Nephrology
Post-streptococcal GN is a form of glomerulonephritis. It is caused by an infection with a type of streptococcus bacteria. The infection does not occur in the kidneys, but in a different part of the body, such as the skin or throat. The strep bacterial infection causes the tiny blood vessels in the filtering units of the kidneys (glomeruli) to become inflamed. This makes the kidneys less able to filter the urine. Post-streptococcal GN is uncommon today because infections that can lead to the disorder are commonly treated with antibiotics. The disorder may develop 1 to 2 weeks after an untreated throat infection, or 3 to 4 weeks after a skin infection. It may occur in people of any age, but it most often occurs in children ages 6 through 10. Although skin and throat infections are common in children, post-streptococcal GN is a rare complication of these infections. Risk factors include: Strep throat Streptococcal skin infections (such as impetigo)
Wilms tumor, also known as nephroblastoma, is a cancer of the kidneys that typically occurs in children, rarely in adults. It is named after Dr. Max Wilms, the German surgeon (1867–1918) who first described it. Approximately 500 cases are diagnosed in the U.S. annually.
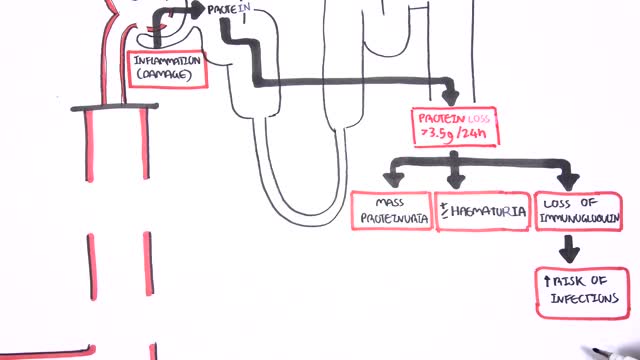
Nephrotic syndrome is a kidney disorder that causes your body to excrete too much protein in your urine. Nephrotic syndrome is usually caused by damage to the clusters of small blood vessels in your kidneys that filter waste and excess water from your blood. Nephrotic syndrome causes swelling (edema), particularly in your feet and ankles, and increases the risk of other health problems. Treatment for nephrotic syndrome includes treating the underlying condition that's causing it and taking medications. Nephrotic syndrome can increase your risk of infections and blood clots. Your doctor may recommend medications and dietary changes to prevent these and other complications of nephrotic syndrome.
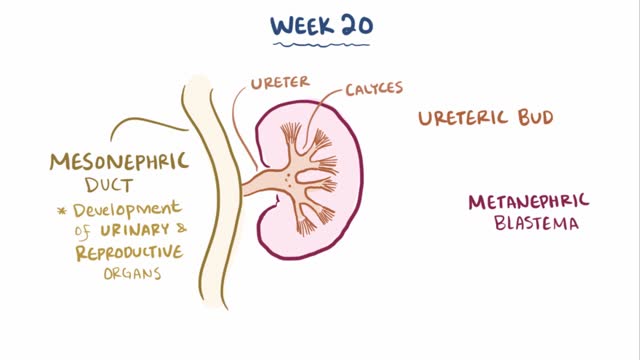
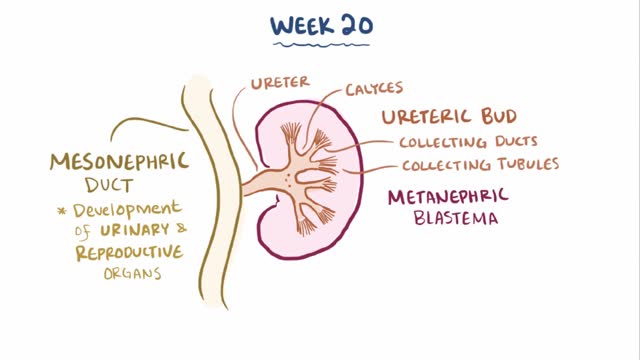
Multicystic dysplastic kidney (MCDK) is a condition that results from the malformation of the kidney during fetal development. The kidney consists of irregular cysts of varying sizes. Multicystic dysplastic kidney is a common type of renal cystic disease, and it is a cause of an abdominal mass in infants.
Renal agenesis is a condition in which a newborn is missing one or both kidneys. Unilateral renal agenesis (URA) is the absence of one kidney. Bilateral renal agenesis (BRA) is the absence of both kidneys. Both types of renal agenesis occur in fewer than 1 percent of births annually, according to the March of Dimes. Fewer than 1 in every 1,000 newborns has URA. BRA is much rarer, occurring in about 1 in every 3,000 births.
Artificial kidney is often a synonym for hemodialysis, but may also, more generally, refer to renal replacement therapies (with exclusion of kidney transplantation) that are in use and/or in development.
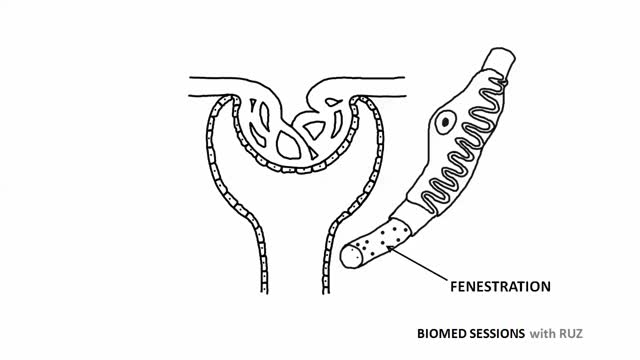
Peritoneal dialysis is a treatment for kidney failure that uses the lining of your abdomen, or belly, to filter your blood inside your body. ... The process of first draining the used dialysis solution and then replacing it with fresh solution is called an exchange.
Hold your elbows at shoulder level and place the backs of your hands together with your wrists bent at 90 degrees. This position increases the pressure on the median nerve. If the test reproduces or worsens your symptoms (pain and tingling in your hands), you may have carpal tunnel syndrome.
To identify an UTI, keep an eye out for the following symptoms: A burning feeling when you urinate. A frequent or intense urge to urinate, even though little comes out when you do. Pain or pressure in your back or lower abdomen. Cloudy, dark, bloody, or strange-smelling urine. Feeling tired or shaky.
Indications for intervention in patients with a renal artery aneurysm (RAA) include the following [20, 8, 13, 14] : Rupture Symptomatic RAA - Hypertension (from associated renal artery stenosis, refractory to medical management), pain, renal ischemia or infarction secondary to embolization from the aneurysm sac RAAs in females who are pregnant or are contemplating pregnancy Diameter greater than 2 cm Enlarging RAA RAA associated with acute dissection Currently, there is no consensus regarding the size at which an RAA should be repaired in an asymptomatic patient. Experts have recommended RAA repair at diameters ranging from 1.5 to 3 cm, [8] though most suggest 2 cm. Some reports have even suggest that larger asymptomatic saccular aneurysms may be managed expectantly. Note that aneurysm rupture at a diameter of 1.5 cm has been reported. Complete calcification of the wall of the aneurysm sac manifests in about 40% of patients. This was once believed to confer protection against rupture [21] ; however, this belief has since been questioned. [30] Asymptomatic, small (<2 cm in diameter) RAAs do not usually require treatment. One notable exception is an RAA in a woman who is pregnant or contemplating pregnancy. In view of the increased risk of rupture in such cases, even small asymptomatic aneurysms should be repaired in this population. For diagnosis and preinterventional planning, gadolinium-enhanced magnetic resonance angiography (MRA) and computed tomography (CT) angiography (CTA) with three-dimensional (3D) reconstruction have essentially replaced conventional arteriography. Regular follow-up examination with ultrasonography (US) or CT) is recommended in patients who are treated expectantly. Spontaneous cure by thrombosis of small aneurysms has been described. Further refinements in endovascular techniques may allow more RAAs to be treated in this manner. So far, excellent short- and intermediate-term results have been described in the literature [40] ; however, there remains a need for further long-term outcome data.
Renal artery stenosis is the narrowing of one or more arteries that carry blood to your kidneys (renal arteries). Narrowing of the arteries prevents normal amounts of oxygen-rich blood from reaching your kidneys. Your kidneys need adequate blood flow to help filter waste products and remove excess fluids. Reduced blood flow may increase blood pressure in your whole body (systemic blood pressure) and injure kidney tissue.
Interventional Nephrology is a new and emerging subspecialty of Nephrology that mainly deals with ultrasonography of kidneys and ultrasound-guided renal biopsy, insertion of peritoneal dialysis catheters, tunneled dialysis catheters as a vascular access for patients undergoing hemodialysis as well as percutaneous ...
A renal biopsy is a procedure used to extract kidney tissue for laboratory analysis. The word “renal” describes the kidneys. A renal biopsy is also called a kidney biopsy. The test helps your doctor identify the type of kidney disease you have, how severe it is, and the best treatment for it.
The kidneys are a pair of organs located in the back of the abdomen. Each kidney is about 4 or 5 inches long -- about the size of a fist. The kidneys' function are to filter the blood. All the blood in our bodies passes through the kidneys several times a day. The kidneys remove wastes, control the body's fluid balance, and regulate the balance of electrolytes. As the kidneys filter blood, they create urine, which collects in the kidneys' pelvis -- funnel-shaped structures that drain down tubes called ureters to the bladder. Each kidney contains around a million units called nephrons, each of which is a microscopic filter for blood. It's possible to lose as much as 90% of kidney function without experiencing any symptoms or problems.
Depending on the underlying cause, some types of kidney disease can be treated. Often, though, chronic kidney disease has no cure. Treatment usually consists of measures to help control signs and symptoms, reduce complications, and slow progression of the disease. If your kidneys become severely damaged, you may need treatment for end-stage kidney disease. Treating the cause Your doctor will work to slow or control the cause of your kidney disease. Treatment options vary, depending on the cause. But kidney damage can continue to worsen even when an underlying condition, such as high blood pressure, has been controlled. Treating complications Kidney disease complications can be controlled to make you more comfortable. Treatments may include: High blood pressure medications. People with kidney disease may experience worsening high blood pressure. Your doctor may recommend medications to lower your blood pressure — commonly angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers — and to preserve kidney function. High blood pressure medications can initially decrease kidney function and change electrolyte levels, so you may need frequent blood tests to monitor your condition. Your doctor will likely also recommend a water pill (diuretic) and a low-salt diet. Medications to lower cholesterol levels. Your doctor may recommend medications called statins to lower your cholesterol. People with chronic kidney disease often experience high levels of bad cholesterol, which can increase the risk of heart disease.
Kidney failure and transplant options One of the most serious complications of polycystic kidney disease is kidney failure. This is when the kidneys are no longer able to filter waste products, maintain fluid balance, and maintain blood pressure on their own. When this occurs, your doctor will discuss options with you that may include a kidney transplant or dialysis treatments to act as artificial kidneys. If your doctor does place you on a kidney transplant list, there are several factors that determine your placement. These include your overall health, expected survival, and time you have been on dialysis. It’s also possible that a friend or relative could donate a kidney to you. Because people can live with only one kidney with relatively few complications, this can be an option for families who have a willing donor. The decision to undergo a kidney transplant or donate a kidney to a person with kidney disease can be a difficult one. Speaking to your nephrologist can help you weigh your options. You can also ask what medications and treatments can help you live as well as possible in the meantime. According to the University of Iowa, the average kidney transplant will allow kidney function from 10 to 12 years.
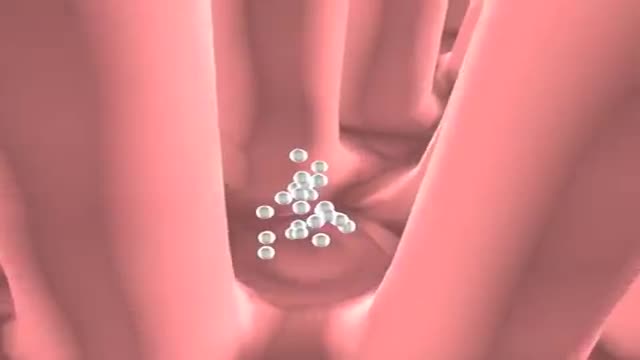
Glomerular filtration is the first step in making urine. It is the process that your kidneys use to filter excess fluid and waste products out of the blood into the urine collecting tubules of the kidney, so they may be eliminated from your body.
Peritoneal dialysis (per-ih-toe-NEE-ul die-AL-uh-sis) is a way to remove waste products from your blood when your kidneys can no longer do the job adequately. A cleansing fluid flows through a tube (catheter) into part of your abdomen and filters waste products from your blood. After a prescribed period of time, the fluid with filtered waste products flows out of your abdomen and is discarded. Peritoneal dialysis differs from hemodialysis, a more commonly used blood-filtering procedure. With peritoneal dialysis, you can give yourself treatments at home, at work or while traveling. Peritoneal dialysis isn't an option for everyone wit
Failing Kidneys and Different Treatment Options
Hemodialysis is a process that uses a membrane (dialyzer) to: Remove wastes, such as urea, from the blood. Restore the proper balance of electrolytes in the blood. Eliminate extra fluid from the body.