Cardiology
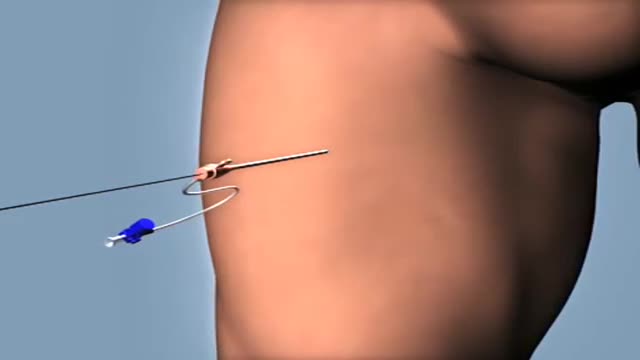
Cardiac cath is performed to find out if you have disease of the heart muscle, valves or coronary (heart) arteries. During the procedure, the pressure and blood flow in your heart can be measured. Coronary angiography is done during cardiac catheterization.
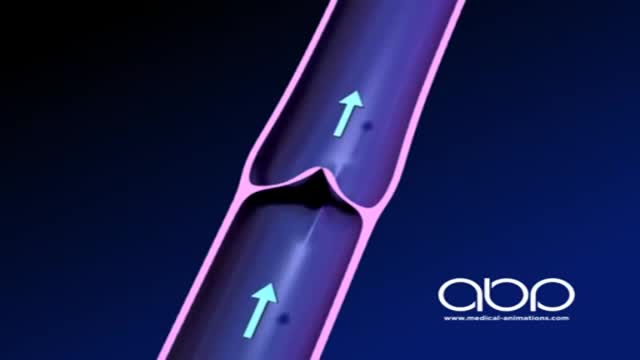
The deep veins play a significant role in propelling blood toward the heart. The one-way valves in deep veins prevent blood from flowing backward, and the muscles surrounding the deep veins compress them, helping force the blood toward the heart, just as squeezing a toothpaste tube ejects toothpaste.
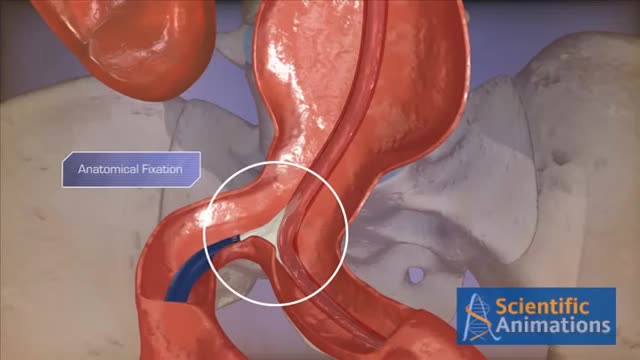
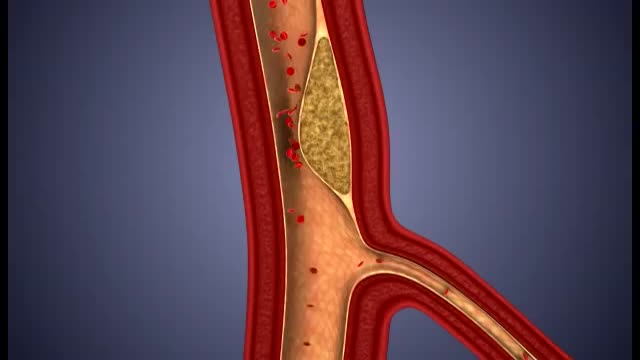
Abdominal aortic aneurysms can weaken the aorta, your body’s largest blood vessel. This can develop into a potentially serious heath problem that can be fatal if the aneurysm bursts, causing massive internal bleeding. Endovascular stent grafting, or endovascular aneurysm repair (EVAR), is a newer form of treatment for abdominal aortic aneurysm that is less invasive than open surgery. Endovascular stent grafting uses an endovascular stent graft to reinforce the wall of the aorta and to help keep the damaged area from rupturing.
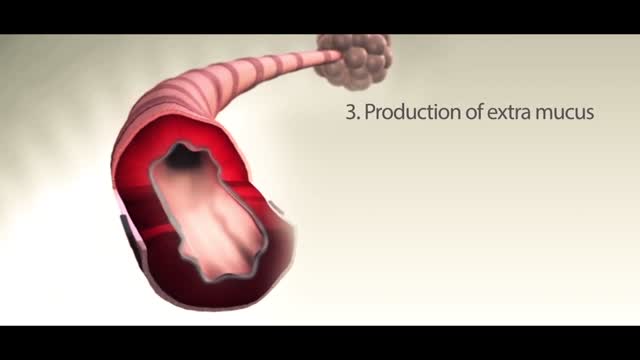
Asthma is a condition in which your airways narrow and swell and produce extra mucus. This can make breathing difficult and trigger coughing, wheezing and shortness of breath.
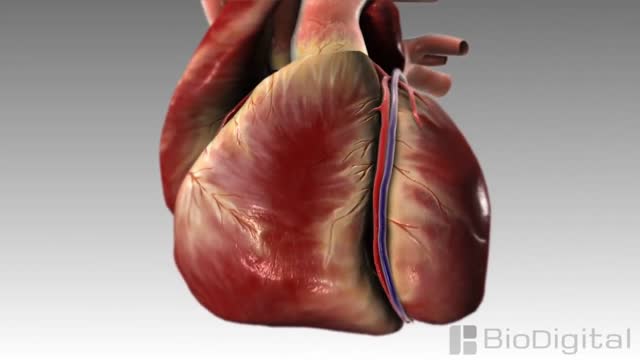
The heart is the body's engine room, responsible for pumping life-sustaining blood via a 60,000-mile-long (97,000-kilometer-long) network of vessels. The organ works ceaselessly, beating 100,000 times a day, 40 million times a year—in total clocking up three billion heartbeats over an average lifetime. It keeps the body freshly supplied with oxygen and nutrients, while clearing away harmful waste matter.
Endovascular Aneurysm Repair Endovascular aneurysm repair (or endovascular aortic repair) (EVAR) is a type of endovascular surgery used to treat pathology of the aorta, most commonly an abdominal aortic aneurysm (AAA).
A heart attack is a frightening, confusing and stressful experience. Life after a heart attack isn’t easy, but we’re with you all the way on your journey toward recovery. Here you will find information about heart attack warning signs, risk factors, diagnosis, treatment, and life as a survivor or caregiver. You will also find heart attack tools and resources to help you get and stay healthy.
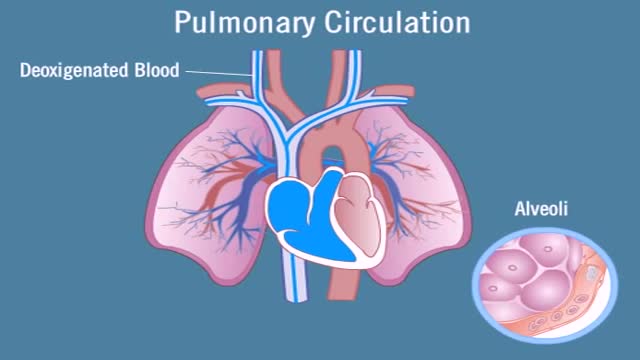
Pulmonary circulation is the portion of the cardiovascular system which carries deoxygenated blood away from the heart, to the lungs, and returns oxygenated (oxygen-rich) blood back to the heart. The function of pulmonary circulation is to exchange carbon dioxide for oxygen in the blood. It is the passage of blood from the heart to the capillaries of the lungs, where the gases are exchanged, and back to the heart to be pumped around the body.
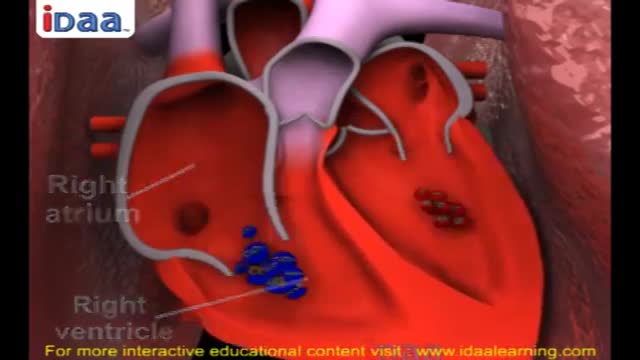
Systemic circulation carries oxygenated blood from the left ventricle, through the arteries, to the capillaries in the tissues of the body. From the tissue capillaries, the deoxygenated blood returns through a system of veins to the right atrium of the heart.
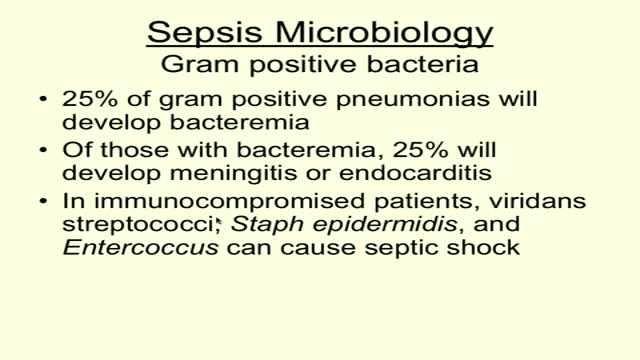
Sepsis is a potentially life-threatening complication of an infection. Sepsis occurs when chemicals released into the bloodstream to fight the infection trigger inflammatory responses throughout the body. This inflammation can trigger a cascade of changes that can damage multiple organ systems, causing them to fail. If sepsis progresses to septic shock, blood pressure drops dramatically, which may lead to death. Anyone can develop sepsis, but it's most common and most dangerous in older adults or those with weakened immune systems. Early treatment of sepsis, usually with antibiotics and large amounts of intravenous fluids, improves chances for survival. Symptoms & causes Symptoms Many doctors view sepsis as a three-stage syndrome, starting with sepsis and progressing through severe sepsis to septic shock. The goal is to treat sepsis during its early stage, before it becomes more dangerous. Sepsis To be diagnosed with sepsis, you must exhibit at least two of the following symptoms, plus a probable or confirmed infection: Body temperature above 101 F (38.3 C) or below 96.8 F (36 C) Heart rate higher than 90 beats a minute Respiratory rate higher than 20 breaths a minute Severe sepsis Your diagnosis will be upgraded to severe sepsis if you also exhibit at least one of the following signs and symptoms, which indicate an organ may be failing: Significantly decreased urine output Abrupt change in mental status Decrease in platelet count Difficulty breathing Abnormal heart pumping function Abdominal pain Septic shock To be diagnosed with septic shock, you must have the signs and symptoms of severe sepsis — plus extremely low blood pressure that doesn't adequately respond to simple fluid replacement. When to see a doctor Most often sepsis occurs in people who are hospitalized. People in the intensive care unit are especially vulnerable to developing infections, which can then lead to sepsis. If you get an infection or if you develop signs and symptoms of sepsis after surgery, hospitalization or an infection, seek medical care immediately. Causes While any type of infection — bacterial, viral or fungal — can lead to sepsis, the most likely varieties include: Pneumonia Abdominal infection Kidney infection Bloodstream infection (bacteremia) The incidence of sepsis appears to be increasing in the United States. The causes of this increase may include: Aging population. Americans are living longer, which is swelling the ranks of the highest risk age group — people older than 65. Drug-resistant bacteria. Many types of bacteria can resist the effects of antibiotics that once killed them. These antibiotic-resistant bacteria are often the root cause of the infections that trigger sepsis. Weakened immune systems. More Americans are living with weakened immune systems, caused by HIV, cancer treatments or transplant drugs. Risk factors Sepsis is more common and more dangerous if you: Are very young or very old Have a compromised immune system Are already very sick, often in a hospital's intensive care unit Have wounds or injuries, such as burns Have invasive devices, such as intravenous catheters or breathing tubes Complications Sepsis ranges from less to more severe. As sepsis worsens, blood flow to vital organs, such as your brain, heart and kidneys, becomes impaired. Sepsis can also cause blood clots to form in your organs and in your arms, legs, fingers and toes — leading to varying degrees of organ failure and tissue death (gangrene). Most people recover from mild sepsis, but the mortality rate for septic shock is nearly 50 percent. Also, an episode of severe sepsis may place you at higher risk of future infections.
Best Foods For Blocked Arteries
Your doctor says your chest pain (angina) is caused by blockages in your heart arteries and that you need to get those blockages taken care of. What are your options? First, it's important to determine what type of angina you have. Different types of angina may need different treatments. Common types of angina are chronic stable angina — a type of angina that occurs when your heart is working hard — and unstable angina, which is new chest pain or chest pain that is getting worse. Other types of angina include variant angina — a rare type of angina caused by a spasm in the coronary arteries — and microvascular angina, which can be a symptom of disease in the small coronary artery blood vessels. Unstable angina is a serious situation and requires emergency treatment. Treatment for unstable angina involves hospitalization with medications to stabilize your condition. Some people with unstable angina may require a procedure called angioplasty (also known as percutaneous coronary intervention), usually combined with the placement of a small metal tube called a stent. In some cases of unstable angina, heart surgery (coronary bypass surgery) may be needed. Generally, if you have mild stable angina that is controlled by medications, you may not need further treatments. If you're experiencing symptoms of chronic stable angina even after taking medications and making lifestyle changes, or if you're at higher risk of serious heart disease, your doctor may recommend angioplasty or coronary bypass surgery. Making a decision on how to treat your angina can be difficult, but knowing the benefits and risks of stents and medications may help you decide.
It's a symptom of heart disease but typically does not cause permanent damage to the heart. It is, though, a sign that you are a candidate for a heart attack at some point in the future. The chest pain may spread to your arm, shoulder, jaw, or back. It may feel like a pressure or squeezing sensation.
A ventricular septal defect (VSD) is an opening or hole in the wall that separates the two lower chambers of the heart. This wall is called the ventricular septum. The hole causes oxygen-rich blood to leak from the left side of the heart to the right side. This causes extra work for the right side of the heart, since more blood than necessary is flowing through the right ventricle to the lungs. The hole is usually closed with surgery. However, in certain situations, your child's cardiologist and surgeon may think it is best to close the hole with a special device. This procedure is done in the heart catheterization lab.
A ventricular septal defect (VSD) is an opening or hole in the wall that separates the two lower chambers of the heart. This wall is called the ventricular septum. The hole causes oxygen-rich blood to leak from the left side of the heart to the right side. This causes extra work for the right side of the heart, since more blood than necessary is flowing through the right ventricle to the lungs.
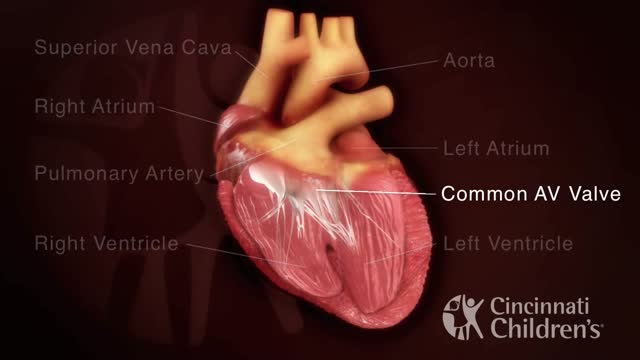
An atrioventricular septal defect (AVSD) is a heart defect in which there are holes between the chambers of the right and left sides of the heart, and the valves that control the flow of blood between these chambers may not be formed correctly
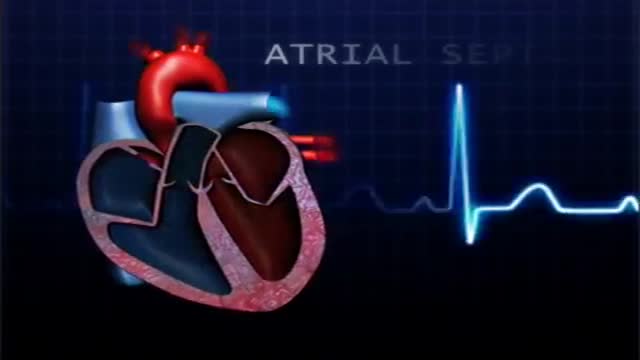
atrial septal defect (ASD) is a hole in the wall between the two upper chambers of your heart (atria). The condition is present from birth (congenital). Small atrial septal defects may close on their own during infancy or early childhood. Large and long-standing atrial septal defects can damage your heart and lungs. Small defects may never cause a problem and may be found incidentally. An adult who has had an undetected atrial septal defect for decades may have a shortened life span from heart failure or high blood pressure that affects the arteries in the lungs (pulmonary hypertension). Surgery may be necessary to repair atrial septal defects to prevent complications
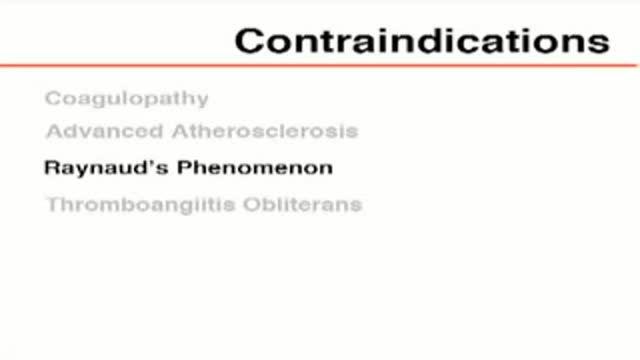
What damage does atherosclerosis cause? Plaque may partially or totally block the blood's flow through an artery in the heart, brain, pelvis, legs, arms or kidneys. Some of the diseases that may develop as a result of atherosclerosis include coronary heart disease, angina (chest pain), carotid artery disease, peripheral artery disease (PAD) and chronic kidney disease.
A central venous catheter, also called a central line, is a long, thin, flexible tube used to give medicines, fluids, nutrients, or blood products over a long period of time, usually several weeks or more. A catheter is often inserted in the arm or chest through the skin into a large vein.
There are two main purposes of an arterial line. Firstly when patients are very sick an arterial line is inserted to provide constant monitoring and recording of the patient's blood pressure. Secondly some patients require frequent blood tests and the arterial line provides easy access to a patient's blood.