Gastroenterology
Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism. The liver carries out several necessary functions, including detoxifying harmful substances in your body, cleaning your blood and making vital nutrients.Apr 6, 2016
Bengmark Naso-Intestinal tube
How to Reverse GERD and Leaky Gut
Experts do not know the exact cause of Zollinger-Ellison syndrome. About 25 to 30 percent of gastrinomas are caused by an inherited genetic disorder called multiple endocrine neoplasia type 1 (MEN1). MEN1 causes hormone-releasing tumors in the endocrine glands and the duodenum.
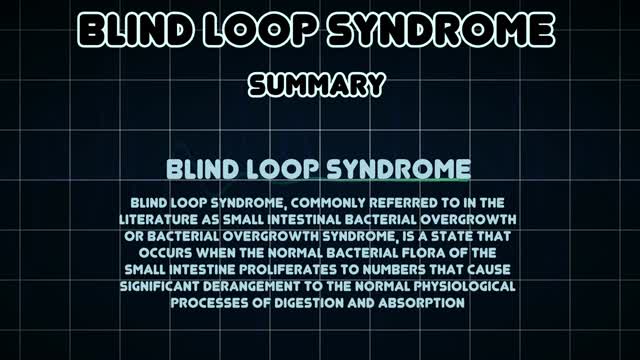
Blind loop syndrome (BLS), commonly referred to in the literature as small intestinal bacterial overgrowth (SIBO) or bacterial overgrowth syndrome (BOS), is a state that occurs when the normal bacterial flora of the small intestine proliferates to numbers that cause significant derangement to the normal physiological ...
The symptoms of bacterial overgrowth include nausea, flatus, constipation, bloating, abdominal distension, abdominal pain or discomfort, diarrhea, fatigue, and weakness. SIBO also causes an increased permeability of the small intestine. Some patients may lose weight.
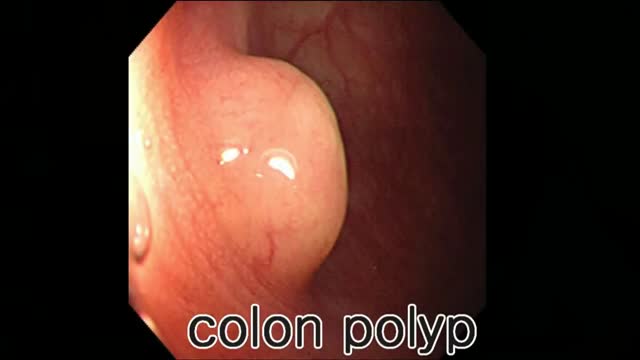
Juvenile polyposis syndrome (JPS) is a hereditary condition that is characterized by the presence of hamartomatous polyps in the digestive tract. Hamartomas are noncancerous (benign) masses of normal tissue that build up in the intestines or other places. These masses are called polyps if they develop inside a body structure, such as the intestines. The term “juvenile polyposis” refers to the type of polyp (juvenile polyp) that is found after examination of the polyp under a microscope, not the age at which people are diagnosed with JPS.
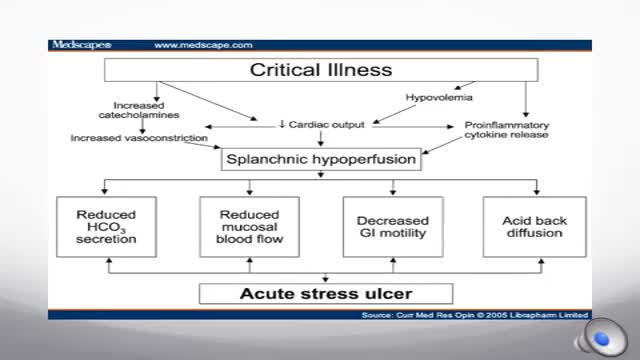
Stress-related mucosal disease (SRMD) is an acute, erosive gastritis representing conditions ranging from stress-related injury to stress ulcers (1, 2). Stress-related injury is superficial mucosal damage that presents primarily as erosions, whereas stress ulcers are deep, focal mucosal damage penetrating the submucosa with high risk for gastrointestinal bleeding (2, 3). Mucosal damage has been reported to occur during the first 24 hours of hospital admission in 75% to 100% of intensive care unit (ICU) patients (4, 5). Clinically important gastrointestinal bleeding can cause hemodynamic instability and increase the need for red blood cell transfusions (1). Significant bleeding may also increase the length of stay in the ICU and mortality (1).
A stress ulcer is a single or multiple mucosal defect which can become complicated by upper gastrointestinal bleeding during the physiologic stress of serious illness.
Gastroparesis -- literally “paralyzed stomach” -- is a serious condition manifested by delayed emptying of stomach contents into the small intestine after a meal. There is no cure for gastroparesis, but treatment can speed gastric emptying and relieve gastrointestinal symptoms such as nausea and vomiting.
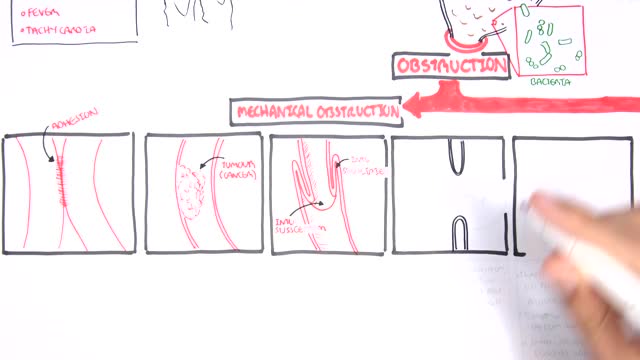
A small-bowel obstruction (SBO) is caused by a variety of pathologic processes. The leading cause of SBO in industrialized countries is postoperative adhesions (60%), followed by malignancy, Crohn disease, and hernias, although some studies have reported Crohn disease as a greater etiologic factor than neoplasia.
Gallstone ileus is an important, though infrequent, cause of mechanical bowel obstruction, affecting older adult patients who often have other significant medical conditions. It is caused by impaction of a gallstone in the ileum after being passed through a biliary-enteric fistula. The diagnosis is often delayed since symptoms may be intermittent and investigations fail to identify the cause of the obstruction. The mainstay of treatment is removal of the obstructing stone after resuscitating the patient. Gallstone ileus continues to be associated with relatively high rates of morbidity and mortality.
How To Cleanse Colon
Colon polyp facts Colon polyps are growths on the inner lining of the colon and are very common. Colon polyps are important because they may be, or may become malignant (cancerous). They also are important because based on their size, number, and microscopic anatomy (histology); they can predict which patients are more likely to develop more polyps and colon cancer. Changes in the genetic material of cells lining the colon are the cause of polyps. There are different types of colon polyps with differing tendencies to become malignant and abilities to predict the development of more polyps and cancer. It is important to recognize families with members who have familial genetic conditions causing polyps because some of these conditions are associated with a very high incidence of colon cancer, and the cancer can be prevented or discovered early.
The timing of the nausea or vomiting can indicate the cause. When appearing shortly after a meal, nausea or vomiting may be caused by food poisoning, gastritis (inflammation of the stomach lining), an ulcer, or bulimia. Nausea or vomiting one to eight hours after a meal may also indicate food poisoning.
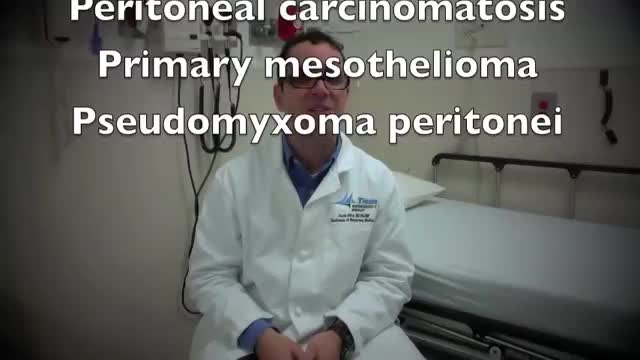
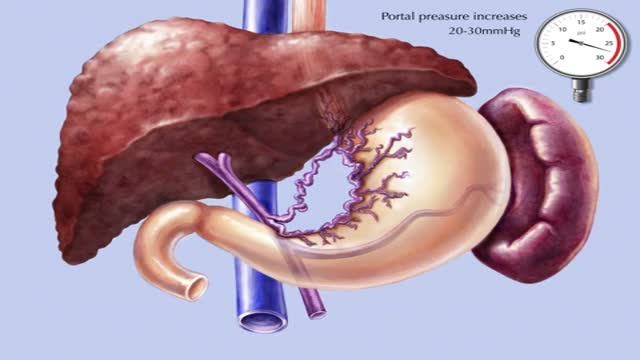
The accumulation of ascitic fluid represents a state of total-body sodium and water excess, but the event that initiates the unbalance is unclear. Although many pathogenic processes have been implicated in the development of abdominal ascites, about 75% likely occur as a result of portal hypertension in the setting of liver cirrhosis, with the remainder due to infective, inflammatory, and infiltrative conditions. Three theories of ascites formation have been proposed: underfilling, overflow, and peripheral arterial vasodilation. The underfilling theory suggests that the primary abnormality is inappropriate sequestration of fluid within the splanchnic vascular bed due to portal hypertension and a consequent decrease in effective circulating blood volume. This activates the plasma renin, aldosterone, and sympathetic nervous system, resulting in renal sodium and water retention. The overflow theory suggests that the primary abnormality is inappropriate renal retention of sodium and water in the absence of volume depletion. This theory was developed in accordance with the observation that patients with cirrhosis have intravascular hypervolemia rather than hypovolemia. The most recent theory, the peripheral arterial vasodilation hypothesis, includes components of both of the other theories. It suggests that portal hypertension leads to vasodilation, which causes decreased effective arterial blood volume. As the natural history of the disease progresses, neurohumoral excitation increases, more renal sodium is retained, and plasma volume expands. This leads to overflow of fluid into the peritoneal cavity. The vasodilation theory proposes that underfilling is operative early and overflow is operative late in the natural history of cirrhosis. Although the sequence of events that occurs between the development of portal hypertension and renal sodium retention is not entirely clear, portal hypertension apparently leads to an increase in nitric oxide levels. Nitric oxide mediates splanchnic and peripheral vasodilation. Hepatic artery nitric oxide synthase activity is greater in patients with ascites than in those without ascites. Regardless of the initiating event, a number of factors contribute to the accumulation of fluid in the abdominal cavity. Elevated levels of epinephrine and norepinephrine are well-documented factors. Hypoalbuminemia and reduced plasma oncotic pressure favor the extravasation of fluid from the plasma to the peritoneal fluid, and, thus, ascites is infrequent in patients with cirrhosis unless both portal hypertension and hypoalbuminemia are present.
Transjugular intrahepatic portosystemic shunt or transjugular intrahepatic portosystemic stent shunting (commonly abbreviated as TIPS or TIPSS) is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein.
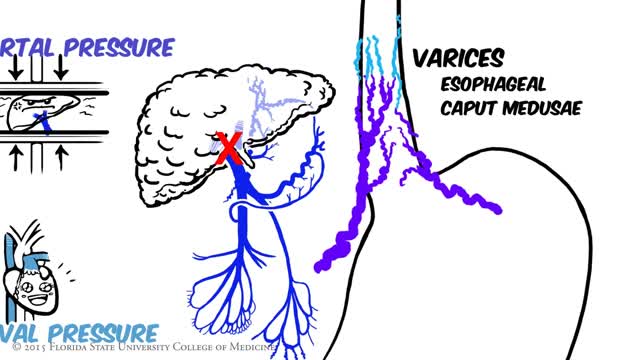
Portal hypertension is an increase in the blood pressure within a system of veins called the portal venous system. Veins coming from the stomach, intestine, spleen, and pancreas merge into the portal vein, which then branches into smaller vessels and travels through the liver.
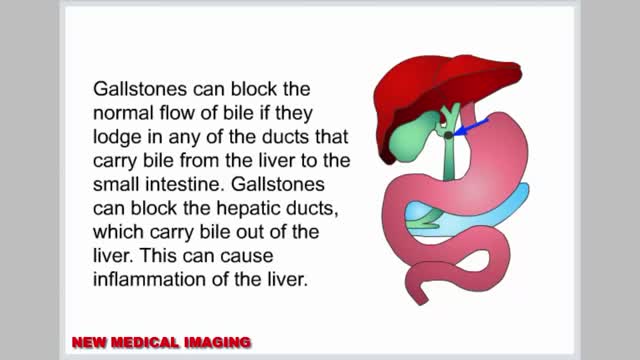
Gallstones are hardened deposits of digestive fluid that can form in your gallbladder. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. The gallbladder holds a digestive fluid called bile that's released into your small intestine. Gallstones range in size from as small as a grain of sand to as large as a golf ball. Some people develop just one gallstone, while others develop many gallstones at the same time. Gallstones are common in the United States. People who experience symptoms from their gallstones usually require gallbladder removal surgery. Gallstones that don't cause any signs and symptoms typically don't need treatment.
Endoscopic retrograde cholangiopancreatography, or ERCP, is a specialized technique used to study the bile ducts, pancreatic duct and gallbladder. Ducts are drainage routes; the drainage channels from the liver are called bile or biliary ducts. The pancreatic duct is the drainage channel from the pancreas.