Pulmonology
Difference between healthy lungs and smoker lungs
Effect of smoking,it's very dangerousAfter watch this video I hope smoker stop smoke now it is dangerously for human
A detailed description of the causes and diagnosis of pleural effusion. The presentation includes a discussion of the causes and exudative and transudative pleural effusions. Light's criteria and its modification are described along with definition and clinical implication of pleural fluid acidosis, glucose, adenosine deaminase, hemorrhagic pleural effusion and protein and LDH as well.
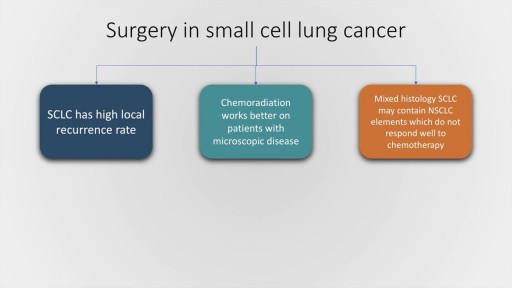
Small cell lung cancer, which occurs almost exclusively in smokers, is a malignancy characterised by rapid doubling time, high growth fraction and widespread metastasis at presentation. In this presentation, we will briefly discuss the classification of pulmonary Neuro-endocrine tumours by the World Health Organisation followed by a detailed discussion of the clinical features, lab evaluation and management of SCLC, both limited and extended stage. The frontline therapy in small cell lung cancer is etoposide and cisplatin along with thoracic radiotherapy and prophylactic cranial irradiation in patients who have a good response to therapy. Hyperfractionation of radiotherapy may provide some benefit but is also associated with increase incidence of complications. Newer agents for SCLC include Vandetanib and immunotherapy molecules, such as Iplimumab and nivolumab.
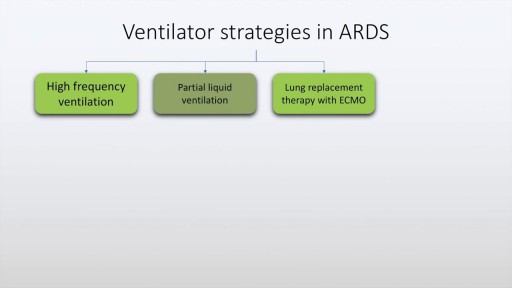
Acute respiratory distress syndrome is characterised by rapid onset dyspnea, bilateral infiltrates on chest x-ray and respiratory failure. This may be due to conditions which directly affect the lung such as pneumonia, aspiration and near drowning. It may also be due to indirect lung injury, as in conditions like sepsis, pancreatitis, trauma and poisoning. The diagnostic criteria of ARDS, often described as the Berlin criteria is discussed in this presentation along with various management aspects of ARDS including ventilation strategies and use of antibiotics and diuretics. Finally prognostic features and alternative strategies are also discussed.
How a Clot Can Become a Pulmonary Embolism
Prompt treatment to break up the clot greatly reduces the risk of death. This can be done with blood thinners and drugs or procedures. Compression stockings and physical activity can help prevent clots from forming in the first place.
Most times, a pulmonary embolism is caused by blood clots that travel from the legs or, rarely, other parts of the body (deep vein thrombosis, or DVT). Symptoms include shortness of breath, chest pain, and cough. Prompt treatment to break up the clot greatly reduces the risk of death. This can be done with blood thinners and drugs or procedures. Compression stockings and physical activity can help prevent clots from forming in the first place.
Pulmonary edema is usually caused by a heart condition. Other causes include pneumonia, exposure to certain toxins and drugs, and being at high elevations. Depending on the cause, pulmonary edema symptoms may appear suddenly or develop over time. Mild to extreme breathing difficulty can occur. Cough, chest pain, and fatigue are other symptoms. Treatment generally includes supplemental oxygen and medications.
The removal of a clot is called an embolectomy. An embolectomy might be done during a surgery. Or it might be done with a minimally invasive procedure that uses a catheter (a thin tube that is guided through a blood vessel). This type of treatment for pulmonary embolism is used only in rare cases.
IVC filter is placed to prevent fatal Pulmonary Embolism due to Deep Venous Thrombosis (DVT). This particular patient had extensive DVT of Ilio-Femoral veins leading to massive swelling of left lower limb. The IVC filter was inserted via the Right Femoral Vein. This case was the first IVC filter placement of North Bengal and adjoining areas.
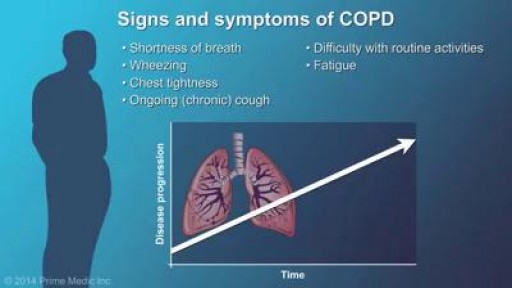
COPD stands for chronic obstructive pulmonary (lung) disease. COPD is a term applied to a family of diseases that includes emphysema, chronic bronchitis, and emphysema due to alpha-1 antitrypsin deficiency. COPD usually progresses gradually, causing limited airflow in and out of the lungs. COPD adds to the work of the heart. Diseased lungs might reduce the amount of oxygen that goes to the blood. High blood pressure in blood vessels from the heart to the lungs makes it difficult for the heart to pump. Lung disease can also cause the body to produce too many red blood cells, which might make the blood thicker and harder to pump.
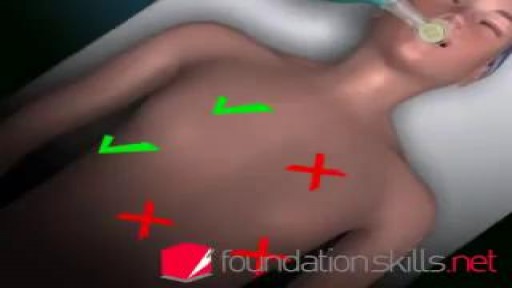
Complications. Mechanical ventilation is often a life-saving intervention, but carries potential complications including pneumothorax, airway injury, alveolar damage, and ventilator-associated pneumonia. Other complications include diaphragm atrophy, decreased cardiac output, and oxygen toxicity.
Endotracheal intubation is a medical procedure in which a tube is placed into the windpipe (trachea) through the mouth or nose. In most emergency situations it is placed through the mouth. Whether you are awake (conscious) or not awake (unconscious), you will be given medicine to make it easier to insert the tube. After endotracheal intubation, you will likely be placed on a breathing machine. If you are awake after the procedure, your health care provider may give you medicine to reduce your anxiety or discomfort.
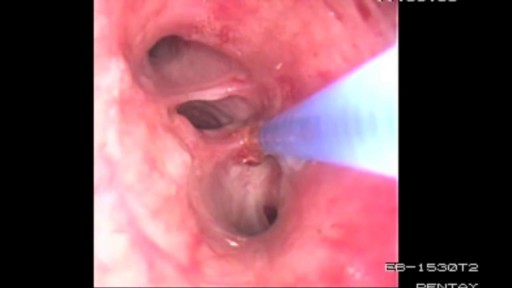
Bronchoscopy Procedure - See inside the lungs!
Smoking causes: Chronic obstructive pulmonary disease (COPD), a disease that gets worse over time and causes wheezing, shortness of breath, chest tightness, and other symptoms. Emphysema, a condition in which the walls between the air sacs in your lungs lose their ability to stretch and shrink back.
A pneumothorax occurs when some of the tiny air sacs (alveoli) in a baby's lung become overinflated and burst. This causes air to leak into the space between the lung and chest wall (pleural space). The most common cause of pneumothorax is respiratory distress syndrome. This is a condition that occurs in babies who are born too early (premature). The baby's lungs lack the slippery substance (surfactant) that helps them stay open. Therefore, the tiny air sacs are not able to expand as easily. If the baby is put on a breathing machine (mechanical ventilator), there is extra pressure on the baby's lungs, which can sometimes burst the air sacs.
Your lungs are have 600 million air pockets -- enough to cover a tennis court.