Neurology
Alcohol not broken down by the liver goes to the rest of the body, including the brain. Alcohol can affect parts of the brain that control movement, speech, judgment, and memory. These effects lead to the familiar signs of drunkenness: difficulty walking, slurred speech, memory lapses, and impulsive behavior.
-Korsakoff's syndrome is a common and preventable sequel of Wernicke's encephalopathy. Thiamine, if given during the stage of Wernicke's encephalopathy, can prevent the onset of Korsakoff's psychosis. The administration of glucose prior to thiamine can precipitate Korsakoff's syndrome, as seen in this case. In such patients, brain MRI frequently shows abnormal enhancement of the mammillary bodies & thallamus
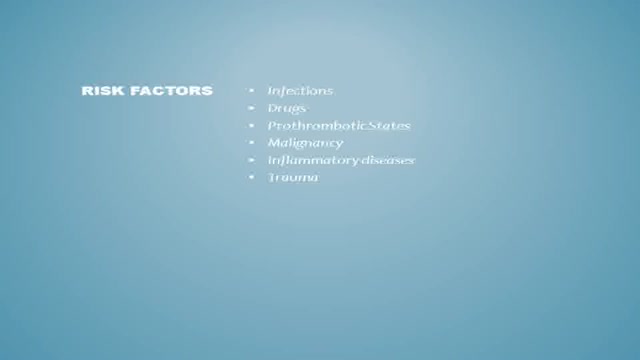
Thrombosis of the venous channels in the brain is an uncommon cause of cerebral infarction relative to arterial disease, but it is an important consideration because of its potential morbidity. (See Prognosis.) Knowledge of the anatomy of the venous system is essential in evaluating patients with cerebral venous thrombosis (CVT), since symptoms associated with the condition are related to the area of thrombosis. For example, cerebral infarction may occur with cortical vein or sagittal sinus thrombosis secondary to tissue congestion with obstruction. (See Presentation.) Lateral sinus thrombosis may be associated with headache and a pseudotumor cerebri–like picture. Extension into the jugular bulb may cause jugular foramen syndrome, while cranial nerve palsies may be seen in cavernous sinus thrombosis as a compressive phenomenon. Cerebral hemorrhage also may be a presenting feature in patients with venous sinus thrombosis. (See Presentation.) Imaging procedures have led to easier recognition of venous sinus thrombosis (see the images below), offering the opportunity for early therapeutic measures. (See Workup.) Left lateral sinus thrombosis demonstrated on magn Left lateral sinus thrombosis demonstrated on magnetic resonance venography (MRV). This 42-year-old woman presented with sudden onset of headache. Physical examination revealed no neurologic abnormalities. View Media Gallery Axial view of magnetic resonance (MR) venogram dem Axial view of magnetic resonance (MR) venogram demonstrating lack of flow in transverse sinus. View Media Gallery The following guidelines for CVT have been provided by the American Heart Association and the American Stroke Association [1] : In patients with suspected CVT, routine blood studies consisting of a complete blood count, chemistry panel, prothrombin time, and activated partial thromboplastin time should be performed. Screening for potential prothrombotic conditions that may predispose a person to CVT (eg, use of contraceptives, underlying inflammatory disease, infectious process) is recommended in the initial clinical assessment. Testing for prothrombotic conditions (including protein C, protein S, or antithrombin deficiency), antiphospholipid syndrome, prothrombin G20210A mutation, and factor V Leiden can be beneficial for the management of patients with CVT. Testing for protein C, protein S, and antithrombin deficiency is generally indicated 2-4 weeks after completion of anticoagulation. There is a very limited value of testing in the acute setting or in patients taking warfarin. In patients with provoked CVT (associated with a transient risk factor), vitamin K antagonists may be continued for 3-6 months, with a target international normalized ratio of 2.0-3.0. In patients with unprovoked CVT, vitamin K antagonists may be continued for 6-12 months, with a target international normalized ratio of 2.0-3.0. For patients with recurrent CVT, venous thromboembolism (VTE) after CVT, or first CVT with severe thrombophilia (ie, homozygous prothrombin G20210A; homozygous factor V Leiden; deficiencies of protein C, protein S, or antithrombin; combined thrombophilia defects; or antiphospholipid syndrome), indefinite anticoagulation may be considered, with a target international normalized ratio of 2.0-3.0. For women with CVT during pregnancy, low-molecular-weight heparin (LMWH) in full anticoagulant doses should be continued throughout pregnancy, and LMWH or vitamin K antagonist with a target international normalized ratio of 2.0-3.0 should be continued for ≥6 weeks postpartum (for a total minimum duration of therapy of 6 months). It is reasonable to advise women with a history of CVT that future pregnancy is not contraindicated. Further investigations regarding the underlying cause and a formal consultation with a hematologist or maternal fetal medicine specialist are reasonable. It is reasonable to treat acute CVT during pregnancy with full-dose LMWH rather than unfractionated heparin. For women with a history of CVT, prophylaxis with LMWH during future pregnancies and the postpartum period is reasonable. Next: Etiology What to Read Next on Medscape Related Conditions and Diseases Quiz: Do You Know the Complications, Proper Workup, and Best Treatment Practices for Ischemic Stroke? Quiz: How Much Do You Know About Hypothyroidism? Quiz: Do You Know the Risk Factors, Symptoms, and Potential Treatments for Alzheimer Disease? Quiz: How Much Do You Know About Hypertension? Quiz: Test Your Knowledge of Epilepsy and Seizure-related Conditions A 25-Year-Old Man With Painless Diplopia NEWS & PERSPECTIVE Temporal Trends and Factors Associated With Diabetes Mellitus Among Patients Hospitalized With Heart Failure Watchful Waiting Tied to Worse Outcomes in LVAD Patients With Hemolysis Age of Transfused Blood Impacts Perioperative Outcomes Among Patients Who Undergo Major Gastrointestinal Surgery TOOLS Drug Interaction Checker Pill Identifier Calculators Formulary SLIDESHOW Chronic Alcohol Abuse: Complications and Consequences Most Popular Articles According to Neurologists DHA Supplements Linked to Less Progression to Alzheimer's in APOE4 Carriers Heading in Soccer Linked to CNS Symptoms 'Transient Smartphone Blindness' Misdiagnosed as Multiple Sclerosis? New Advances in Traumatic Brain Injury FDA Clears Deflazacort (Emflaza) for DMD View More Overview Background
See the effects of cannabis first hand, unedited, on Parkinson's tremor dyskinesia, and voice.
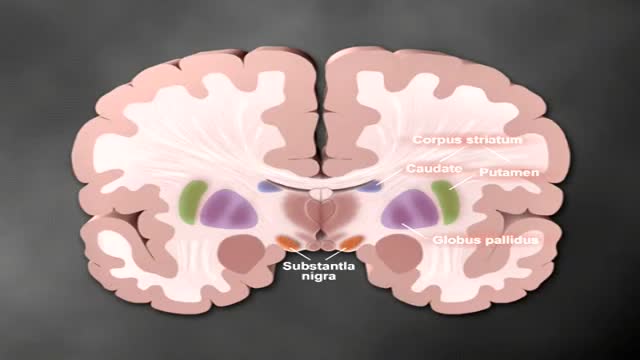
Both selegiline and rasagiline can improve the symptoms of Parkinson's disease, although their effects are small compared with levodopa. They can be used alongside levodopa or dopamine agonists. MAO-B inhibitors are generally very well tolerated, but can occasionally cause side effects, including: nausea.
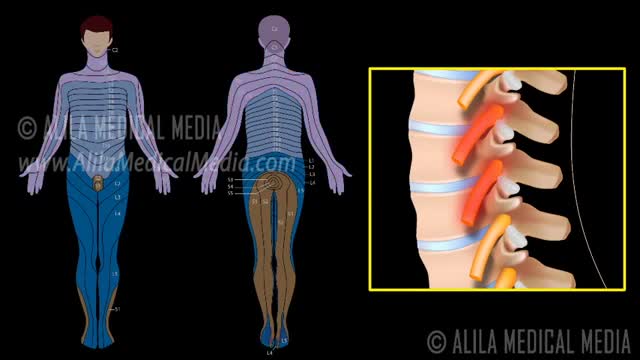
A nerve root block is an injection of local anesthetic (numbing medicine) and steroid injected under X-ray guidance into the area where the nerve exits the spinal column. A nerve root block is usually ordered by your doctor for pain in the arm or leg that follows the path of a single nerve. A nerve root block may be diagnostic (a test to determine the source of your pain) and/or therapeutic (to relieve your pain). If you get a period of sustained pain relief from the injection, the block may be repeated. Sometimes the block is done to help identify whether or not surgery might be helpful and at what level such surgery might be most helpful.
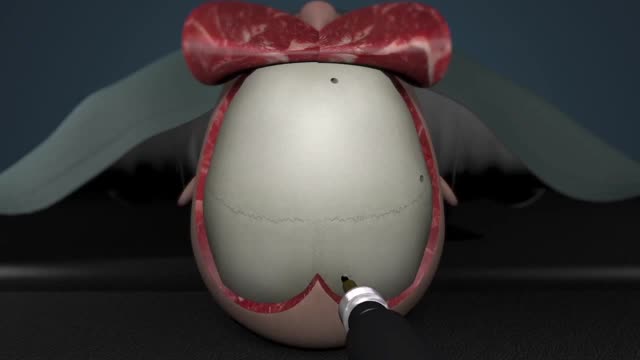
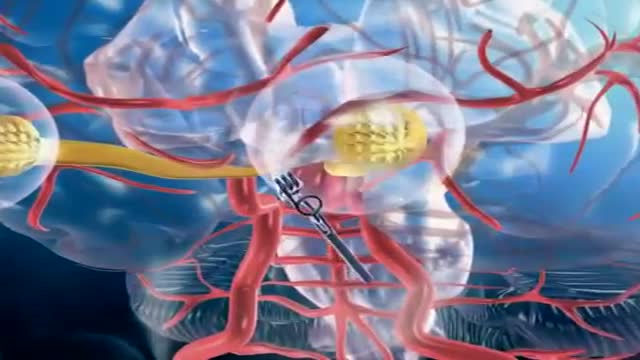
A craniotomy is the surgical removal of part of the bone from the skull to expose the brain. Specialized tools are used to remove the section of bone called the bone flap. The bone flap is temporarily removed, then replaced after the brain surgery has been done.
You may have a lot of questions about epilepsy. We will help you understand the basics, answer the most common questions, and help you find resources and other information you may need. However, information alone won’t help you manage your epilepsy and find a way to cope with the effects on your daily life. You’ll need to learn how to use the information and make it work for you.
How are seizures and epilepsy treated? What should I do if someone has a seizure? When seizure medications don't work, what else can be tried? These are just a few of the questions that you'll find answered here. Some treatment goals are common to everyone. Everyone should know what to do when a person is having a seizure. All people with seizures and their families should know that the real goal of treating epilepsy is to stop seizures or control them as best as possible. But you are more than just a seizure and how epilepsy affects you and your family may be different from someone else. Don't forget the most important goal of the Epilepsy Foundation - helping people with seizures and their families lead full and unrestricted lives according to their own wishes. Patient and doctor discussing treatment options"No seizures, no side effects" is the motto for epilepsy treatment. Not every person will reach that goal right now, but research and getting the "right care at the right time" can help more people achieve it each year. You may learn things here that can help you right away or later on. While seizure medicines are the mainstay of epilepsy treatment, there are other approaches to think about too. We hope these sections will help you learn about different treatments and get the help you need. Learn about the basics of Treatment 101 to help you get started. Look at Receiving Quality Care to see what to expect when you have just been diagnosed or after you have already started treatment. Then learn about specific treatments, what to do if seizures don't stop, and how to develop your health care team. You'll also find tools to help you manage your epilepsy or learn about research studies in other sections, so don't stop here!
Focal seizures (also called partial seizures [citation needed] and localized seizures) are seizures which affect initially only one hemisphere of the brain. [citation needed] The brain is divided into two hemispheres, each consisting of four lobes – the frontal, temporal, parietal and occipital lobes.
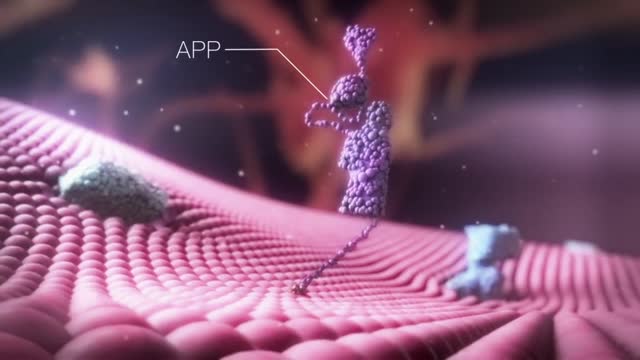
Three cholinesterase inhibitors are commonly prescribed: Donepezil (Aricept) is approved to treat all stages of Alzheimer's. Rivastigmine (Exelon) is approved to treat mild to moderate Alzheimer's. Galantamine (Razadyne) is approved to treat mild to moderate Alzheimer's. Currently, there is no cure for Alzheimer's. But drug and non-drug treatments may help with both cognitive and behavioral symptoms. Researchers are looking for new treatments to alter the course of the disease and improve the quality of life for people with dementia. ... Medications for Memory Loss.
Alzheimer's worsens over time. Alzheimer's is a progressive disease, where dementia symptoms gradually worsen over a number of years. In its early stages, memory loss is mild, but with late-stage Alzheimer's, individuals lose the ability to carry on a conversation and respond to their environment. Alzheimer's is the sixth leading cause of death in the United States. Those with Alzheimer's live an average of eight years after their symptoms become noticeable to others, but survival can range from four to 20 years, depending on age and other health conditions. Alzheimer's has no current cure, but treatments for symptoms are available and research continues. Although current Alzheimer's treatments cannot stop Alzheimer's from progressing, they can temporarily slow the worsening of dementia symptoms and improve quality of life for those with Alzheimer's and their caregivers. Today, there is a worldwide effort under way to find better ways to treat the disease, delay its onset, and prevent it from developing. Alzheimer's has no current cure, but treatments for symptoms are available and research continues. Although current Alzheimer's treatments cannot stop Alzheimer's from progressing, they can temporarily slow the worsening of dementia symptoms and improve quality of life for those with Alzheimer's and their caregivers. Today, there is a worldwide effort under way to find better ways to treat the disease, delay its onset, and prevent it from developing.
Alzheimer's is the most common form of dementia, a general term for memory loss and other intellectual abilities serious enough to interfere with daily life. Alzheimer's disease accounts for 60 to 80 percent of dementia cases. Alzheimer's is not a normal part of aging, although the greatest known risk factor is increasing age, and the majority of people with Alzheimer's are 65 and older. But Alzheimer's is not just a disease of old age. Up to 5 percent of people with the disease have early onset Alzheimer's (also known as younger-onset), which often appears when someone is in their 40s or 50s.
A brain (cerebral) aneurysm is a bulging, weak area in the wall of an artery that supplies blood to the brain. In most cases, a brain aneurysm causes no symptoms and goes unnoticed. In rare cases, the brain aneurysm ruptures, releasing blood into the skull and causing a stroke. When a brain aneurysm ruptures, the result is called a subarachnoid hemorrhage. Depending on the severity of the hemorrhage, brain damage or death may result. The most common location for brain aneurysms is in the network of blood vessels at the base of the brain called the circle of Willis. What causes a brain aneurysm? A person may inherit the tendency to form aneurysms, or aneurysms may develop because of hardening of the arteries (atherosclerosis) and aging. Some risk factors that can lead to brain aneurysms can be controlled, and others can't. The following risk factors may increase your risk for an aneurysm or, if you already have an aneurysm, may increase your risk of it rupturing: Family history. People who have a family history of brain aneurysms are more likely to have an aneurysm than those who don't. Previous aneurysm. People who have had a brain aneurysm are more likely to have another. Gender. Women are more likely to develop a brain aneurysm or to suffer a subarachnoid hemorrhage. Race. African Americans are more likely than whites to have a subarachnoid hemorrhage. High blood pressure. The risk of subarachnoid hemorrhage is greater in people who have a history of high blood pressure. Smoking. In addition to being a cause of high blood pressure, the use of cigarettes may greatly increase the chances of a brain aneurysm rupturing.
Parkinson's disease is a progressive disorder of the nervous system that affects movement. It develops gradually, sometimes starting with a barely noticeable tremor in just one hand. But while a tremor may be the most well-known sign of Parkinson's disease, the disorder also commonly causes stiffness or slowing of movement. In the early stages of Parkinson's disease, your face may show little or no expression, or your arms may not swing when you walk. Your speech may become soft or slurred. Parkinson's disease symptoms worsen as your condition progresses over time. Although Parkinson's disease can't be cured, medications may markedly improve your symptoms. In occasional cases, your doctor may suggest surgery to regulate certain regions of your brain and improve your symptoms.
Ca2+ binds with the membrane of the synaptic vesicles, which causes the vesicles to break and release the neurotransmitter into the synaptic cleft. After the neurotransmitters are released, they diffuse across the synaptic cleft and interact with receptors on the postsynaptic membrane. When the action potential reaches the presynaptic terminal, it provokes the release of a small quantity of neurotransmitter molecules, which bind to chemical receptor molecules located in the membrane of another neuron, the postsynaptic neuron, on the opposite side of the synaptic cleft.
Traumatic brain injury (TBI) is a nondegenerative, noncongenital insult to the brain from an external mechanical force, possibly leading to permanent or temporary impairment of cognitive, physical, and psychosocial functions, with an associated diminished or altered state of consciousness.
There are a number of different causes of vertigo. Vertigo can be defined based upon whether the cause is peripheral or central. Central causes of vertigo arise in the brain or spinal cord while peripheral vertigo is due to a problem within the inner ear. The inner ear can become inflamed because of illness, or small crystals or stones found normally within the inner ear can become displaced and cause irritation to the small hair cells within the semicircular canals, leading to vertigo. This is known as benign paroxysmal positional vertigo (BPPV).
Fibromyalgia syndrome (FMS) is a form of fibromyalgia where pain and stiffness occurs in muscles, tendons, and ligaments throughout the body, accompanied by other generalized symptoms such as fatigue, sleep disruption or unrefreshing sleep, mood disorder, and cognitive difficulties such as poor memory or mental ...
Memory Loss & the Brain. It's not just a movement disorder. Besides causing tremors and other motion-related symptoms, Parkinson's disease affects memory, learning, and behavior. Parkinson's disease is notorious for so-called motor symptoms like muscle rigidity, tremor, slowed movement, and unsteady posture and gait.