removing the plaque from the artery your vascular surgeon repairs the artery by stitching in a natural graft (formed from a piece of vein from elsewhere in your body) or a woven patch. The incision is closed
The objective of carotid endarterectomy (CEA) is to prevent strokes. In the United States, stroke is the third leading cause of death overall and the second leading cause of death for women.[1] Among patients suffering a stroke, 50-75% had carotid artery disease that would have been amenable to surgical treatment. Several prospective randomized trials have compared the safety and efficacy of CEA with those of medical therapy in symptomatic and asymptomatic patients. Data from these prospective trials have confirmed that CEA offers better protection from ipsilateral strokes than medical therapy alone in patients presenting with either symptomatic or asymptomatic carotid artery disease.
Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn't pump blood as well as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently. Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing salt in your diet, managing stress and losing weight — can improve your quality of life. One way to prevent heart failure is to control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
An aortic dissection is a serious condition in which the inner layer of the aorta, the large blood vessel branching off the heart, tears. Blood surges through the tear, causing the inner and middle layers of the aorta to separate (dissect). If the blood-filled channel ruptures through the outside aortic wall, aortic dissection is often fatal. Aortic dissection is relatively uncommon. The condition most frequently occurs in men in their 60s and 70s. Symptoms of aortic dissection may mimic those of other diseases, often leading to delays in diagnosis. However, when an aortic dissection is detected early and treated promptly, the chance of survival greatly improves.
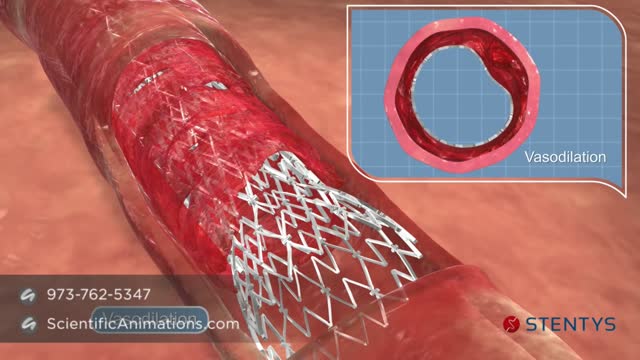
Before the angioplasty procedure begins, you will receive some pain medicine. You may also be given medicine that relaxes you, and blood thinning medicines to prevent a blood clot from forming. You will lie on a padded table. Your doctor will insert a flexible tube (catheter) through a surgical cut into an artery. Sometimes the catheter will be placed in your arm or wrist, or in your upper leg or groin area. You will be awake during the procedure. The doctor will use live x-ray pictures to carefully guide the catheter up into your heart and arteries. Dye will be injected into your body to highlight blood flow through the arteries. This helps the doctor see any blockages in the blood vessels that lead to your heart. A guide wire is moved into and across the blockage. A balloon catheter is pushed over the guide wire and into the blockage. The balloon on the end is blown up (inflated). This opens the blocked vessel and restores proper blood flow to the heart. A wire mesh tube (stent) may then be placed in this blocked area. The stent is inserted along with the balloon catheter. It expands when the balloon is inflated. The stent is left there to help keep the artery open
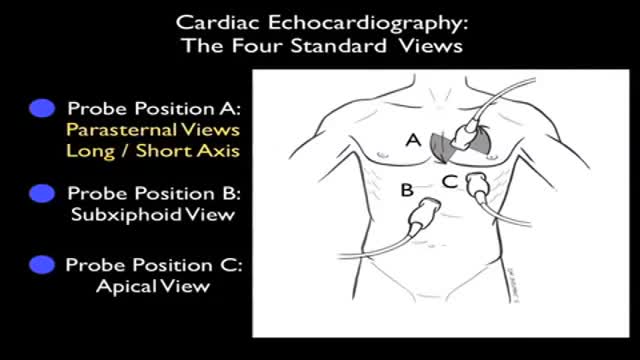
Ultrasound of Heart
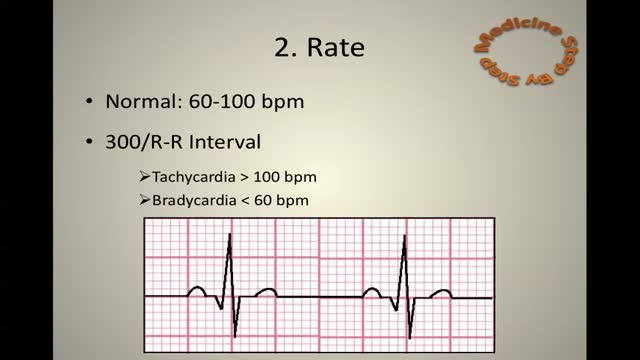
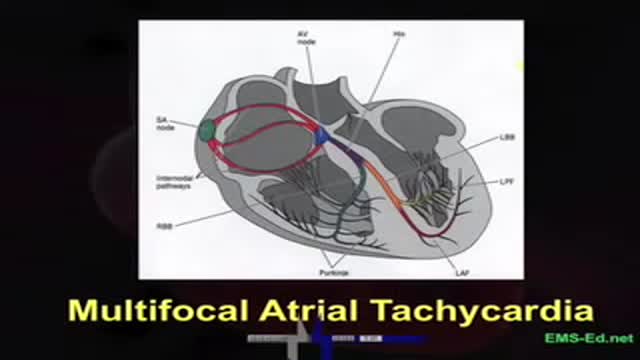
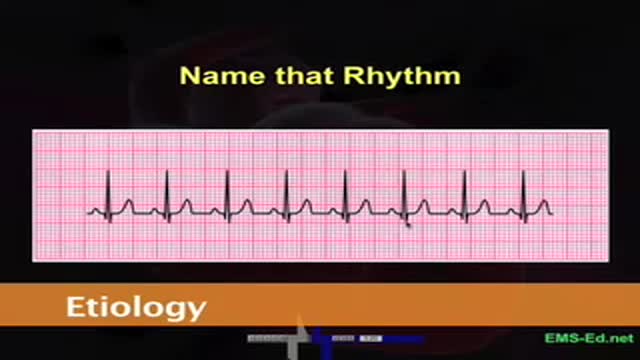
ECG Learn it
EKG Interpretation Part 3
ECG
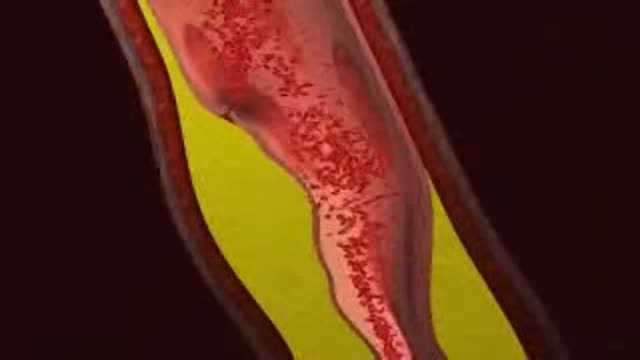
LDL (Bad) Cholesterol LDL cholesterol is considered the “bad” cholesterol because it contributes to plaque, a thick, hard deposit that can clog arteries and make them less flexible. This condition is known as atherosclerosis. If a clot forms and blocks a narrowed artery, heart attack or stroke can result. Another condition called peripheral artery disease can develop when plaque buildup narrows an artery supplying blood to the legs. View an animation of cholesterolHDL (Good) Cholesterol HDL cholesterol is considered “good” cholesterol because it helps remove LDL cholesterol from the arteries. Experts believe HDL acts as a scavenger, carrying LDL cholesterol away from the arteries and back to the liver, where it is broken down and passed from the body. One-fourth to one-third of blood cholesterol is carried by HDL. A healthy level of HDL cholesterol may also protect against heart attack and stroke, while low levels of HDL cholesterol have been shown to increase the risk of heart disease.
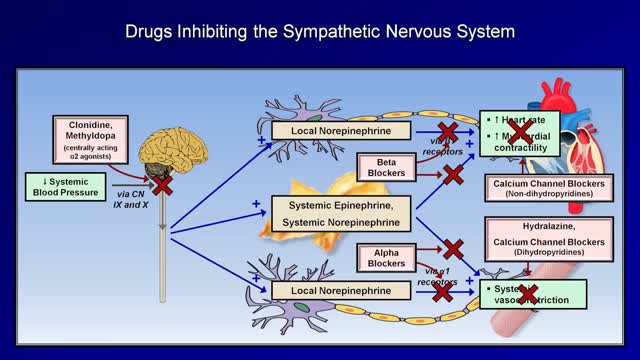
Although drug treatment of hypertension is associated with improved survival and decreased vascular complications, drug compliance is a major problem in the control of hypertension. All antihypertensive medications are associated with side effects; thus, it is a physician's responsibility to explain to each patient the side effects of the drugs he prescribes to treat hypertension, and to instill in the patient a sense of necessity for the treatment of hypertension. The choice of antihypertensive drug should be made based on each patient's lifestyle, overall health and ability to tolerate the drug. Ideally, the antihypertensive regimen should be simple, effective, convenient to take and have very few side effects.
Myocardial infarction (MI), commonly known as a heart attack, is defined pathologically as the irreversible death of myocardial cells caused by ischemia. Clinically, MI is a syndrome that can be recognized by a set of symptoms, chest pain being the hallmark of these symptoms in most cases, supported by biochemical laboratory changes, electrocardiographic (ECG) changes, or findings on imaging modalities able to detect myocardial injury and necrosis. According to the third universal definition of MI, implemented by a joint task force from the European Society of Cardiology (ESC), American College of Cardiology (ACC) Foundation, American Heart Association (AHA), and the World Heart Federation (WHF), MI is diagnosed when either of the following two criteria are met