Gynecology
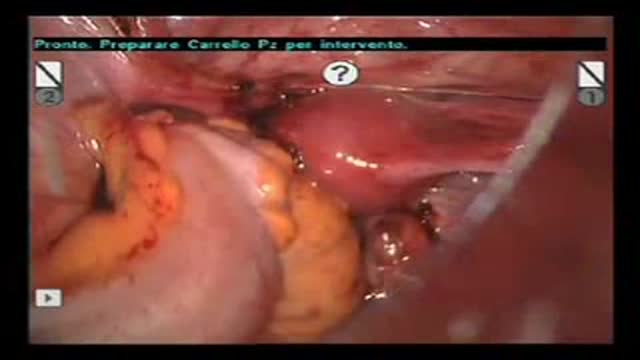
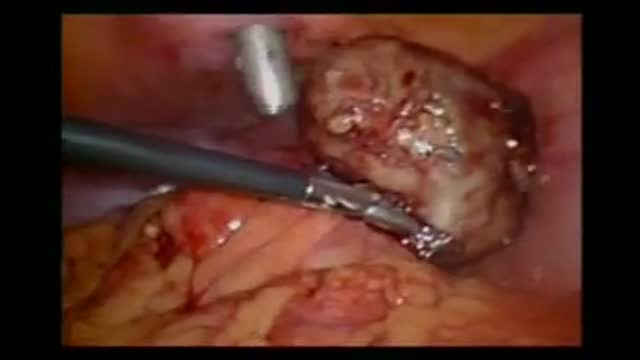
An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open
After birth care for babies,a small glimpse just to let you know what happens.
Something you should know about Wonderful Tonight.
A local doctor says that the new pap smear guidelines makes sense for many women
A video discussing Causes of Itching in the Vulva
An animation showing the Pelvic Inflammatory Disease (PID)
The pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling . Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border.) The perineum has the pelvic floor as its superior border.
Some sources do not consider “pelvic floor” and “pelvic diaphragm” to be identical, with the “diaphragm” consisting of only the levator ani and coccygeus, while the “floor” also includes the perineal membrane and deep perineal pouch.
The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling . Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border.) The perineum has the pelvic floor as its superior border.
Some sources do not consider “pelvic floor” and “pelvic diaphragm” to be identical, with the “diaphragm” consisting of only the levator ani and coccygeus, while the “floor” also includes the perineal membrane and deep perineal pouch. However, other sources include the fascia as part of the diaphragm. In practice, the two terms are often used interchangeably.
Inferiorly, the pelvic floor extends into the anal triangle.
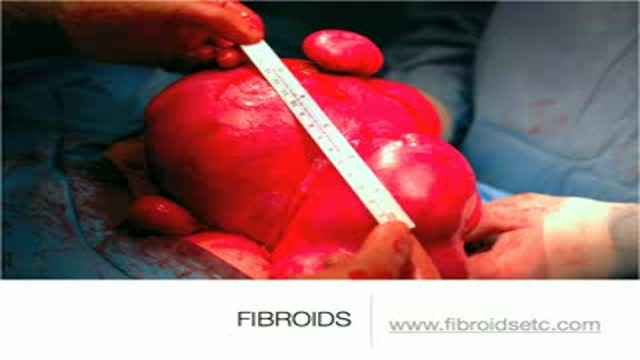
A uterine fibroid (also uterine leiomyoma, myoma, fibromyoma, leiofibromyoma, fibroleiomyoma, and fibroma) (plural of ... myoma is ...myomas or ...myomata) is a benign (non-cancerous) tumor that originates from the smooth muscle layer (myometrium) and the accompanying connective tissue of the uterus. Fibroids are the most common benign tumors in females and typically found during the middle and later reproductive years. While most fibroids are asymptomatic, they can grow and cause heavy and painful menstruation, painful sexual intercourse, and urinary frequency and urgency. Uterine fibroids is the major indication for hysterectomy in the US.[2] Fibroids are often multiple and if the uterus contains too many leiomyomatas to count, it is referred to as uterine leiomyomatosis. The malignant version of a fibroid is uncommon and termed a leiomyosarcoma.
Uploaded by http://nursing-resource.com
Laparoscopic Tubal Ligation using Filshie Clips. Brought to you by http://nursing-resource.com
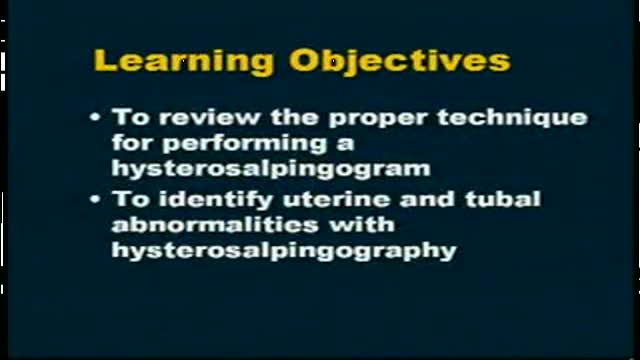
Video is an excellent introduction to Hysterosalpingography and summarizes different pathologies. While the information on this presentation is about health care issues, it is not medical advice. People seeking specific medical advice or assistance should contact their personal physician. Although we believe the information in this presentation to be accurate and timely, because of the rapid advances in health care and our reliance on information provided by outside sources, we make no warranty or guarantee concerning the accuracy or reliability of the content or other material which we may reference. When clinical matters are discussed, the opinions presented are those of the discussants only. The material discussed on the presentation is not intended to present the only or necessarily the best method or procedure, but rather presents the approach or opinion of the discussant. This presentation is provided in an “as is” format without warranties of any kind, expressed or implied, including but not limited to warranties of title, non-infringement or implied warranties of merchantability or fitness for a particular purpose.
Caesarean section is the most common way to deliver a breech baby in the USA, Australia, and Great Britain. Like any major surgery, it involves risks. Maternal mortality is increased by a Caesarean section, but still remains a rare complication in the First World. Third World statistics are dramatically different, and mortality is increased significantly. There is remote risk of injury to the mother’s internal organs, injury to the baby, and severe hemorrhage requiring hysterectomy with resultant infertility. More commonly seen are problems with noncatastrophic bleeding, postoperative infection and wound healing problems. It should be added that the increase in maternal mortality rates could be slightly skewed due to the fact that Caesarean sections are often used during high-risk pregnancies and/or when mortality is already a strong possibility.
One large study has confirmed that elective cesarean section has lower risk to the fetus and a slightly increased risk to the mother, than planned vaginal delivery of the breech however elements of the methodology used have undergone some criticism.
The same birth injuries that can occur in vaginal breech birth may rarely occur in Caesarean breech delivery. A Caesarean breech delivery is still a breech delivery. However the soft tissues of the uterus and abdominal wall are more forgiving of breech delivery than the hard bony ring of the pelvis. If a Caesarean is scheduled in advance (rather than waiting for the onset of labor) there is a risk of accidentally delivering the baby too early, so that the baby might have complications of prematurity. The mother’s subsequent pregnancies will be riskier than they would be after a vaginal birth (uterine rupture). The presence of a uterine scar will be a risk factor for any subsequent pregnancies.
Causes of declining libido in women
Robot-Assisted Laparoscopic Rectal Resection for Endometriosis
Recto-vaginal medical examination
Dr. Berger, Medical Director of Chapel Hill Tubal Reversal Center discusses the pros and cons of tubal reversal vs. IVF with a couple wanting a baby after a tubal ligation.
Anterior vaginal wall relaxation (cystocele) is one of the most commonly diagnosed forms of pelvic organ prolapse in women. More than 200,000 cystocele repairs are completed yearly, however to date the procedures that are completed do not provide very high cure rates and/or poor anatomic outcomes. Successful treatment of anterior vaginal wall prolapse remains one of the most challenging aspects of pelvic reconstructive surgery we face. We have developed very good procedures that provide excellent support for the posterior wall (ie rectoceles) and the apex of the vagina (ie vaginal vault prolapse) and reproduce normal anatomy. We were one of the first centers in the country to utilize grafts in rectocele repairs and have seen improved cure rates to over 90% with minimal complications. It has been known for many years that abdominal sacralcolpopexy with placement of a mesh graft at the top of the vagina for vaginal vault prolapse is the most successful procedure in the literature. We have made advancements with this procedure as well in being able to offer our patients a laparoscopic minimally invasive approach for sacralcolpopexy, with the same excellent cure rates (>92%) and with hospital stays typically less than 24 hours and reduced complications. However the anterior wall has been one of the most difficult compartments in the vagina to get good anatomic results and high cure rates with traditional repairs and at the same time not cause sexual dysfunction, pain with intercourse, voiding dysfunction (ie incontinence or urgency/frequency syndrome), or a shortened or scarred down vagina. The transobturator approach was developed as a less invasive way to place an anterior wall graft (see below) however this still involved blind needle passes and the graft did not support the apex of the vagina, therefore the search for improvements in these procedures is ongoing.
Laparoscopic Salpengectomy of a torted Fallopian Tube
Conjoined Twins