Gastroenterology
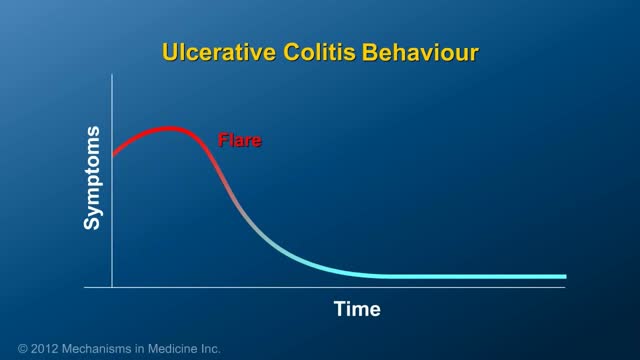
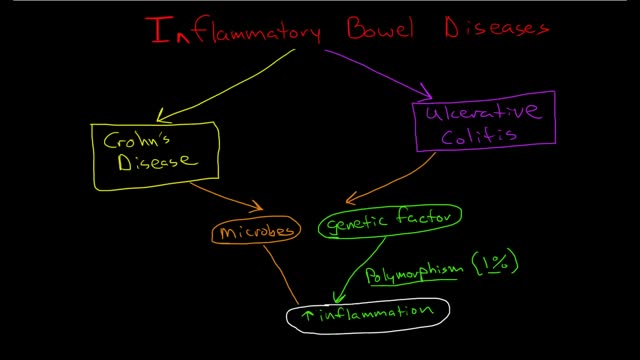
Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine (colon) and rectum. Symptoms usually develop over time, rather than suddenly. Ulcerative colitis can be debilitating and sometimes can lead to life-threatening complications. While it has no known cure, treatment can greatly reduce signs and symptoms of the disease and even bring about long-term remission.
Symptoms of liver failure include vomiting, diarrhea and fatigue as well as the symptoms from stage 3. While the progression from cirrhosis to failure can take years, the damage is irreversible and leads to eventual death. The key to treating liver disease is to diagnose the condition as early as possible.
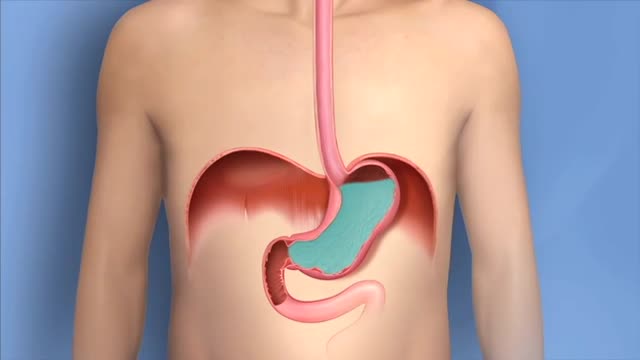
Gastroesophageal reflux disease (GERD) is a chronic digestive disease. GERD occurs when stomach acid or, occasionally, stomach content, flows back into your food pipe (esophagus). The backwash (reflux) irritates the lining of your esophagus and causes GERD. Both acid reflux and heartburn are common digestive conditions that many people experience from time to time. When these signs and symptoms occur at least twice each week or interfere with your daily life, or when your doctor can see damage to your esophagus, you may be diagnosed with GERD. Most people can manage the discomfort of GERD with lifestyle changes and over-the-counter medications. But some people with GERD may need stronger medications, or even surgery, to reduce symptoms.
Your stomach must be empty, so you should not eat or drink anything for approximately 8 hours before the examination. Your physician will be more specific about the time to begin fasting depending on the time of day that your test is scheduled. Your current medications may need to be adjusted or avoided. Most medications can be continued as usual. Medication use such as aspirin, Vitamin E, non-steroidal anti-inflammatories, blood thinners and insulin should be discussed with your physician prior to the examination as well as any other medication you might be taking. It is therefore best to inform your physician of any allergies to medications, iodine, or shellfish. It is essential that you alert your physician if you require antibiotics prior to undergoing dental procedures, since you may also require antibiotics prior to ERCP. Also, if you have any major diseases, such as heart or lung disease that may require special attention during the procedure, discuss this with your physician. To make the examination comfortable, you will be sedated during the procedure, and, therefore, you will need someone to drive you home afterward. Sedatives will affect your judgment and reflexes for the rest of the day, so you should not drive or operate machinery until the next day.
ERCP is most commonly performed to diagnose conditions of the pancreas or bile ducts, and is also used to treat those conditions. It is used to evaluate symptoms suggestive of disease in these organs, or to further clarify abnormal results from blood tests or imaging tests such as ultrasound or CT scan. The most common reasons to do ERCP include abdominal pain, weight loss, jaundice (yellowing of the skin), or an ultrasound or CT scan that shows stones or a mass in these organs. ERCP may be used before or after gallbladder surgery to assist in the performance of that operation. Bile duct stones can be diagnosed and removed with an ERCP. Tumors, both cancerous and noncancerous, can be diagnosed and then treated with indwelling plastic tubes that are used to bypass a blockage of the bile duct. Complications from gallbladder surgery can also sometimes be diagnosed and treated with ERCP. In patients with suspected or known pancreatic disease, ERCP will help determine the need for surgery or the best type of surgical procedure to be performed. Occasionally, pancreatic stones can be removed by ERCP.
ERCP is a procedure that enables your physician to examine the pancreatic and bile ducts. A bendable, lighted tube (endoscope) about the thickness of your index finger is placed through your mouth and into your stomach and first part of the small intestine (duodenum). In the duodenum a small opening is identified (ampulla) and a small plastic tube (cannula) is passed through the endoscope and into this opening. Dye (contrast material) is injected and X-rays are taken to study the ducts of the pancreas and liver.
Many over-the-counter medications can help relieve heartburn. The options include: Antacids, which help neutralize stomach acid. Antacids may provide quick relief. But they can't heal an esophagus damaged by stomach acid. H-2-receptor antagonists (H2RAs), which can reduce stomach acid. H2RAs don't act as quickly as antacids, but may provide longer relief. Proton pump inhibitors, such as lansoprazole (Prevacid 24HR) and omeprazole (Prilosec OTC), which also can reduce stomach acid.
Heartburn is a burning pain in your chest, just behind your breastbone. The pain is often worse when lying down or bending over. Occasional heartburn is common and no cause for alarm. Most people can manage the discomfort of heartburn on their own with lifestyle changes and over-the-counter medications. Heartburn that is more frequent or interferes with your daily routine may be a symptom of a more serious condition that requires medical care
Symptoms Burning stomach pain Feeling of fullness, bloating or belching Fatty food intolerance Heartburn Nausea The most common peptic ulcer symptom is burning stomach pain. Stomach acid makes the pain worse, as does having an empty stomach. The pain can often be relieved by eating certain foods that buffer stomach acid or by taking an acid-reducing medication, but then it may come back. The pain may be worse between meals and at night. Nearly three-quarters of people with peptic ulcers don't have symptoms. Less often, ulcers may cause severe signs or symptoms such as: Vomiting or vomiting blood — which may appear red or black Dark blood in stools, or stools that are black or tarry Trouble breathing Feeling faint Nausea or vomiting Unexplained weight loss Appetite changes
Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is stomach pain. Peptic ulcers include: Gastric ulcers that occur on the inside of the stomach Duodenal ulcers that occur on the inside of the upper portion of your small intestine (duodenum) The most common causes of peptic ulcers are infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of aspirin and certain other painkillers, such as ibuprofen (Advil, Motrin, others) and naproxen sodium (Aleve, Anaprox, others). Stress and spicy foods do not cause peptic ulcers. However, they can make your symptoms worse.
Megacolon, as well as megarectum, is a descriptive term. It denotes dilatation of the colon that is not caused by mechanical obstruction.[1, 2] Although the definition of megacolon has varied in the literature, most researchers use the measurement of greater than 12 cm for the cecum as the standard. Because the diameter of the large intestine varies, the following definitions would also be considered: greater than 6.5 cm in the rectosigmoid region and greater than 8 cm for the ascending colon. Megacolon can be divided into the following 3 categories: Acute megacolon ( pseudo-obstruction) Chronic megacolon, which includes congenital, acquired, and idiopathic causes Toxic megacolon
Constipation is a common problem. It means either going to the toilet less often than usual to empty the bowels, or passing hard or painful stools (faeces). Constipation may be caused by not eating enough fibre, or not drinking enough fluids. It can also be a side-effect of certain medicines, or related to an underlying medical condition. In many cases, the cause is not clear. Laxatives are a group of medicines that can treat constipation. Ideally, laxatives should only be used for short periods of time until symptoms ease. Note: there is a separate leaflet on constipation in children. What is constipation? Constipation is common. If you are constipated it causes one or more of the following: Stools (faeces) become hard and difficult or painful to pass. The time between toilet trips increases compared with your usual pattern. (Note: there is a large range of normal bowel habit. Some people normally go to the toilet to pass stools 2-3 times per day. For others, 2-3 times per week is normal. It is a change from your usual pattern that may mean that you are constipated.) Sometimes, crampy pains occur in the lower part of your tummy (abdomen) You may also feel bloated and feel sick if you have severe constipation. What are the causes of constipation? Known causes include the following: Not eating enough fibre (roughage) is a common cause. The average person in the UK eats about 12 g of fibre each day. But, 18 g per day is recommended by the British Nutrition Foundation. Fibre is the part of plant food that is not digested. It remains in your gut. It adds bulk to the stools (faeces) and helps your bowels to work well. Foods high in fibre include fruit, vegetables, cereals and wholemeal bread. Not drinking much may make constipation worse. Stools are usually soft and easily passed if you eat enough fibre and drink enough fluid. However, some people need more fibre and/or fluid than others in order to avoid constipation. Some special slimming diets are low in fibre and may cause constipation. Some medicines can cause constipation as a side-effect. Examples are painkillers (particularly those with codeine, such as co-codamol, or very strong painkillers, such as morphine), some antacids, some antidepressants (including amitriptyline) and iron tablets; however, there are many others. See the list of possible side-effects on the leaflet that comes with any medicine that you may be taking. Tell a doctor if you suspect a medicine is making you constipated. A change of medication may be possible. Various medical conditions can cause constipation. For example, an underactive thyroid gland, irritable bowel syndrome, some gut disorders and conditions that cause poor mobility, particularly in the elderly. Pregnancy. About 1 in 5 pregnant women will become constipated. It is due to the hormonal changes of pregnancy that slow down the gut movements. In later pregnancy, it can simply be due to the baby taking up a lot of room in the tummy and the bowels being pushed to one side.
Colorectal cancer screening tests Screening is the process of looking for cancer in people who have no symptoms of the disease. Several tests can be used to screen for colorectal cancers. These tests can be divided into: Tests that can find both colorectal polyps and cancer: These tests look at the structure of the colon itself to find any abnormal areas. This is done either with a scope put into the rectum or with special imaging (x-ray) tests. Polyps found during these tests can be removed before they become cancerous, so these tests may prevent colorectal cancer. Because of this, these tests are preferred if they are available and you are willing to have them. Tests that mainly find cancer: These tests check the stool (feces) for signs of cancer. These tests are less invasive and easier to have done, but they are less likely to detect polyps.
Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of your digestive tract. IBD primarily includes ulcerative colitis and Crohn's disease. Both usually involve severe diarrhea, pain, fatigue and weight loss. IBD can be debilitating and sometimes leads to life-threatening complications. Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease that causes long-lasting inflammation and sores (ulcers) in the innermost lining of your large intestine (colon) and rectum. Crohn's disease is an IBD that cause inflammation of the lining of your digestive tract. In Crohn's disease, inflammation often spreads deep into affected tissues. The inflammation can involve different areas of the digestive tract — the large intestine, small intestine or both. Collagenous (kuh-LAJ-uh-nus) colitis and lymphocytic colitis also are considered inflammatory bowel diseases but are usually regarded separately from classic inflammatory bowel disease.
Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach (esophagus). This condition occurs most often in people with serious liver diseases. Esophageal varices develop when normal blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flows into smaller blood vessels that aren't designed to carry large volumes of blood. The vessels can leak blood or even rupture, causing life-threatening bleeding. A number of drugs and medical procedures can help prevent and stop bleeding from esophageal varices.
The hepatitis E virus, responsible for major epidemics of viral hepatitis in subtropical and tropical countries, was cloned only 7 years ago.1 Hepatitis E was found to belong to the family of Caliciviridae, which includes the Norwalk virus—a common cause of gastroenteritis in humans—and consists of a single, plus-strand RNA genome of approximately 7.2 kb without an envelope (Fig. 1). The virus contains at least three open reading frames encoding viral proteins against which antibodies are made on exposure. These antibodies, especially those against the capsid protein derived from the second open reading frame2 and a protein of unknown function derived from the third open reading frame, are detected by currently available serologic assays. Retrospective studies on stored sera of past epidemics of viral hepatitis in Mexico, Africa, Afghanistan, Pakistan, India, Bangladesh, Burma, Nepal, and Borneo have revealed that all were caused by strains of hepatitis E. In addition, hepatitis E was found to be responsible for the hepatitis epidemic in the southern part of Xinjiang, China, in which 120,000 persons became infected between September 1986 and April 1988.3 Hepatitis E predominantly affects young adults (15 to 40 years old). The symptoms of hepatitis E are similar to those of hepatitis A. Frequently, a prodrome consisting of anorexia, nausea, low-grade fever, and right upper abdominal pain is present 3 to 7 days before jaundice develops. Aminotransferase levels peak (usually between 1,000 and 2,000 U/L) near the onset of symptoms; bilirubin levels (10 to 20 mg/dL) peak later. Jaundice usually resolves after 1 to 2 weeks. In about 10% of cases, the disease is fulminant—especially in pregnant women, among whom mortality rates as high as 20% due to hemorrhagic and thrombotic complications have been reported. No evidence has suggested that hepatitis E can cause chronic infection. Transmission is by the fecal-oral route, predominantly through fecally contaminated drinking water supplies. In addition, however, preliminary reports have suggested transmission of the hepatitis E virus through blood transfusions. Volunteer studies confirmed the presence of the virus in serum and feces before and during clinical disease.4 The virus is shed into feces approximately 1 week before symptoms develop. The incubation period varies from 2 to 9 weeks (mean duration, approximately 45 days). Until now, a few reports had described symptomatic hepatitis E acquired in Europe;5, 6 all patients with symptomatic hepatitis E in the United States were travelers returning from Mexico, Africa, or the Far East, in whom hepatitis E developed after their return home.7 In this issue of the Mayo Clinic Proceedings (pages 1133 to 1136), Kwo and associates describe a case of hepatitis E in a man who had not left the United States during the previous 10 years. Specific serologic tests for hepatitis E virus IgG (enzyme immunoassays and a fluorescent antibody blocking assay) and IgM8 (US strain-specific enzyme-linked immunosorbent assay with use of synthetic polypeptides deduced from the viral genome, as shown in Figure 1), developed at Abbott Laboratories (IgG and IgM) as well as at the Centers for Disease Control and Prevention (IgG), were used to prove that the patient indeed had acute hepatitis E. Researchers at Abbott Laboratories have prepared a report that describes most of the viral genome in this patient (Fig. I).8 Their results are interesting because this strain from the United States differs considerably from hepatitis E strains isolated in Mexico, Burma, Pakistan, or China. Furthermore, the sequence of the US strain is highly homologous (98% and 94% homology at the amino acid level to the second and third open reading frames, respectively) to a recently isolated hepatitis E strain from American swine.9 This finding suggests that, in the United States, hepatitis E is a zoonosis with the swine population as one of its hosts. This relationship would confirm earlier studies in Asia, where swine were also found to carry variants of the hepatitis E virus.10 Why are these two recent discoveries important for medicine in the United States? First, other sporadic, locally acquired cases of acute hepatitis may be caused by hepatitis E. Second, these back-to-back discoveries strongly suggest that a common natural host for hepatitis E is present in countries with more moderate climates. Because swine do not seem to experience any symptoms associated with infection and because symptoms in humans can be minor or absent, we now may also have an explanation for the 1 to 2% of positive hepatitis E serologic results in blood donors in the United States,11 Netherlands,12 and Italy,6 countries with large swine staples. Clearly, more research needs to be done to confirm this hypothesis. Third, in countries with more moderate climates, hepatitis E may often result in a subclinical infection. Is this variation in manifestation due to less virulent strains, and do sequence variations determine virulence? Fourth, swine may be used as an animal model for study of the disease as well as vaccine development.
Hepatitis is an inflammation of the liver. The condition can be self-limiting or can progress to fibrosis (scarring), cirrhosis or liver cancer. Hepatitis viruses are the most common cause of hepatitis in the world but other infections, toxic substances (e.g. alcohol, certain drugs), and autoimmune diseases can also cause hepatitis. There are 5 main hepatitis viruses, referred to as types A, B, C, D and E. These 5 types are of greatest concern because of the burden of illness and death they cause and the potential for outbreaks and epidemic spread. In particular, types B and C lead to chronic disease in hundreds of millions of people and, together, are the most common cause of liver cirrhosis and cancer. Hepatitis A and E are typically caused by ingestion of contaminated food or water. Hepatitis B, C and D usually occur as a result of parenteral contact with infected body fluids. Common modes of transmission for these viruses include receipt of contaminated blood or blood products, invasive medical procedures using contaminated equipment and for hepatitis B transmission from mother to baby at birth, from family member to child, and also by sexual contact. Acute infection may occur with limited or no symptoms, or may include symptoms such as jaundice (yellowing of the skin and eyes), dark urine, extreme fatigue, nausea, vomiting and abdominal pain.
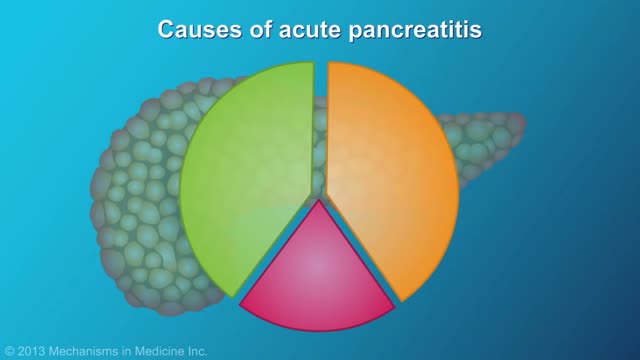
Pancreatitis is inflammation in the pancreas. The pancreas is a long, flat gland that sits tucked behind the stomach in the upper abdomen. The pancreas produces enzymes that assist digestion and hormones that help regulate the way your body processes sugar (glucose). Pancreatitis can occur as acute pancreatitis — meaning it appears suddenly and lasts for days. Or pancreatitis can occur as chronic pancreatitis, which describes pancreatitis that occurs over many years. Mild cases of pancreatitis may go away without treatment, but severe cases can cause life-threatening complications.
Esophageal cancer is cancer that occurs in the esophagus — a long, hollow tube that runs from your throat to your stomach. Your esophagus carries food you swallow to your stomach to be digested. Esophageal cancer usually begins in the cells that line the inside of the esophagus. Esophageal cancer can occur anywhere along the esophagus, but in people in the United States, it occurs most often in the lower portion of the esophagus. More men than women get esophageal cancer. Esophageal cancer isn't common in the United States. In other areas of the world, such as Asia and parts of Africa, esophageal cancer is much more common.
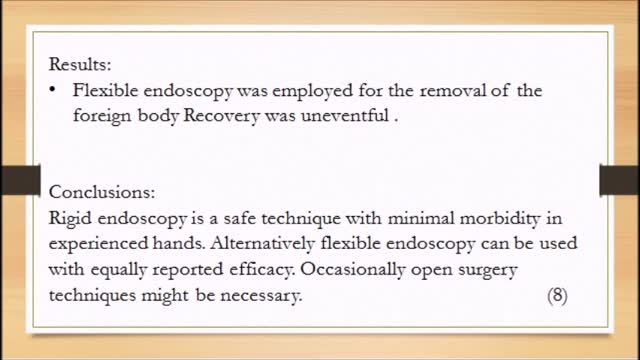
We present a cases of child of age 4 yrs with open safety pin (SP) impacted in the U/3 esophagus and description of the techniques used for their removal