Neurology
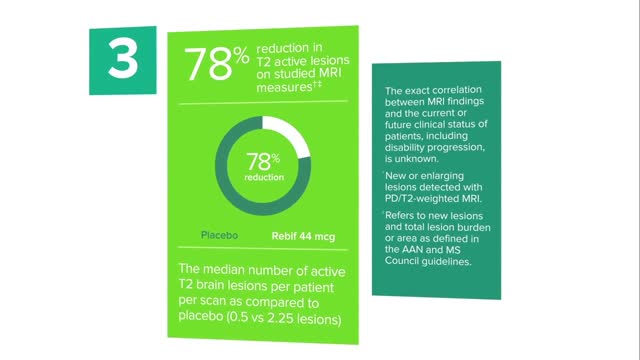
Doctors have many options to choose from, including interferon (Avonex, Betaseron, Extavia, and Rebif ), glatiramer acetate (Copaxone), mitoxantrone (Novantrone), teriflunomide (Aubagio), fingolimod (Gilenya), dimethyl fumarate (Tecfidera), and natalizumab (Tysabri).
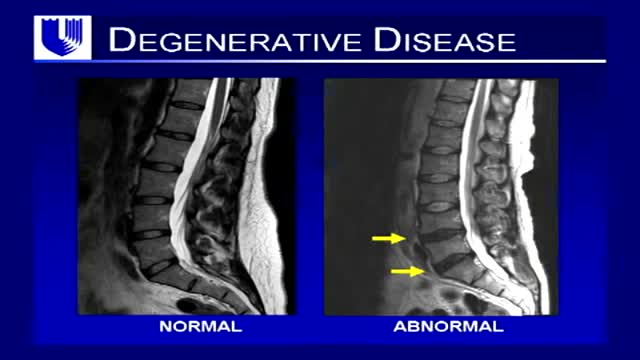
Neck pain is a common complaint. Neck muscles can be strained from poor posture — whether it's leaning over your computer or hunching over your workbench. Osteoarthritis also is a common cause of neck pain. Rarely, neck pain can be a symptom of a more serious problem. Seek medical care if your neck pain is accompanied by numbness or loss of strength in your arms or hands or if you have shooting pain into your shoulder or down your arm
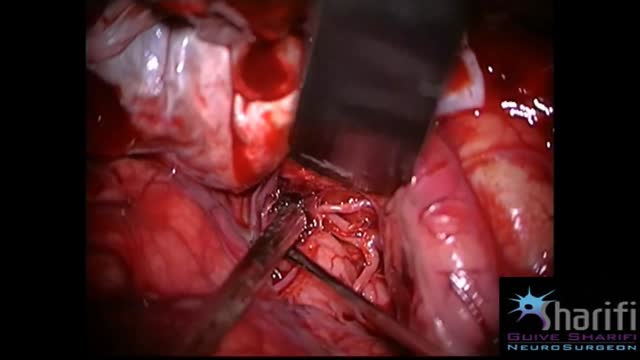
The goal of surgical clipping is to isolate an aneurysm from the normal circulation without blocking off any small perforating arteries nearby. Under general anesthesia, an opening is made in the skull, called a craniotomy. The brain is gently retracted to locate the aneurysm. A small clip is placed across the base, or neck, of the aneurysm to block the normal blood flow from entering. The clip works like a tiny coil-spring clothespin, in which the blades of the clip remain tightly closed until pressure is applied to open the blades. Clips are made of titanium and remain on the artery permanently.
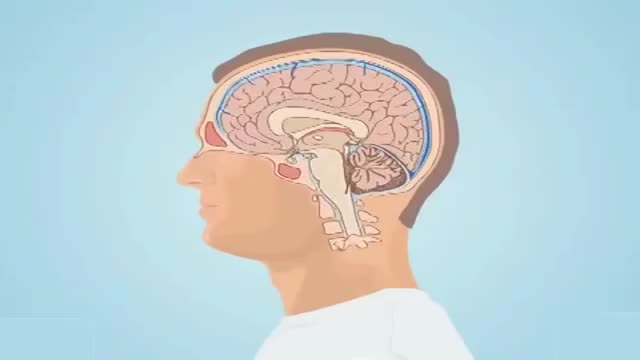
The term subarachnoid hemorrhage (SAH) refers to extravasation of blood into the subarachnoid space between the pial and arachnoid membranes. SAH constitutes half of all spontaneous atraumatic intracranial hemorrhages; the other half consists of bleeding that occurs within the brain parenchyma. Subarachnoid hemorrhage occurs in various clinical contexts, the most common being head trauma. However, the familiar use of the term SAH refers to nontraumatic (or spontaneous) hemorrhage, which usually occurs in the setting of a ruptured cerebral aneurysm or arteriovenous malformation (AVM).
Cluster headaches, which occur in cyclical patterns or clusters, are one of the most painful types of headache. A cluster headache commonly awakens you in the middle of the night with intense pain in or around one eye on one side of your head. Bouts of frequent attacks, known as cluster periods, can last from weeks to months, usually followed by remission periods when the headaches stop. During remission, no headaches occur for months and sometimes even years. Fortunately, cluster headache is rare and not life-threatening. Treatments can make cluster headache attacks shorter and less severe. In addition, medications can reduce the number of cluster headaches.
The pain is frequently severe and is described as throbbing or pulsating. Nausea is common, and many migraine patients have a watering eye, a running nose, or congestion. If these symptoms are prominent, they may lead to a misdiagnosis of sinus headaches.
Headache is pain in any region of the head. Headaches may occur on one or both sides of the head, be isolated to a certain location, radiate across the head from one point, or have a viselike quality. A headache may appear as a sharp pain, a throbbing sensation or a dull ache. Headaches can develop gradually or suddenly, and may last from less than an hour to several days
Your headache symptoms can help your doctor determine its cause and the appropriate treatment. Most headaches aren't the result of a serious illness, but some may result from a life-threatening condition requiring emergency care. Headaches are generally classified by cause: Primary headaches A primary headache is caused by overactivity of or problems with pain-sensitive structures in your head. A primary headache isn't a symptom of an underlying disease. Chemical activity in your brain, the nerves or blood vessels surrounding your skull, or the muscles of your head and neck (or some combination of these factors) can play a role in primary headaches. Some people may also carry genes that make them more likely to develop such headaches. The most common primary headaches are: Cluster headache Migraine (with and without aura) Tension headache (also known as tension-type headache) Trigeminal autonomic cephalalgia (TAC), such as cluster headache and paroxysmal hemicrania A few headache patterns also are generally considered types of primary headache, but are less common. These headaches have distinct features, such as an unusual duration or pain associated with a certain activity. Although generally considered primary, each could be a symptom of an underlying disease. They include: Chronic daily headaches (for example, chronic migraine, chronic tension-type headache, or hemicranias continua) Cough headaches Exercise headaches Sex headaches Some primary headaches can be triggered by lifestyle factors, including: Alcohol, particularly red wine Certain foods, such as processed meats that contain nitrates Changes in sleep or lack of sleep Poor posture Skipped meals Stress Secondary headaches A secondary headache is a symptom of a disease that can activate the pain-sensitive nerves of the head. Any number of conditions — varying greatly in severity — may cause secondary headaches. Possible causes of secondary headaches include: Acute sinusitis Arterial tears (carotid or vertebral dissections) Blood clot (venous thrombosis) within the brain — separate from stroke Brain aneurysm (a bulge in an artery in your brain) Brain AVM (brain arteriovenous malformation) — an abnormal formation of brain blood vessels Brain tumor Carbon monoxide poisoning Chiari malformation (structural problem at the base of your skull) Concussion Dehydration Dental problems Ear infection (middle ear) Encephalitis (brain inflammation) Giant cell arteritis (inflammation of the lining of the arteries) Glaucoma (acute angle closure glaucoma) Hangovers
Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. You may have sleep apnea if you snore loudly, and you feel tired even after a full night's sleep. The main types of sleep apnea are: Obstructive sleep apnea, the more common form that occurs when throat muscles relax. Central sleep apnea, which occurs when your brain doesn't send proper signals to the muscles that control breathing. Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea. If you think you might have any form of sleep apnea, see your doctor. Treatment can ease your symptoms and may help prevent heart problems and other complications.
A dream is a succession of images, ideas, emotions, and sensations that usually occurs involuntarily in the mind during certain stages of sleep.[1] The content and purpose of dreams are not definitively understood, though they have been a topic of scientific speculation, as well as a subject of philosophical and religious interest, throughout recorded history. The scientific study of dreams is called oneirology
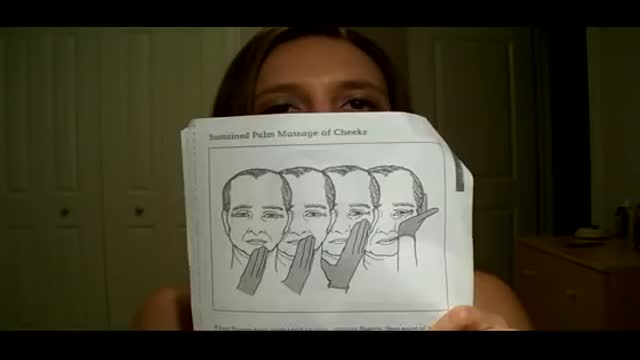
Bell's palsy is a form of facial paralysis resulting from damage or trauma to the facial nerves. The facial nerve-also called the 7th cranial nerve-travels through a narrow, bony canal (called the Fallopian canal) in the skull, beneath the ear, to the muscles on each side of the face. For most of its journey, the nerve is encased in this bony shell. Each facial nerve directs the muscles on one side of the face, including those that control eye blinking and closing, and facial expressions such as smiling and frowning. Additionally, the facial nerve carries nerve impulses to the lacrimal or tear glands, the saliva glands, and the muscles of a small bone in the middle of the ear called the stapes. The facial nerve also transmits taste sensations from the tongue. When Bell's palsy occurs, the function of the facial nerve is disrupted, causing an interruption in the messages the brain sends to the facial muscles. This interruption results in facial weakness or paralysis. Bell's palsy is named for Sir Charles Bell, a 19th century Scottish surgeon who described the facial nerve and its connection to the condition. The disorder, which is not related to stroke, is the most common cause of facial paralysis. Generally, Bell's palsy affects only one of the paired facial nerves and one side of the face, however, in rare cases, it can affect both sides.
Bell's palsy is a form of temporary facial paralysis resulting from damage or trauma to the facial nerves. The facial nerve-also called the 7th cranial nerve-travels through a narrow, bony canal (called the Fallopian canal) in the skull, beneath the ear, to the muscles on each side of the face. For most of its journey, the nerve is encased in this bony shell. Each facial nerve directs the muscles on one side of the face, including those that control eye blinking and closing, and facial expressions such as smiling and frowning. Additionally, the facial nerve carries nerve impulses to the lacrimal or tear glands, the saliva glands, and the muscles of a small bone in the middle of the ear called the stapes. The facial nerve also transmits taste sensations from the tongue. When Bell's palsy occurs, the function of the facial nerve is disrupted, causing an interruption in the messages the brain sends to the facial muscles. This interruption results in facial weakness or paralysis. Bell's palsy is named for Sir Charles Bell, a 19th century Scottish surgeon who described the facial nerve and its connection to the condition. The disorder, which is not related to stroke, is the most common cause of facial paralysis. Generally, Bell's palsy affects only one of the paired facial nerves and one side of the face, however, in rare cases, it can affect both sides.
A traumatic brain injury (TBI) is defined as a blow or jolt to the head, or a penetrating head injury that disrupts the normal function of the brain. TBI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue. Symptoms of a TBI can be mild, moderate or severe, depending on the extent of damage to the brain. Mild cases (mild traumatic brain injury, or mTBI) may result in a brief change in mental state or consciousness, while severe cases may result in extended periods of unconsciousness, coma or even death. The 4th International Conference on Concussion in Sport held in Zurich, Switzerland in 2012 defined concussion, a subset of mTBI, as the following: Concussion is the historical term representing low velocity injuries that cause brain ‘shaking’ resulting in clinical symptoms and that are not necessarily related to a pathological injury. Concussion is a subset of TBI and will be the term used in this document. It was also noted that the term commotio cerebri is often used in European and other countries. Minor revisions were made to the definition of concussion, which is defined as follows: Concussion is a brain injury and is defined as a complex pathophysiological process affecting the brain, induced by biomechanical forces. Several common features that incorporate clinical, pathologic and biomechanical injury constructs that may be utilised in defining the nature of a concussive head injury include: 1. Concussion may be caused either by a direct blow to the head, face, neck or elsewhere on the body with an "impulsive" force transmitted to the head. 2. Concussion typically results in the rapid onset of short-lived impairment of neurological function that resolves spontaneously. However, in some cases, symptoms and signs may evolve over a number of minutes to hours. 3. Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury and, as such, no abnormality is seen on standard structural neuroimaging studies. 4. Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. However, it is important to note that in some cases symptoms may be prolonged. To view peer reviewed literature related to sports concussions, the Sports Concussion Library can be found here. Incidence The U.S. Consumer Product Safety Commission (CPSC) tracks product-related injuries through its National Electronic Injury Surveillance System (NEISS). According to CPSC data, there were an estimated 446,788 sports-related head injuries treated at U.S. hospital emergency rooms in 2009. This number represents an increase of nearly 95,000 sports-related injuries from the prior year. All of the 20 sports noted below posted increases in the number of injuries treated in 2009, except for trampolines, which posted 52 fewer injuries in 2009. Sports that exhibited substantial increases from 2008 to 2009 included water sports (11,239 to 28,716*), cycling (70,802 to 85,389), baseball and softball (26,964 to 38,394) and basketball (27,583 to 34,692). *Four categories were tabulated by the AANS in the current analysis that were not reflected in the 2008 injury data analysis, but together, these account for only 1,397 injuries. The actual incidence of head injuries may potentially be much higher for two primary reasons. 1). In the 2009 report, the CPSC excluded estimates for product categories that yielded 1,200 injuries or less, those that had very small sample counts and those that were limited to a small geographic area of the country; 2). Many less severe head injuries are treated at physician's offices or immediate care centers, or are self-treated. Included in these statistics are not only the sports/recreational activities, but the equipment and apparel used in these activities. For example, swimming-related injuries include the activity as well as diving boards, equipment, flotation devices, pools and water slides. The following 20 sports/recreational activities represent the categories contributing to the highest number of estimated head injuries treated in U.S. hospital emergency rooms in 2009.
A sleep disorder, or somnipathy, is a medical disorder of the sleep patterns of a person or animal. Some sleep disorders are serious enough to interfere with normal physical, mental, social and emotional functioning. Polysomnography and actigraphy are tests commonly ordered for some sleep disorders.
Subarachnoid hemorrhage is bleeding in the space between your brain and the surrounding membrane (subarachnoid space). Bleeding usually results from the rupture of an abnormal bulge in a blood vessel in your brain (brain aneurysm). Sometimes an abnormal tangle of blood vessels in your brain (arteriovenous malformation), trauma or other events cause bleeding. A subarachnoid hemorrhage may lead to permanent brain damage or death if not treated.
What is idiopathic intracranial hypertension??? Idiopathic intracranial hypertension (IIH) is a disorder that results from an increase in the pressure of the Cerebro-Spinal Fluid (CSF) that cushions and protects the brain and spinal cord. The CSF is constantly produced in the brain and reabsorbed back into the bloodstream at a fairly constant rate. This allows the fluid pressure around the brain to remain constant. What are the symptoms of idiopathic intracranial hypertension? Headaches that are generally nonspecific in location, type and frequency and can be associated with nausea and vomiting. Pulsatile tinnitus is a rhythmic or pulsating ringing heard in one or both ears. Horizontal double vision can be a sign of pressure on the 6th cranial nerve(s). Nonspecific radiating pain in the arms or legs (radicular pain). Transient obscurations of vision (TOV), which are temporary dimming or complete blacking out of vision. Visual field defects. These defects can occur in the central as well as the peripheral vision. Loss of color vision. What causes idiopathic intracranial hypertension? The cause is usually not known. A common explanation for increased pressure is a problem with the reabsorption of this fluid back into the body, which causes the pressure to increase. Sometimes the cause is determined and is referred to as “secondary” intracranial hypertension.
What is idiopathic intracranial hypertension? Idiopathic intracranial hypertension (IIH) is a disorder that results from an increase in the pressure of the Cerebro-Spinal Fluid (CSF) that cushions and protects the brain and spinal cord. The CSF is constantly produced in the brain and reabsorbed back into the bloodstream at a fairly constant rate. This allows the fluid pressure around the brain to remain constant. What are the symptoms of idiopathic intracranial hypertension? Headaches that are generally nonspecific in location, type and frequency and can be associated with nausea and vomiting. Pulsatile tinnitus is a rhythmic or pulsating ringing heard in one or both ears. Horizontal double vision can be a sign of pressure on the 6th cranial nerve(s). Nonspecific radiating pain in the arms or legs (radicular pain). Transient obscurations of vision (TOV), which are temporary dimming or complete blacking out of vision. Visual field defects. These defects can occur in the central as well as the peripheral vision. Loss of color vision. What causes idiopathic intracranial hypertension? The cause is usually not known. A common explanation for increased pressure is a problem with the reabsorption of this fluid back into the body, which causes the pressure to increase. Sometimes the cause is determined and is referred to as “secondary” intracranial hypertension.
Absence seizures involve brief, sudden lapses of consciousness. They're more common in children than adults. Someone having an absence seizure may look like he or she is staring into space for a few seconds. This type of seizure usually doesn't lead to physical injury. Absence seizures usually can be controlled with anti-seizure medications. Some children who have them also develop other seizures. Many children outgrow absence seizures in their teens.
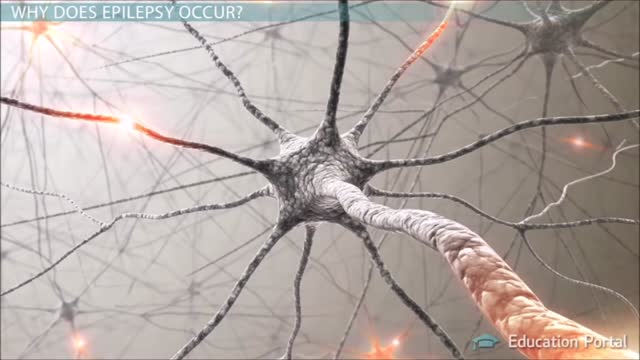
A seizure occurs when there’s abnormal electrical activity in the brain. Seizures may go virtually unnoticed. Or, in severe cases, they may produce a change or loss of consciousness and involuntary muscle spasms called convulsions. Seizures usually come on suddenly and vary in duration and severity. A seizure may be a one-time event, or you may have seizures repeatedly. Recurrent seizures are called epilepsy, or a seizure disorder. Less than one in 10 people who has a seizure develops epilepsy. Experts classify seizures into two general categories and many subtypes based on the pattern of the attack. Generalized seizures involve both sides of the brain from the start of the attack. Common subtypes include tonic-clonic (grand mal) and absence seizures (petit mal). Febrile and infantile spasms are two types of generalized seizures that occur almost exclusively in young children. Partial (or focal) seizures are the second major seizure type. These begin in a specific area of the brain and may be contained there. Or they may spread to the entire brain. With simple partial seizures, the person remains conscious. Complex partial seizures involve impaired consciousness. What Causes Seizures? Often the cause of a seizure is unknown. Many conditions can provoke seizures, including: Stroke Brain tumors Head injuries Electrolyte imbalance Very low blood sugar Repetitive sounds or flashing lights, such as in video games Medications, such as antipsychotics and some asthma drugs Withdrawal from medications, such as Xanax, narcotics, or alcohol Use of drugs such as cocaine and heroin Cancer Brain infections, such as meningitis
Epilepsy is a chronic disorder, the hallmark of which is recurrent, unprovoked seizures. Many people with epilepsy have more than one type of seizure and may have other symptoms of neurological problems as well. Sometimes EEG testing, clinical history, family history and outlook are similar among a group of people with epilepsy. In these situations, their condition can be defined as a specific epilepsy syndrome. The human brain is the source of human epilepsy. Although the symptoms of a seizure may affect any part of the body, the electrical events that produce the symptoms occur in the brain. The location of that event, how it spreads and how much of the brain is affected, and how long it lasts all have profound effects. These factors determine the character of a seizure and its impact on the individual. Esssentially, anything the brain can do, it can do in the form of a seizure. Having seizures and epilepsy can affect one's safety, relationships, work, driving and so much more. Public perception and treatment of people with epilepsy are often bigger problems than actual seizures.