Neurology
Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo — the sudden sensation that you're spinning or that the inside of your head is spinning. Benign paroxysmal positional vertigo causes brief episodes of mild to intense dizziness. Benign paroxysmal positional vertigo is usually triggered by specific changes in the position of your head. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed. Although benign paroxysmal positional vertigo can be a bothersome problem, it's rarely serious except when it increases the chance of falls. You can receive effective treatment for benign paroxysmal positional vertigo during a doctor's office visit
Epley maneuver: Step 1 You will sit on the doctor's exam table with your legs extended in front of you. The doctor will turn your head so that it is halfway between looking straight ahead and looking directly to the side that causes the worst vertigo. Without changing your head position, the doctor will guide you back quickly so that your shoulders are on the table but your head is hanging over the edge of the table. In this position, the side of your head that is causing the worst vertigo is facing the floor. The doctor will hold you in this position for 30 seconds or until your vertigo stops. Epley maneuver: Step 2 Then, without lifting up your head, the doctor will turn your head to look at the same angle to the opposite side, so that the other side of your head is now facing the floor. The doctor will hold you in this position for 30 seconds or until your vertigo stops. Epley maneuver: Step 3 The doctor will help you roll in the same direction you are facing so that you are now lying on your side. (For example, if you are looking to your right, you will roll onto your right side.) The side that causes the worst vertigo should be facing up. The doctor will hold you in this position for another 30 seconds or until your vertigo stops. Epley maneuver: Step 4 The doctor will then help you to sit back up with your legs hanging off the table on the same side that you were facing. This maneuver is done with the assistance of a doctor or physical therapist. A single 10- to 15-minute session usually is all that is needed. When your head is firmly moved into different positions, the crystal debris (canaliths) causing vertigo will move freely and no longer cause symptoms.
Vertigo is a sensation of spinning. If you have these dizzy spells, you might feel like you are spinning or that the world around you is spinning. Causes of Vertigo Vertigo is often caused by an inner ear problem. Some of the most common causes include: BPPV. These initials stand for benign paroxysmal positional vertigo. BPPV occurs when tiny calcium particles (canaliths) clump up in canals of the inner ear. The inner ear sends signals to the brain about head and body movements relative to gravity. It helps you keep your balance. BPPV can occur for no known reason and may be associated with age. Meniere's disease. This is an inner ear disorder thought to be caused by a buildup of fluid and changing pressure in the ear. It can cause episodes of vertigo along with ringing in the ears (tinnitus) and hearing loss. Vestibular neuritis or labyrinthitis. This is an inner ear problem usually related to infection (usually viral). The infection causes inflammation in the inner ear around nerves that are important for helping the body sense balance
Fainting occurs when the blood supply to your brain is momentarily inadequate, causing you to lose consciousness. This loss of consciousness is usually brief. Fainting can have no medical significance, or the cause can be a serious disorder. Therefore, treat loss of consciousness as a medical emergency until the signs and symptoms are relieved and the cause is known. Discuss recurrent fainting spells with your doctor. If you feel faint Lie down or sit down. To reduce the chance of fainting again, don't get up too quickly. Place your head between your knees if you sit down. If someone else faints Position the person on his or her back. If the person is breathing, restore blood flow to the brain by raising the person's legs above heart level — about 12 inches (30 centimeters) — if possible. Loosen belts, collars or other constrictive clothing. To reduce the chance of fainting again, don't get the person up too quickly. If the person doesn't regain consciousness within one minute, call 911 or your local emergency number. Check the person's airway to be sure it's clear. Watch for vomiting. Check for signs of circulation (breathing, coughing or movement). If absent, begin CPR. Call 911 or your local emergency number. Continue CPR until help arrives or the person responds and begins to breathe.
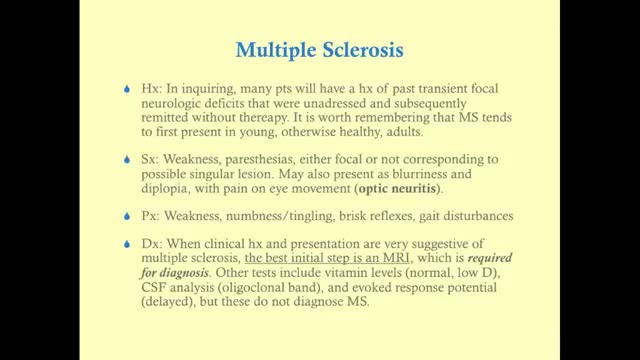
Multiple Sclerosis Multiple sclerosis (MS) affects the brain and spinal cord. Early MS symptoms include weakness, tingling, numbness, and blurred vision. Other signs are muscle stiffness, thinking problems, and urinary problems. Treatment can relieve MS symptoms and delay disease progression.
Multiple sclerosis (MS) affects the brain and spinal cord. Early MS symptoms include weakness, tingling, numbness, and blurred vision. Other signs are muscle stiffness, thinking problems, and urinary problems. Treatment can relieve MS symptoms and delay disease progression.
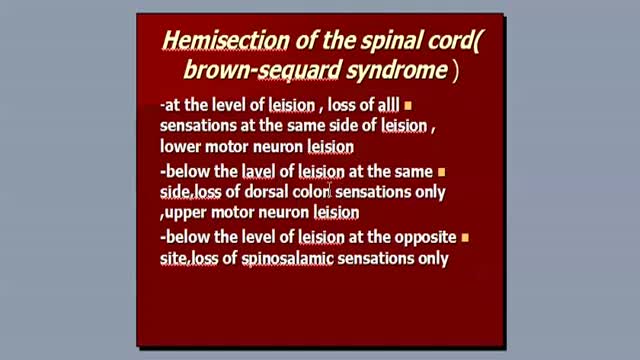
Brown-Séquard syndrome is an incomplete spinal cord lesion characterized by a clinical picture reflecting hemisection injury of the spinal cord, often in the cervical cord region. (See Presentation.) Patients with Brown-Séquard syndrome suffer from ipsilateral upper motor neuron paralysis and loss of proprioception, as well as contralateral loss of pain and temperature sensation. A zone of partial preservation or segmental ipsilateral lower motor neuron weakness and analgesia may be noted. Loss of ipsilateral autonomic function can result in Horner syndrome. (See Etiology, Presentation, and Workup.) As an incomplete spinal cord syndrome, the clinical presentation of Brown-Séquard syndrome may range from mild to severe neurologic deficit. (See Presentation.) Brown-Séquard–plus syndrome The pure Brown-Séquard syndrome reflecting hemisection of the cord is not often observed. A clinical picture composed of fragments of the syndrome or of the hemisection syndrome plus additional symptoms and signs is more common. These less-pure forms of the disorder are often referred to as Brown-Séquard–plus syndrome.[1] Interruption of the lateral corticospinal tracts, the lateral spinal thalamic tract, and at times the posterior columns produces a picture of a spastic, weak leg with brisk reflexes and a strong leg with loss of pain and temperature sensation. Note that spasticity and hyperactive reflexes may not be present with an acute lesion.
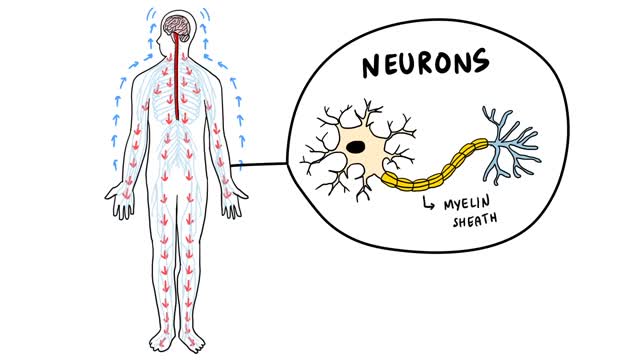
Guillain-Barre syndrome is a rare disorder in which your body's immune system attacks your nerves. Weakness and tingling in your extremities are usually the first symptoms. These sensations can quickly spread, eventually paralyzing your whole body. In its most severe form Guillain-Barre syndrome is a medical emergency. Most people with the condition must be hospitalized to receive treatment. The exact cause of Guillain-Barre syndrome is unknown. But it is often preceded by an infectious illness such as a respiratory infection or the stomach flu. There's no known cure for Guillain-Barre syndrome, but several treatments can ease symptoms and reduce the duration of the illness. Most people recover from Guillain-Barre syndrome, though some may experience lingering effects from it, such as weakness, numbness or fatigue.
Guillain-Barre (gee-YAH-buh-RAY) syndrome is a rare disorder in which your body's immune system attacks your nerves. Weakness and tingling in your extremities are usually the first symptoms. These sensations can quickly spread, eventually paralyzing your whole body. In its most severe form Guillain-Barre syndrome is a medical emergency. Most people with the condition must be hospitalized to receive treatment. The exact cause of Guillain-Barre syndrome is unknown. But it is often preceded by an infectious illness such as a respiratory infection or the stomach flu. There's no known cure for Guillain-Barre syndrome, but several treatments can ease symptoms and reduce the duration of the illness. Most people recover from Guillain-Barre syndrome, though some may experience lingering effects from it, such as weakness, numbness or fatigue.
Friedreich's ataxia is an inherited disease that damages your nervous system. The damage affects your spinal cord and the nerves that control muscle movement in your arms and legs. Symptoms usually begin between the ages of 5 and 15. The main symptom is ataxia, which means trouble coordinating movements. Specific symptoms include Difficulty walking Muscle weakness Speech problems Involuntary eye movements Scoliosis (curving of the spine to one side) Heart palpitations, from the heart disease which can happen along with Friedreich's ataxia People with Friedreich's ataxia usually need a wheelchair 15 to 20 years after symptoms first appear. In severe cases, people become incapacitated. There is no cure. You can treat symptoms with medicines, braces, surgery, and physical therapy.
Migraine treatments can help stop symptoms and prevent future attacks. Many medications have been designed to treat migraines. Some drugs often used to treat other conditions also may help relieve or prevent migraines. Medications used to combat migraines fall into two broad categories: Pain-relieving medications. Also known as acute or abortive treatment, these types of drugs are taken during migraine attacks and are designed to stop symptoms. Preventive medications. These types of drugs are taken regularly, often on a daily basis, to reduce the severity or frequency of migraines. Your treatment strategy depends on the frequency and severity of your headaches, the degree of disability your headaches cause, and your other medical conditions. Some medications aren't recommended if you're pregnant or breast-feeding. Some medications aren't given to children. Your doctor can help find the right medication for you
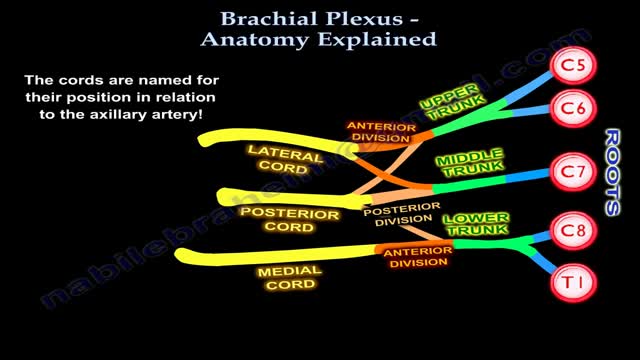
The brachial plexus is the network of nerves that sends signals from your spine to your shoulder, arm and hand. A brachial plexus injury occurs when these nerves are stretched, compressed, or in the most serious cases, ripped apart or torn away from the spinal cord. Minor brachial plexus injuries, known as stingers or burners, are common in contact sports, such as football. Babies sometimes sustain brachial plexus injuries during birth. Other conditions, such as inflammation or tumors, may affect the brachial plexus. The most severe brachial plexus injuries usually result from auto or motorcycle accidents. Severe brachial plexus injuries can leave your arm paralyzed, with a loss of function and sensation. Surgical procedures such as nerve grafts, nerve transfers or muscle transfers can help restore function.
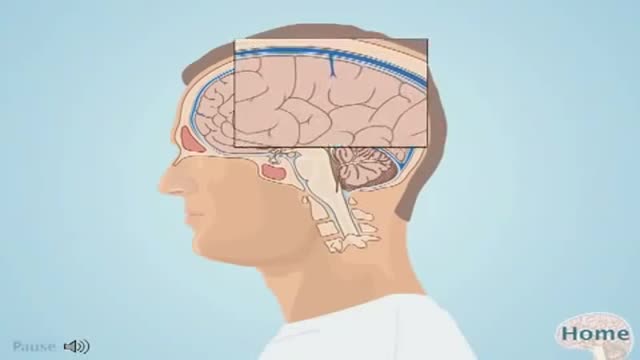
What is an Aneurysm? A cerebral or intracranial aneurysm is an abnormal focal dilation of an artery in the brain that results from a weakening of the inner muscular layer (the intima) of a blood vessel wall. The vessel develops a "blister-like" dilation that can become thin and rupture without warning. The resultant bleeding into the space around the brain is called a subarachnoid hemorrhage (SAH). This kind of hemorrhage can lead to a stroke, coma, and/or death. Aneurysms are usually found at the base of the brain just inside the skull, in an area called the subarachnoid space. In fact, 90 percent of SAHs are attributed to ruptured cerebral aneurysms and the two terms are often used synonymously.
intracranial hematoma occurs when a blood vessel ruptures within your brain or between your skull and your brain. The collection of blood (hematoma) compresses your brain tissue. An intracranial hematoma may occur because the fluid that surrounds your brain can't absorb the force of a sudden blow or a quick stop. Then your brain may slide forcefully against the inner wall of your skull and become bruised. Although some head injuries — such as one that causes only a brief lapse of consciousness (concussion) — can be minor, an intracranial hematoma is potentially life-threatening and often requires immediate treatment. An intracranial hematoma often, but not always, requires surgery to remove the blood.
An intracranial hematoma occurs when a blood vessel ruptures within your brain or between your skull and your brain. The collection of blood (hematoma) compresses your brain tissue. An intracranial hematoma may occur because the fluid that surrounds your brain can't absorb the force of a sudden blow or a quick stop. Then your brain may slide forcefully against the inner wall of your skull and become bruised. Although some head injuries — such as one that causes only a brief lapse of consciousness (concussion) — can be minor, an intracranial hematoma is potentially life-threatening and often requires immediate treatment. An intracranial hematoma often, but not always, requires surgery to remove the blood.
Medial medullary syndrome, also known as Dejerine syndrome, represents less than 1% of brainstem stroke syndromes. Thrombotic or embolic occlusion of small perforating branches from vertebral or proximal basilar artery supplying the medial aspect of medulla oblongata cause this rare syndrome. It is characterized by contralateral hemiplegia/hemiparesis as well as hemisensory loss with ipsilateral hypoglossal palsy (ipsilateral tongue weakness and atrophy) from involvement of CN XII nucleus. Other manifestations e.g. vertigo, nausea, ipsilateral limb ataxia are also reported.
What is Wallenberg syndrome? Wallenberg syndrome is a rare condition in which an infarction, or stroke, occurs in the lateral medulla. The lateral medulla is a part of the brain stem. Oxygenated blood doesn’t get to this part of the brain when the arteries that lead to it are blocked. A stroke can occur due to this blockage. This condition is also sometimes called lateral medullary infarction. The cause of the syndrome isn’t always clear, however.
Middle cerebral artery syndrome is a condition whereby the blood supply from the middle cerebral artery (MCA) is restricted, leading to a reduction of the function of the portions of the brain supplied by that vessel: the lateral aspects of frontal, temporal and parietal lobes, the corona radiata, globus pallidus, caudate and putamen. The MCA is the most common site for the occurrence of ischemic stroke.[1] Depending upon the location and severity of the occlusion, signs and symptoms may vary within the population affected with MCA syndrome. More distal blockages tend to produce milder deficits due to more extensive branching of the artery and less ischemic response. In contrast, the most proximal occlusions result in widespread effects that can lead to significant cerebral edema, increased intracranial pressure, loss of consciousness and could even be fatal.[1] In such occasions, mannitol (osmotic diuretic) or hypertonic saline are given to draw fluid out of the oedematus cerebrum to minimise secondary injury. Hypertonic saline is better than mannitol, as mannitol being a diuretic will decrease the mean arterial pressure and since cerebral perfusion is mean arterial pressure minus intracranial pressure, mannitol will also cause a decrease in cerebral perfusion. Contralateral hemiparesis and hemisensory loss of the face, upper and lower extremities is the most common presentation of MCA syndrome.[1] Lower extremity function is more spared than that of the faciobrachial region.[2] The majority of the primary motor and somatosensory cortices are supplied by the MCA and the cortical homunculus can, therefore, be used to localize the defects more precisely.it is important to note that middle cerebral artery lesions mostly affect the dominant hemisphere i.e. the left cerebral hemisphere.
LBD is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known diseases like Alzheimer’s and Parkinson’s, it is currently widely underdiagnosed. Many doctors or other medical professionals still are not familiar with LBD. LBD is an umbrella term for two related diagnoses. LBD refers to both Parkinson’s disease dementia and dementia with Lewy bodies. The earliest symptoms of these two diseases differ, but reflect the same underlying biological changes in the brain. Over time, people with both diagnoses will develop very similar cognitive, physical, sleep, and behavioral symptoms. While it may take more than a year or two for enough symptoms to develop for a doctor to diagnose LBD, it is critical to pursue a formal diagnosis. Early diagnosis allows for important early treatment that may extend quality of life and independence. LBD is a multisystem disease and typically requires a comprehensive treatment approach. This approach involves a team of physicians from different specialties who collaborate to provide optimum treatment of each symptom without worsening other LBD symptoms. Many people with LBD enjoy significant improvement of their symptoms with a comprehensive approach to treatment, and some can have remarkably little change from year to year. Some people with LBD are extremely sensitive or may react negatively to certain medications used to treat Alzheimer’s or Parkinson’s in addition to certain over-the-counter medications.
Parkinson disease (PD) is a common neurodegenerative condition. Typically beginning in the sixth or seventh decade of life, it is characterized by the unilateral onset of resting tremor in combination with varying degrees of rigidity and bradykinesia. PD was originally described by James Parkinson (1755-1824), a man of many talents and interests. Parkinson published works on chemistry, paleontology, and other diverse topics. Early in his career he was a social activist championing the rights of the disenfranchised and poor. His efforts in this area were enough to result in his arrest and appearance before the Privy Council in London on at least one occasion. In collaboration with his son, who was a surgeon, he also offered the first description in the English language of a ruptured appendix. His small but famous publication, "Essay on the Shaking Palsy," was published in 1817, seven years before his death. The clinical descriptions of 6 cases was remarkable in part because he never actually examined the people he described. Instead, he had simply observed these people on the streets of London.