Gynecology
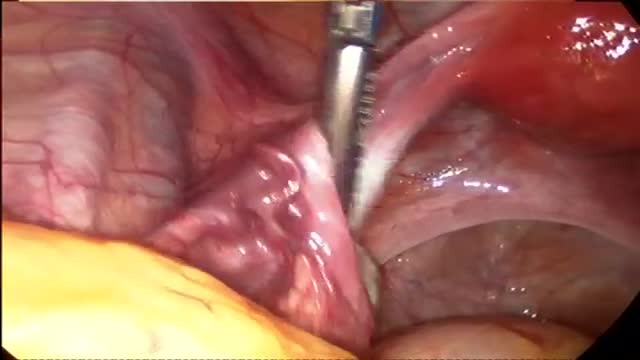
Endometriosis surgery
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It usually occurs when sexually transmitted bacteria spread from your vagina to your uterus, fallopian tubes or ovaries. Many women who develop pelvic inflammatory disease either experience no signs or symptoms or don't seek treatment. Pelvic inflammatory disease may be detected only later when you have trouble getting pregnant or if you develop chronic pelvic pain.
How to Get Pregnant Quickly With Irregular Periods
can i get pregnant right after my period
Best Position for Getting Pregnant Fast
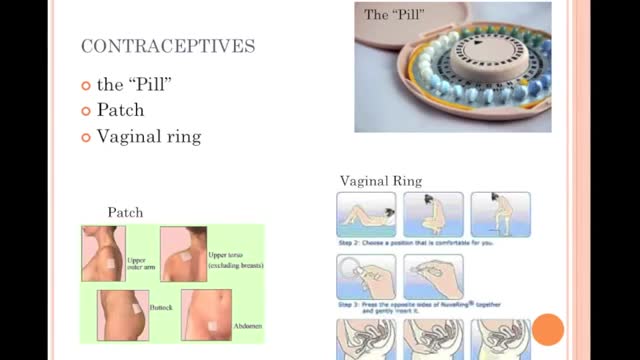
Specific treatment for menorrhagia is based on a number of factors, including: Your overall health and medical history The cause and severity of the condition Your tolerance for specific medications, procedures or therapies The likelihood that your periods will become less heavy soon Your future childbearing plans Effects of the condition on your lifestyle Your opinion or personal preference Drug therapy for menorrhagia may include: Iron supplements. If you also have anemia, your doctor may recommend that you take iron supplements regularly. If your iron levels are low but you're not yet anemic, you may be started on iron supplements rather than waiting until you become anemic. Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs, such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve), help reduce menstrual blood loss. NSAIDs have the added benefit of relieving painful menstrual cramps (dysmenorrhea). Tranexamic acid. Tranexamic acid (Lysteda) helps reduce menstrual blood loss and only needs to be taken at the time of the bleeding. Oral contraceptives. Aside from providing birth control, oral contraceptives can help regulate menstrual cycles and reduce episodes of excessive or prolonged menstrual bleeding. Oral progesterone. When taken for 10 or more days of each menstrual cycle, the hormone progesterone can help correct hormone imbalance and reduce menorrhagia. The hormonal IUD (Mirena). This intrauterine device releases a type of progestin called levonorgestrel, which makes the uterine lining thin and decreases menstrual blood flow and cramping. If you have menorrhagia from taking hormone medication, you and your doctor may be able to treat the condition by changing or stopping your medication.
Menorrhagia is the medical term for menstrual periods with abnormally heavy or prolonged bleeding. Although heavy menstrual bleeding is a common concern among premenopausal women, most women don't experience blood loss severe enough to be defined as menorrhagia. With menorrhagia, every period you have causes enough blood loss and cramping that you can't maintain your usual activities. If you have menstrual bleeding so heavy that you dread your period, talk with your doctor. There are many effective treatments for menorrhagia.
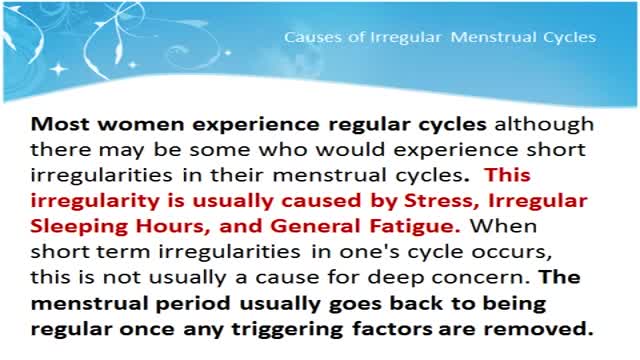
Most women have between 11 and 13 menstrual periods each year. You may be different: You may have more or fewer. Missed or irregular periods must be looked at in terms of what is normal for you. Menstrual periods are often irregular during the first few years after menstruation starts. It may take several years for the hormones that control menstruation to reach a balance. Menstrual periods also may be very irregular at the other end of the menstrual years. Many women realize that they are approaching perimenopause and menopause when their otherwise regular periods become irregular. Menopause occurs when it has been 12 months since you had a menstrual period. Pregnancy is the most common cause of a missed period. If you might be pregnant, treat yourself as if you are pregnant until you know for sure. Use a home pregnancy test as the first step to finding out whether you are pregnant.
Uterine fibroids are noncancerous growths of the uterus that often appear during childbearing years. Also called leiomyomas (lie-o-my-O-muhs) or myomas, uterine fibroids aren't associated with an increased risk of uterine cancer and almost never develop into cancer. Fibroids range in size from seedlings, undetectable by the human eye, to bulky masses that can distort and enlarge the uterus. You can have a single fibroid or multiple ones. In extreme cases, multiple fibroids can expand the uterus so much that it reaches the rib cage. Many women have uterine fibroids sometime during their lives. But most women don't know they have uterine fibroids because they often cause no symptoms. Your doctor may discover fibroids incidentally during a pelvic exam or prenatal ultrasound.
OverviewSymptomsTestingComplicationsTreatmentPreventionTakeawayRead This Next What is gonorrhea? Highlights Some people may never develop noticeable symptoms. Gonorrhea is usually treated with an antibiotic injection or oral antibiotics. You’re at a higher risk of contracting gonorrhea if you’ve had any other STDs. Gonorrhea is a sexually transmitted disease (STD). It’s caused by infection with the bacterium Neisseria gonorrhoeae. It tends to infect warm, moist areas of the body, including the: urethra (the tube that drains urine from the urinary bladder) eyes throat vagina anus female reproductive tract (the fallopian tubes, cervix, and uterus) Gonorrhea passes from person to person through unprotected oral, anal, or vaginal sex. People with numerous sexual partners or those who don’t use a condom are at greatest risk of infection. The best protections against infection are abstinence, monogamy (sex with only one partner), and proper condom usage. Behaviors that make a person more likely to engage in unprotected sex also increase the likelihood of infection. These behaviors include alcohol abuse and illegal drug abuse, particularly intravenous drug use. Advertisement Symptoms of gonorrhea Symptoms
Preventing Sexually Transmitted Diseases A sexually transmitted disease (STD) is an infection that is spread during sexual contact with another person. This includes touching, since some STDs can be spread from skin-to-skin contact. In general, STDs are highly preventable. Almost 20 million new STDs are diagnosed each year in the United States, according to the Centers for Disease Control and Prevention (CDC). However, a large number of those infections could be avoided if people made different decisions about their sexual health. The only guaranteed method to prevent STDs is to abstain from all sexual contact. This may not a practical solution for everyone. Fortunately, there are steps people can take to limit their risk of exposure.
Choosing not to have sex provides 100 percent protection from HIV, STIs, and pregnancy. For some, this means avoiding vaginal, anal, and oral-genital intercourse altogether. Others may choose to avoid any type of sexual or intimate contact, including hugging and kissing. Choosing not to have sex is often referred to as “abstinence.” WHAT ARE THE ADVANTAGES OF CHOOSING NOT TO HAVE SEX (ABSTINENCE)? Choosing not to have sex is free and available to all. Not having sex is extremely effective at preventing both infection and pregnancy. It is the only 100% effective method of preventing sexually transmitted infections (STIs) and unintended pregnancy. Not having sex can be practiced at any time in one's life. Not having sex may encourage people to build relationships in other ways. Not having sex may be the course of action which you feel is right for you and makes you feel good about yourself.
Looking for a week-by-week guide to pregnancy? You're in luck! We've got loads of expert-approved info about each week and trimester, including what's up with your growing baby and what changes to expect for yourself. You'll find stunning fetal development videos, thousands of articles, and helpful tools like our Due Date Calculator and Baby Names Finder. Meet other parents-to-be in our online community, and get all of this and more in our free pregnancy app. Dive in, and congratulations!
Polycystic ovary syndrome (PCOS) is a common endocrine system disorder among women of reproductive age. Women with PCOS may have enlarged ovaries that contain small collections of fluid — called follicles — located in each ovary as seen during an ultrasound exam. Infrequent or prolonged menstrual periods, excess hair growth, acne, and obesity can all occur in women with polycystic ovary syndrome. In adolescents, infrequent or absent menstruation may raise suspicion for the condition. The exact cause of polycystic ovary syndrome is unknown. Early diagnosis and treatment along with weight loss may reduce the risk of long-term complications, such as type 2 diabetes and heart disease.
Menstruation is the time of month when the womb (uterus) sheds its lining and vaginal bleeding occurs. This is known as a menstrual period. Periods vary widely from woman to woman. Some periods are punctual, some are unpredictable. On average, a woman gets her period every 24 to 38 days. A period usually lasts about two to eight days. Irregular periods may require treatment. What Are Irregular Periods? You may have irregular periods if: The time between each period starts to change. You are losing more or less blood during a period than usual. The number of days that your period lasts varies significantly. There are different terms for different types of irregular periods: Irregular Menstrual Bleeding (IrregMB): Bleeding of more than 20 days in individual cycle lengths over a period of one year. Absent Menstrual Bleeding (amenorrhea): No bleeding in a 90-day period. Heavy Menstrual Bleeding (HMB): Excessive menstrual blood loss that interferes with the woman’s physical, emotional, social, and material quality of life and can occur alone or in combination with other symptoms. Heavy and Prolonged Menstrual Bleeding (HPMB): Less common than HMB. It is important to make a distinction from HMB given they may have different etiologies and respond to different therapies. Light Menstrual Bleeding: Based on patient complaint, rarely related to pathology.
To relieve mild menstrual cramps: Take aspirin or another pain reliever, such as Tylenol (acetaminophen), Motrin (ibuprofen) or Aleve (naproxen). (Note: For best relief, you must take these medications as soon as bleeding or cramping starts.) Place a heating pad or hot water bottle on your lower back or abdomen
How to Stop Your Period
Back pain during pregnancy is a common complaint — and it's no wonder. You're gaining weight, your center of gravity changes, and your hormones are relaxing the ligaments in the joints of your pelvis. Often, however, you can prevent or ease back pain during pregnancy. Consider seven ways to give pregnancy back pain the boot. 1. Practice good posture As your baby grows, your center of gravity shifts forward. To avoid falling forward, you might compensate by leaning back — which can strain the muscles in your lower back and contribute to back pain during pregnancy. Keep these principles of good posture in mind: Stand up straight and tall. Hold your chest high. Keep your shoulders back and relaxed. Don't lock your knees. When you stand, use a comfortably wide stance for the best support. If you must stand for long periods of time, rest one foot on a low step stool — and take time for frequent breaks. Good posture also means sitting with care. Choose a chair that supports your back, or place a small pillow behind your lower back. 2. Get the right gear Wear low-heeled — not flat — shoes with good arch support. Avoid high heels, which can further shift your balance forward and cause you to fall. You might also consider wearing a maternity support belt. Although research on the effectiveness of maternity support belts is limited, some women find the additional support helpful. 3. Lift properly When lifting a small object, squat down and lift with your legs. Don't bend at the waist or lift with your back. It's also important to know your limits. Ask for help if you need it. 4. Sleep on your side Sleep on your side, not your back. Keep one or both knees bent. Consider using pregnancy or support pillows between your bent knees, under your abdomen and behind your back.
HOW BABY GROWS IN THE WOMB DURING PREGNANCY
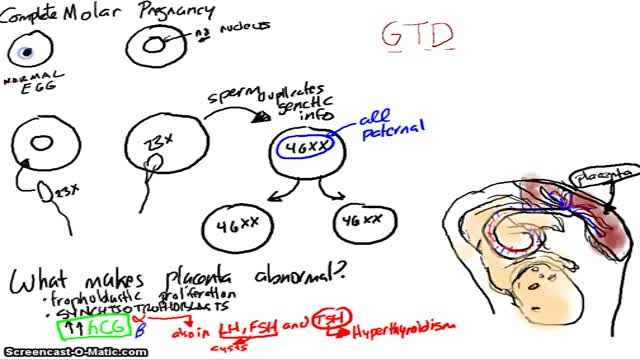
A molar pregnancy — also known as hydatidiform mole — is a noncancerous (benign) tumor that develops in the uterus. A molar pregnancy starts when an egg is fertilized, but instead of a normal, viable pregnancy resulting, the placenta develops into an abnormal mass of cysts. In a complete molar pregnancy, there's no embryo or normal placental tissue. In a partial molar pregnancy, there's an abnormal embryo and possibly some normal placental tissue. The embryo begins to develop but is malformed and can't survive. A molar pregnancy can have serious complications — including a rare form of cancer — and requires early treatment.