Nephrology
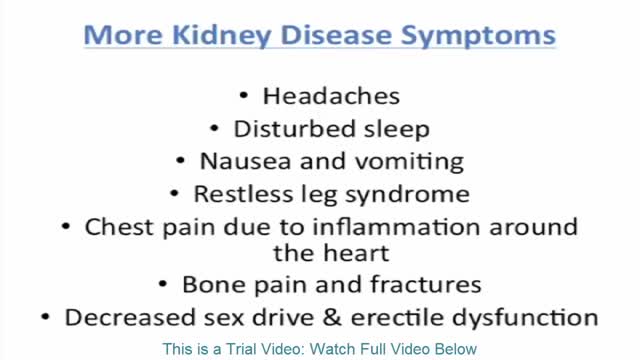
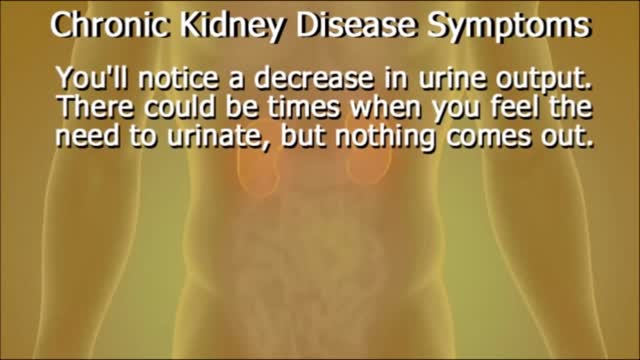
Signs and symptoms of chronic kidney disease develop over time if kidney damage progresses slowly. Signs and symptoms of kidney disease may include: Nausea Vomiting Loss of appetite Fatigue and weakness Sleep problems Changes in how much you urinate Decreased mental sharpness Muscle twitches and cramps Swelling of feet and ankles Persistent itching Chest pain, if fluid builds up around the lining of the heart Shortness of breath, if fluid builds up in the lungs High blood pressure (hypertension) that's difficult to control Signs and symptoms of kidney disease are often nonspecific, meaning they can also be caused by other illnesses. Because your kidneys are highly adaptable and able to compensate for lost function, signs and symptoms may not appear until irreversible damage has occurred.
Chronic kidney disease includes conditions that damage your kidneys and decrease their ability to keep you healthy by doing the jobs listed. If kidney disease gets worse, wastes can build to high levels in your blood and make you feel sick. You may develop complications like high blood pressure, anemia (low blood count), weak bones, poor nutritional health and nerve damage. Also, kidney disease increases your risk of having heart and blood vessel disease. These problems may happen slowly over a long period of time. Chronic kidney disease may be caused by diabetes, high blood pressure and other disorders. Early detection and treatment can often keep chronic kidney disease from getting worse. When kidney disease progresses, it may eventually lead to kidney failure, which requires dialysis or a kidney transplant to maintain life.
Acute kidney failure occurs when your kidneys suddenly become unable to filter waste products from your blood. When your kidneys lose their filtering ability, dangerous levels of wastes may accumulate, and your blood's chemical makeup may get out of balance. Acute kidney failure — also called acute renal failure or acute kidney injury — develops rapidly over a few hours or a few days. Acute kidney failure is most common in people who are already hospitalized, particularly in critically ill people who need intensive care. Acute kidney failure can be fatal and requires intensive treatment. However, acute kidney failure may be reversible. If you're otherwise in good health, you may recover normal or nearly normal kidney function.
arteriovenous hemodialysis access has been the "gold standard" for patients needing hemodialysis for the past 30 years. Despite the reported advantages of autologous access, the availability of prosthetic graft material, coupled with the challenging dialysis candidate, has led to a trend of primary prosthetic graft dialysis access in the 1980s and 1990s. In recognition of this unfortunate trend, the National Kidney Foundation Dialysis Outcomes Quality Initiative (DOQI) used evidence from published studies and summary articles to generate clinical practice guidelines, emphasizing a shift back to autologous arteriovenous fistula (AVF) as the key to long-term successful hemodialysis.[1,2] These initial guidelines proposed a goal of 50% autologous AVF as the initial access, with a 40% prevalence of autologous access for a given practice or unit.
Dehydration is a condition that occurs when the loss of body fluids, mostly water, exceeds the amount that is taken in. With dehydration, more water is moving out of our cells and bodies than what we take in through drinking. We lose water every day in the form of water vapor in the breath we exhale and in our excreted sweat, urine, and stool. Along with the water, small amounts of salts are also lost.
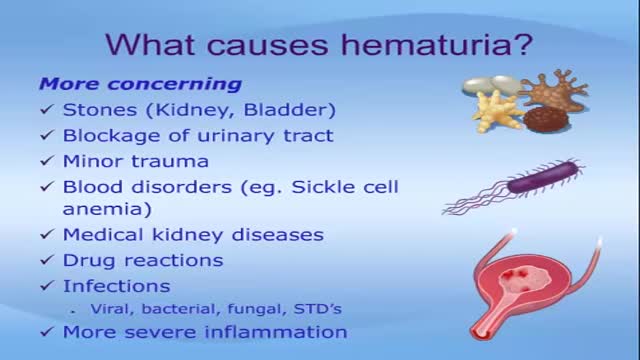
Seeing blood in your urine can cause anxiety. While in many instances there are benign causes, blood in urine (hematuria) can also indicate a serious disorder. Blood that you can see is called gross hematuria. Urinary blood that's visible only under a microscope is known as microscopic hematuria and is found when your doctor tests your urine. Either way, it's important to determine the reason for the bleeding. Treatment depends on the underlying cause.
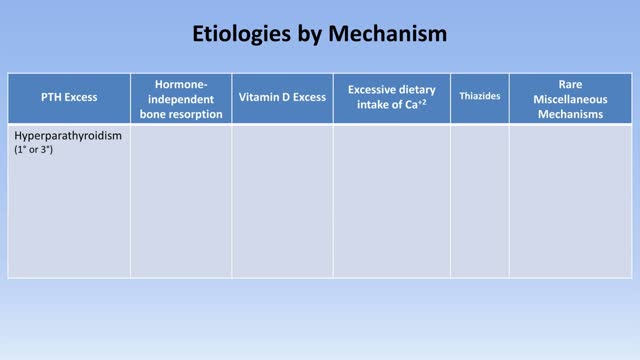
Hypercalcemia is a condition in which the calcium level in your blood is above normal. Too much calcium in your blood can weaken your bones, create kidney stones, and interfere with the way your heart and brain works. Hypercalcemia most commonly results from overactive parathyroid glands. These four tiny glands are each about the size of a grain of rice and are located on or near the thyroid gland. Other causes of hypercalcemia include cancer, certain other medical disorders, some medications, and excessive use of calcium and vitamin D supplements. Signs and symptoms of hypercalcemia may range from nonexistent to severe. Treatment depends on the underlying cause.
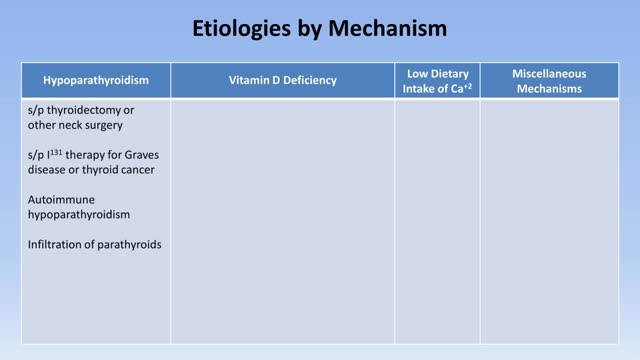
In neonates, hypocalcemia is more likely to occur in infants born of diabetic or preeclamptic mothers. Hypocalcemia also may occur in infants born to mothers with hyperparathyroidism. Clinically evident hypocalcemia generally presents in milder forms and is usually the result of a chronic disease state. In emergency department patients, chronic or subacute complaints secondary to mild or moderate hypocalcemia are more likely to be a chief complaint than severe symptomatic hypocalcemia. Once laboratory results demonstrate hypocalcemia, the first question is whether the hypocalcemia is true—that is, whether it is representative of a decrease in ionized calcium. The presence of chronic diarrhea or intestinal disease (eg, Crohn disease, sprue, chronic pancreatitis) suggests the possibility of hypocalcemia due to malabsorption of calcium and/or vitamin D. The patient's past medical history should be explored for pancreatitis, anxiety disorders, renal or liver failure, gastrointestinal disorders, and hyperthyroidism or hyperparathyroidism. Previous neck surgery suggests hypoparathyroidism; a history of seizures suggests hypocalcemia secondary to anticonvulsants. The patient may have a recent history of thyroid, parathyroid, or bowel surgeries or recent neck trauma. The length of time that a disorder is present is an important clue. Hypoparathyroidism and pseudohypoparathyroidism are lifelong disorders. Instead, acute transient hypocalcemia may be associated with acute gastrointestinal illness, nutritional deficiency, or acute or chronic renal failure. In an elderly patient, a nutritional deficiency may be associated with a low intake of vitamin D. A history of alcoholism can help diagnose hypocalcemia due to magnesium deficiency, malabsorption, or chronic pancreatitis. Inquire about recent use of drugs associated with hypocalcemia, including the following: Radiocontrast Estrogen Loop diuretics Bisphosphonates Calcium supplements Antibiotics Antiepileptic drugs Cinacalcet Other considerations in the history include the following: Family history of hypocalcemia Low-calcium diet Lack of sun exposure
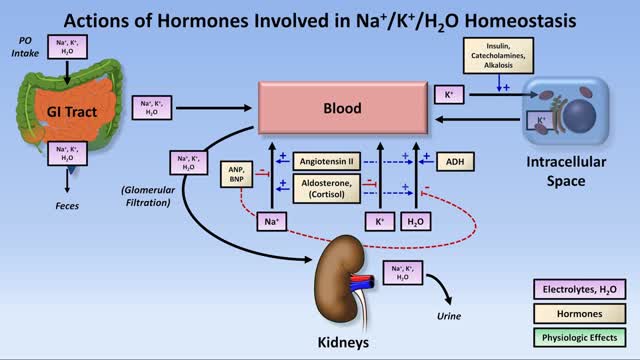
Hyponatremia is a condition that occurs when the level of sodium in your blood is abnormally low. Sodium is an electrolyte, and it helps regulate the amount of water that's in and around your cells. In hyponatremia, one or more factors — ranging from an underlying medical condition to drinking too much water during endurance sports — causes the sodium in your body to become diluted. When this happens, your body's water levels rise, and your cells begin to swell. This swelling can cause many health problems, from mild to life-threatening. Hyponatremia treatment is aimed at resolving the underlying condition. Depending on the cause of hyponatremia, you may simply need to cut back on how much you drink. In other cases of hyponatremia, you may need intravenous fluids and medications
Sodium levels are tightly controlled in a healthy individual by regulation of urine concentration and an intact thirst mechanism. Hypernatremia (defined as a serum sodium level >145 mEq/L) is rare in patients with preserved thirst mechanism. When hypernatremia does occur, it is associated with a high mortality rate (>50% in most studies). Given this high mortality rate, the emergency physician must be able to recognize and treat this condition. This article discusses the patients in whom hypernatremia should be suspected and how to initiate workup and administer appropriate treatment. In general, hypernatremia can be caused by derangement of the thirst response or altered behavioral response thereto (primarily psychiatric patients, and elderly patients who are institutionalized), impaired renal concentrating mechanism (diabetes insipidus [DI]) secondary to kidney pathology (nephrogenic DI) or difficulty with the neurohormonal control of this concentrating mechanism (central DI), or by losses of free water from other sources.
Low potassium (hypokalemia) refers to a lower than normal potassium level in your bloodstream. Potassium is a chemical (electrolyte) that is critical to the proper functioning of nerve and muscles cells, particularly heart muscle cells. Normally, your blood potassium level is 3.6 to 5.2 millimoles per liter (mmol/L). A very low potassium level (less than 2.5 mmol/L) can be life-threatening and requires urgent medical attention.
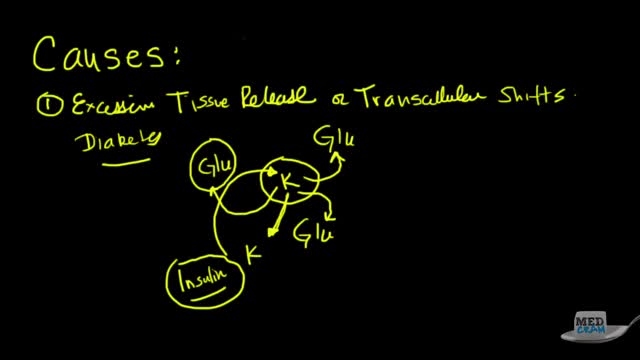
Hyperkalemia is defined as a serum potassium concentration higher than the upper limit of the normal range; the range in infants and children is age-dependent, whereas the range for adults is approximately 3.5-5.5 mEq/L. The upper limit may be considerably higher in young or premature infants, as high as 6.5 mEq/L.[5] Degrees of hyperkalemia are defined as follows[6] : 5.5-6.0 mEq/L – Mild 6.1-7.0 mEq/L – Moderate ≥7.0 mEq/L – Severe levels higher than 7 mEq/L can lead to significant hemodynamic and neurologic consequences. levels exceeding 8.5 mEq/L can cause respiratory paralysis or cardiac arrest and can quickly be fatal. Because of a paucity of distinctive signs and symptoms, hyperkalemia can be difficult to diagnose. Indeed, it is frequently discovered as an incidental laboratory finding. The physician must be quick to consider hyperkalemia in patients who are at risk for this disease process. (See Etiology.) However, any single laboratory study demonstrating hyperkalemia must be repeated to confirm the diagnosis, especially if the patient has no changes on electrocardiography (ECG). Because hyperkalemia can lead to sudden death from cardiac arrhythmias, any suggestion of hyperkalemia requires an immediate ECG to ascertain whether ECG signs of electrolyte imbalance are present (see Workup). Continuous ECG monitoring is essential if hyperkalemia is confirmed. Other testing is directed toward uncovering the condition or conditions that led to the hyperkalemia (see Workup). The aggressiveness of therapy for hyperkalemia is directly related to the rapidity with which the condition has developed, the absolute level of serum potassium, and the evidence of toxicity. The faster the rise of the potassium level, the higher it has reached, and the greater the evidence of cardiotoxicity, the more aggressive therapy should be. In severe cases, treatment focuses on immediate stabilization of the myocardial cell membrane, rapid shifting of potassium to the intracellular space, and total body potassium elimination. In addition, all sources of exogenous potassium should be immediately discontinued. (See Treatment.)
Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux is the abnormal flow of urine from your bladder back up the tubes (ureters) that connect your kidneys to your bladder. Normally, urine flows only down from your kidneys to your bladder. Vesicoureteral reflux is usually diagnosed in infants and children. The disorder increases the risk of urinary tract infections, which, if left untreated, can lead to kidney damage. Vesicoureteral reflux can be primary or secondary. Children with primary vesicoureteral reflux are born with a defect in the valve that normally prevents urine from flowing backward from the bladder into the ureters. Secondary vesicoureteral reflux is due to a urinary tract malfunction, often caused by infection. Children may outgrow primary vesicoureteral reflux. Treatment, which includes medication or surgery, aims at preventing kidney damage.
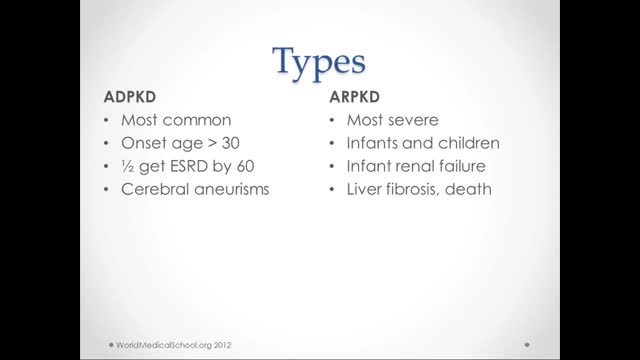
What is polycystic kidney disease? Polycystic kidney disease (also called PKD) causes numerous cysts to grow in the kidneys. These cysts are filled with fluid. If too many cysts grow or if they get too big, the kidneys can become damaged. PKD cysts can slowly replace much of the kidneys, reducing kidney function and leading to kidney failure. How common is PKD? In the United States about 600,000 people have PKD. It is the fourth leading cause of kidney failure. It is found in all races and occurs equally in men and women. It causes about 5% of all kidney failure. What other organs besides the kidney are affected by PKD? PKD can affect other organs besides the kidney. People with PKD may have cysts in their liver, pancreas, spleen, ovaries, and large bowel. Cysts in these organs usually do not cause serious problems, but can in some people. PKD can also affect the brain or heart. If PKD affects the brain, it can cause an aneurysm. An aneurysm is a bulging blood vessel that can burst, resulting in a stroke or even death. If PKD affects the heart, the valves can become floppy, resulting in a heart murmur in some patients. What are the clues that someone has PKD? Most people do not develop symptoms until they are 30 to 40 years old. The first noticeable signs and symptoms may include: Back or side pain An increase in the size of the abdomen Blood in the urine Frequent bladder or kidney infections High blood pressure High blood pressure is the most common sign of PKD. Occasionally, patients may develop headaches related to high blood pressure or their doctors may detect high blood pressure during a routine physical exam. Because high blood pressure can cause kidney damage, it is very important to treat it. In fact, treatment of high blood pressure can help slow or even prevent kidney failure. Fluttering or pounding in the chest About 25% of PKD patients have a so-called floppy valve in the heart, and may experience a fluttering or pounding in the chest as well as chest pain. These symptoms almost always disappear on their own but may be the first hint that someone has PKD. How is PKD diagnosed? Ultrasound is the most reliable, inexpensive and non-invasive way to diagnose PKD. If someone at risk for PKD is older than 40 years and has a normal ultrasound of the kidneys, he or she probably does not have PKD. Occasionally, a CT scan (computed tomography scan) and MRI (magnetic resonance imaging) may detect smaller cysts that cannot be found by an ultrasound. MRI is used to measure and monitor volume and growth of kidneys and cysts. In some situations, genetic testing might also be done. This involves a blood test that checks for abnormal genes that cause the disease. Genetic testing is not recommended for everyone. The test is costly, and it also fails to detect PKD in about 15% of people who have it. However, genetic testing can be useful when a person: has an uncertain diagnosis based on imaging tests has a family history of PKD and wants to donate a kidney is younger than 30-years old with a family history of PKD and a negative ultrasound, and is planning to start a family
Renal transplantation is the treatment of choice for a minority of patients with end-stage renal disease (ESRD). Most adult patients with ESRD are never referred for evaluation for transplantation, and have a 70% 5-year mortality on dialysis. Marked improvements in early graft survival and long-term graft function have made kidney transplantation a more cost-effective alternative to dialysis. In the United States, over 375,000 kidney transplants have been performed, and in 2012, 191,400 patients were alive and with a functioning transplanted kidney; currently, more than 101,000 patients are waiting for kidney transplants.[1, 2] Before the advent of immunosuppression, renal transplantation was limited to identical twins and was not applicable to the vast majority of patients with ESRD. The introduction of combined azathioprine-steroid therapy in 1963 produced encouraging results and became the mainstay of immunosuppression. Although this therapy improved the results of transplantation, acute rejection and complications associated with steroid therapy persisted. The introduction of cyclosporine in 1983 significantly improved the outcomes of all solid-organ transplants by reducing the risk of rejection. Further innovations, including anti–T cell antibodies (both monoclonal and polyclonal preparations), as well as other maintenance immunosuppressants (eg, tacrolimus, mycophenolate, sirolimus), have made a significant impact on both patient and graft survival. Currently, 1-year patient and graft survival rates exceed 90% in most transplant centers. For patient education information, see Kidney Transplant and the Mayo Clinic's kidney transplant information Web page.
Dissection and Cannulation of Cadaveric Kidney
Hemodialysis Machine Setup
Diabetic Nephropathy Animation 3D
Acute Renal Failure for Nursing
Peritoneal Dialysis for Kidney Disease