Pulmonology
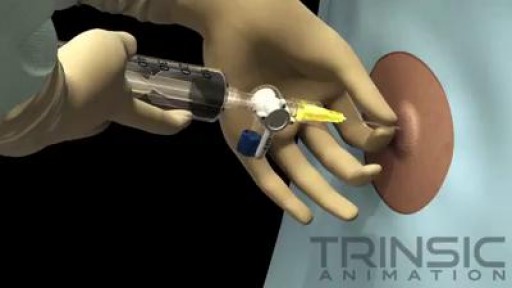
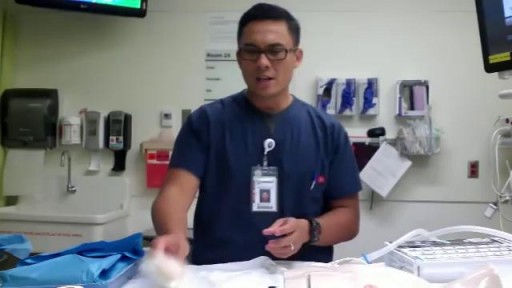
Thoracentesis is a procedure in which a needle is inserted into the pleural space between the lungs and the chest wall. This procedure is done to remove excess fluid, known as a pleural effusion, from the pleural space to help you breathe easier. It may be done to determine the cause of your pleural effusion. Some conditions such as heart failure, lung infections, and tumors can cause pleural effusions.
Chronic obstructive pulmonary disease (COPD) is defined as progressive, chronic airflow obstruction due to chronic bronchitis, emphysema, or both. The majority of patients have components of both, although one of these entities will frequently dominate the clinical picture. Emphysema�airspace enlargement distal to the terminal bronchioles due to destruction of alveolar septa. Chronic bronchitis�chronic airway inflammation and bronchospasm. Clinically defined as productive cough lasting for at least 3 mo over 2 consecutive years. Although COPD is irreversible, patients with acute exacerbations do have reversible bronchospastic and inflammatory components.
For strong lungs, chew 3 to 5 peppermint leaves each day. To treat congestion, add a few drops of peppermint oil to a pot of hot water and inhale the steam. You can also drink 2 cups of peppermint tea daily. To make the tea, add 1 teaspoon of dried peppermint leaves to a cup of hot water.
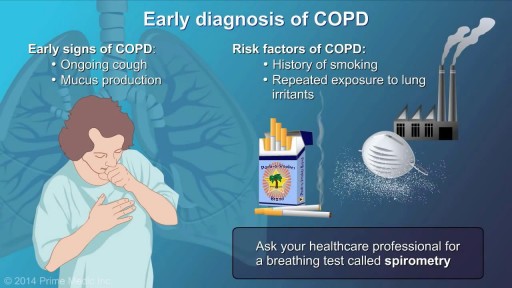
To diagnose COPD, your doctor will probably do the following tests: Medical history and physical exam. These will give your doctor important information about your health. Lung function testsLung function tests, including an FEV1 test. These tests measure the amount of air in your lungs and the speed at which air moves in and out. Spirometry is the most important of these tests. Chest X-rayChest X-ray. This helps rule out other conditions with similar symptoms, such as lung cancer.
The goal of COPD management is to improve a patient’s functional status and quality of life by preserving optimal lung function, improving symptoms, and preventing the recurrence of exacerbations. Currently, no treatments aside from lung transplantation have been shown to significantly improve lung function or decrease mortality; however, oxygen therapy (when appropriate) and smoking cessation may reduce mortality. Once the diagnosis of COPD is established, it is important to educate the patient about the disease and to encourage his or her active participation in therapy.
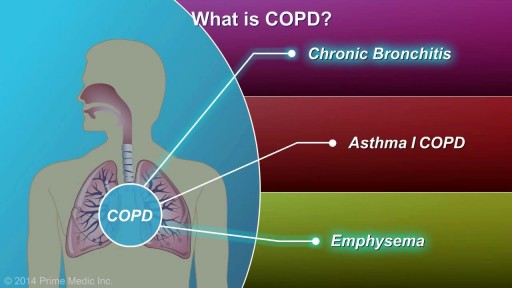
COPD, or chronic obstructive pulmonary disease, is a progressive disease that makes it hard to breathe. Progressive means the disease gets worse over time. COPD can cause coughing that produces large amounts of a slimy substance called mucus, wheezing, shortness of breath, chest tightness, and other symptoms. Cigarette smoking is the leading cause of COPD. Most people who have COPD smoke or used to smoke. However, up to 25 percent of people with COPD never smoked. Long-term exposure to other lung irritants—such as air pollution, chemical fumes, or dusts—also may contribute to COPD. A rare genetic condition called alpha-1 antitrypsin (AAT) deficiency can also cause the disease.
The most common symptoms of pneumoconiosis are cough and shortness of breath. The risk is generally higher when people have been exposed to mineral dusts in high concentrations and/or for long periods of time. Inadequate or inconsistent use of personal protective equipment (PPE) such as respirators (specially fitted protective masks) is another risk factor since preventing dusts from being inhaled will also prevent pneumoconiosis. Pneumoconiosis does not generally occur from environmental (non-workplace) exposures since dust levels in the environment are much lower.
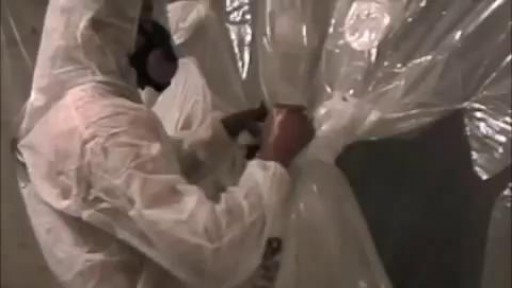
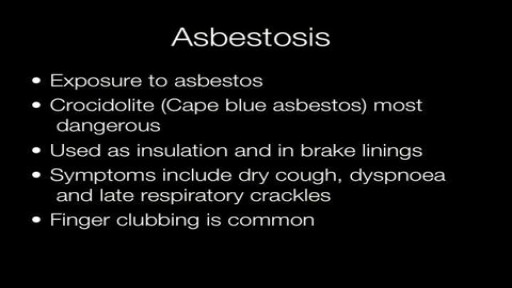
Every owner of a building where asbestos abatement activity occurs is responsible for the performance of the asbestos abatement activities by his/her agent, contractor, employee, or other representative. Each building owner is responsible for determining the amount of asbestos-containing material that may be disturbed during the course of work. The size and scope of the overall project, with particular reference to the total amount of asbestos-containing material that will be disturbed determines the reporting or filing requirements established in the Asbestos Control Program Rules. An asbestos project is defined as any form of work that will disturb more than 25 linear feet or more than 10 square feet of asbestos-containing material.
www.lung.org > Lung Health and Diseases > Lung Disease Lookup > Silicosis Learn About Silicosis Silicosis is a lung disease caused by breathing in tiny bits of silica, a mineral that is part of sand, rock, and mineral ores such as quartz. It mostly affects workers exposed to silica dust in occupations such mining, glass manufacturing, and foundry work. Over time, exposure to silica particles causes scarring in the lungs, which can harm your ability to breathe. Key Facts There are three types of silicosis: acute, chronic, and accelerated. It occurs in workers from mines, foundries, sandblasting, and glass manufacturing. About 2 million US workers remain potentially exposed to occupational silica. There is no cure for silicosis, but it can be prevented. What Is Silicosis? There are three types of silicosis: Acute silicosis, which causes cough, weight loss, and fatigue within a few weeks or years of exposure to inhaled silica. Chronic silicosis, which appears 10 to 30 years after exposure and can affect upper lungs and sometimes cause extensive scarring. Accelerated silicosis, which occurs within 10 years of high-level exposure. Silicosis can develop within a few weeks to even decades after exposure. When people breathe silica dust, they inhale tiny particles of the mineral silica. This silica dust can cause fluid buildup and scar tissue in the lungs that cuts down your ability to breathe. This can lead to lung scarring and cough, weight loss, and fatigue.
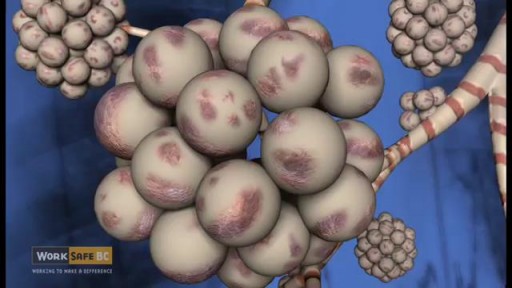
Asbestosis is linked to chrysotile fibers. Chrysotile is one of the six known types of asbestos. Exposure occurs when someone breathes in the dangerous fibers. Extended exposure can lead to an accumulation of the fibers in lung tissues, setting the stage for long-term fibrosis (scarring). Over time, lung tissues thicken, causing pain and restricting breathing. Symptoms include labored breathing during routine tasks and exercise, chest pain and coughing. Doctors prescribe breathing treatments, prescription medication and sometimes surgery for people with asbestosis.

If you’re like me, you probably hook your chest tube up to a Pleur-Evac, put it on the ground, then back away slowly. Who knows what goes on in that mysterious bubbling white box? Hopefully this will post shed some light. Isn’t this just a container for stuff that comes out of the chest? Why does it look so complicated? It’s complicated because the detection/collection of air and fluid require different setups. Most commercial models also allow you to hook the drainage system to wall suction, so you can quickly evacuate the pleural space. This requires its own setup. Because of the need to juggle air, fluid and suction, the most common commercial system includes 3 distinct chambers. If you were to simplify the device, or build one out of spare bottles and tubes, it might look like this:
A small spontaneous pneumothorax may resolve without treatment; a pneumothorax arising as a result of lung disease or injury requires immediate treatment. Treatment may include insertion of a chest tube or aspiration of the free air in the chest cavity.

A small spontaneous pneumothorax may resolve without treatment; a pneumothorax arising as a result of lung disease or injury requires immediate treatment. Treatment may include insertion of a chest tube or aspiration of the free air in the chest cavity.Feb 19, 2016
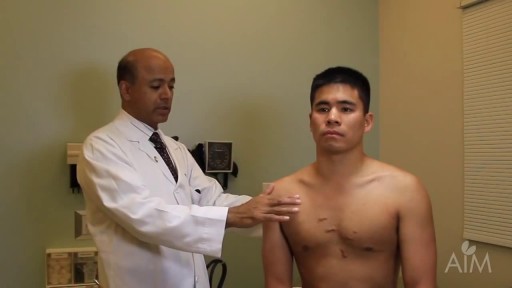
Primary spontaneous pneumothorax is an abnormal accumulation of air in the space between the lungs and the chest cavity (called the pleural space) that can result in the partial or complete collapse of a lung. This type of pneumothorax is described as primary because it occurs in the absence of lung disease such as emphysema. Spontaneous means the pneumothorax was not caused by an injury such as a rib fracture. Primary spontaneous pneumothorax is likely due to the formation of small sacs of air (blebs) in lung tissue that rupture, causing air to leak into the pleural space. Air in the pleural space creates pressure on the lung and can lead to its collapse. A person with this condition may feel chest pain on the side of the collapsed lung and shortness of breath.
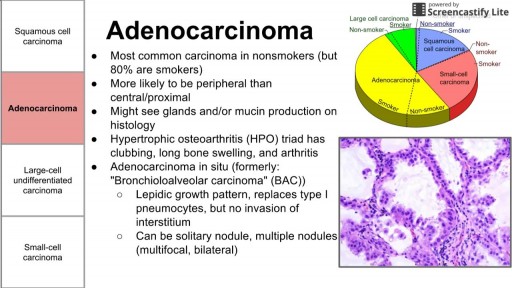
There are three main types of lung cancer. Knowing which type you have is important because it affects your treatment options and your outlook (prognosis). If you aren’t sure which type of lung cancer you have, ask your doctor so you can get the right information.
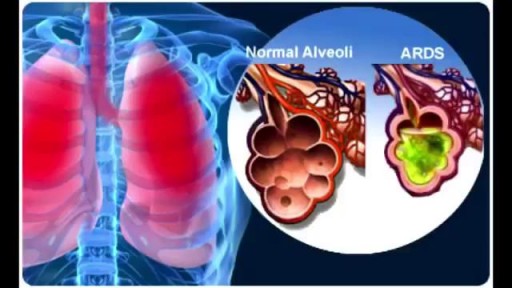
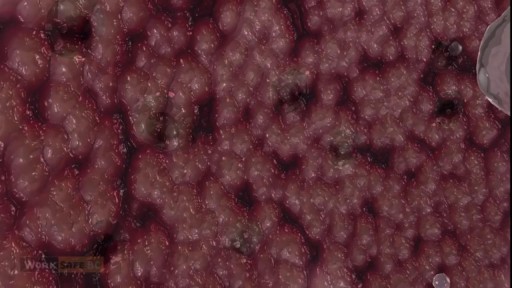
ARDS was recognized as the most severe form of acute lung injury (ALI), a form of diffuse alveolar injury. The AECC defined ARDS as an acute condition characterized by bilateral pulmonary infiltrates and severe hypoxemia in the absence of evidence for cardiogenic pulmonary edema. The severity of hypoxemia necessary to make the diagnosis of ARDS was defined by the ratio of the partial pressure of oxygen in the patient’s arterial blood (PaO2) to the fraction of oxygen in the inspired air (FiO2). ARDS was defined by a PaO2/FiO2 ratio of less than 200, and in ALI, less than 300. This definition was further refined in 2011 by a panel of experts and is termed the Berlin definition of ARDS. [3] ARDS is defined by timing (within 1 wk of clinical insult or onset of respiratory symptoms); radiographic changes (bilateral opacities not fully explained by effusions, consolidation, or atelectasis); origin of edema (not fully explained by cardiac failure or fluid overload); and severity based on the PaO2/FiO2 ratio on 5 cm of continuous positive airway pressure (CPAP). The 3 categories are mild (PaO2/FiO2 200-300), moderate (PaO2/FiO2 100-200), and severe (PaO2/FiO2 ≤100).
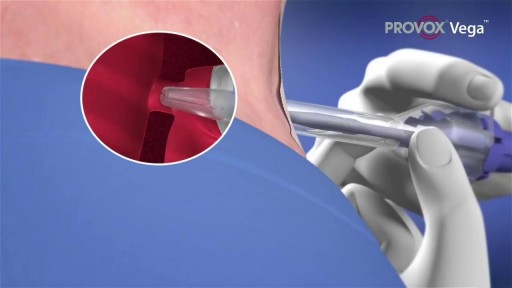
A voice prosthesis (plural prostheses) is an artificial device, usually made of silicone that is used to help laryngectomized patients to speak. During a total laryngectomy, the entire voice box (larynx) is removed and the windpipe (trachea) and food pipe (esophagus) are separated from each other.

James Burke Fine DMD by James Burke Fine DMD Periodontal disease is a gum condition caused by the buildup of bacteria along and below the teeth's gumline. Acute forms are usually associated with pain from oral tissue gone bad – also known as necrotizing gingivitis or trench mouth – whereas chronic forms are painless but have a more long-term impact on your overall, systemic health. The most common chronic form is gingivitis, whose bleeding, puffiness and redness comes from an organized mass of bacteria called plaque. You may know it can advance into a form called periodontitis. If these conditions are left untreated, however, it can also lead to infections within other parts of the body, such as the lungs.