Pulmonology
Pulmonary fibrosis is a condition in which the tissue deep in your lungs becomes scarred over time. This tissue gets thick and stiff. That makes it hard for you to catch your breath, and your blood may not get enough oxygen. Causes of pulmonary fibrosis include environmental pollutants, some medicines, some connective tissue diseases, and interstitial lung disease. Interstitial lung disease is the name for a large group of diseases that inflame or scar the lungs. In most cases, the cause cannot be found. This is called idiopathic pulmonary fibrosis
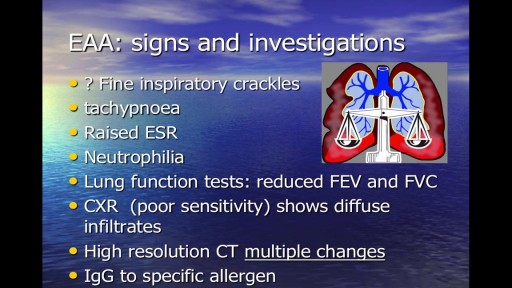
Occupational respiratory disease is any lung condition you get at work. Certain workplaces lend themselves to disease. The most common are coalmines and factories or areas with high amounts of toxins. These include asbestos and silica dust, as well as smoke, fumes, gases, and other particles. Types of occupational respiratory disease include: coal workers’ pneumoconiosis, also known as Black Lung Disease asbestosis silicosis farmers’ lung, also known as allergic alveolitis. It also includes forms of asthma, bronchitis, or emphysema.
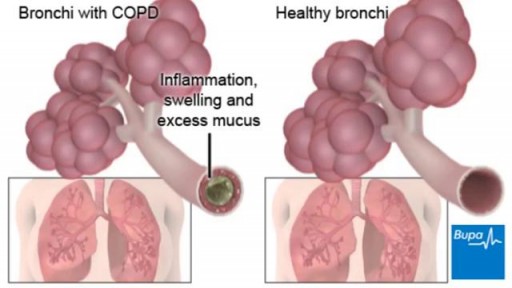
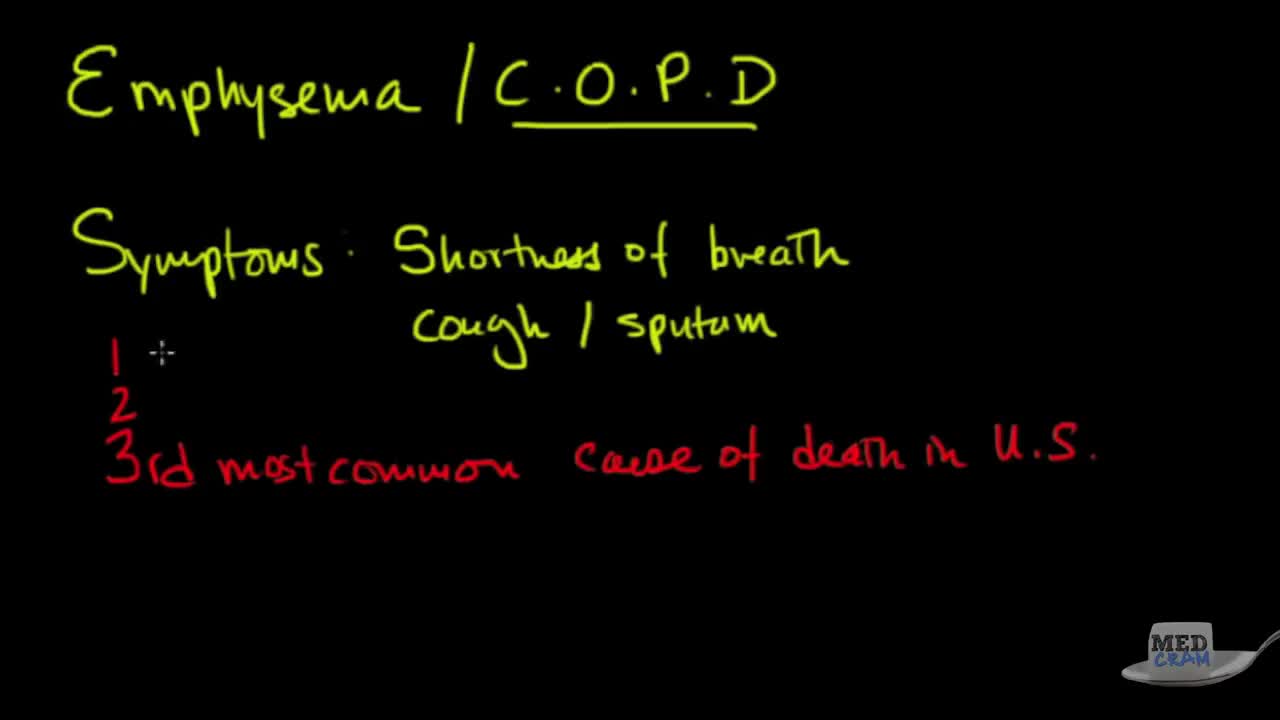
COPD (chronic obstructive pulmonary disease) makes it hard for you to breathe. The two main types are chronic bronchitis and emphysema. The main cause of COPD is long-term exposure to substances that irritate and damage the lungs. This is usually cigarette smoke. Air pollution, chemical fumes, or dust can also cause it. At first, COPD may cause no symptoms or only mild symptoms. As the disease gets worse, symptoms usually become more severe. They include A cough that produces a lot of mucus Shortness of breath, especially with physical activity Wheezing Chest tightness Doctors use lung function tests, imaging tests, and blood tests to diagnose COPD. There is no cure. Treatments may relieve symptoms. They include medicines, oxygen therapy, surgery, or a lung transplant. Quitting smoking is the most important step you can take to treat COPD.
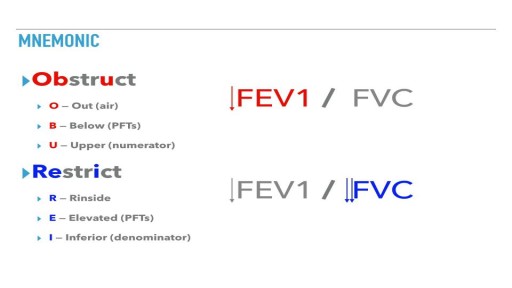
Obstructive lung diseases include conditions that make it hard to exhale all the air in the lungs. People with restrictive lung disease have difficulty fully expanding their lungs with air. Obstructive and restrictive lung disease share the same main symptom: shortness of breath with exertion.
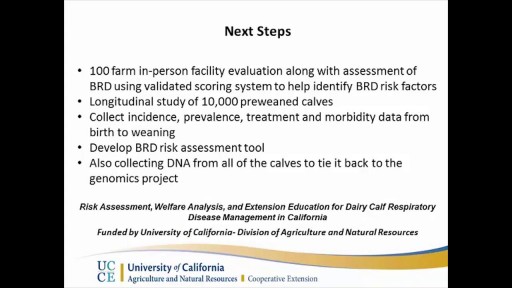
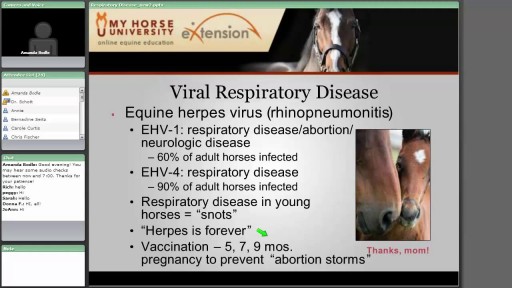
Bovine respiratory disease (BRD) has a multifactorial etiology and develops as a result of complex interactions between environmental factors, host factors, and pathogens. Environmental factors (eg, weaning, transport, commingling, crowding, inclement weather, dust, and inadequate ventilation) serve as stressors that adversely affect the immune and nonimmune defense mechanisms of the host. In addition, certain environmental factors (eg, crowding and inadequate ventilation) can enhance the transmission of infectious agents among animals. Many infectious agents have been associated with BRD. An initial pathogen (eg, a virus) may alter the animal’s defense mechanisms, allowing colonization of the lower respiratory tract by bacteria.
The Irish Thoracic Society speak about the importance of Exercise with Chronic or Acute Respiratory illnesses/ Diseases and respiratory distress
These air sacs make up most of the lung tissue. Lung diseases affecting the alveoli include: Pneumonia: An infection of the alveoli, usually by bacteria. Tuberculosis: A slowly progressive pneumonia caused by the bacteria Mycobacterium tuberculosis. Chronic respiratory diseases are chronic diseases of the airways and other structures of the lung. Some of the most common are: asthma, chronic obstructive pulmonary disease, occupational lung diseases and pulmonary hypertension.
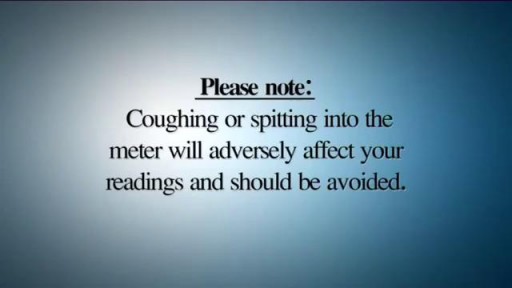
A peak flow meter is an inexpensive, portable, handheld device for those with asthma that is used to measure how well air moves out of your lungs. Measuring your peak flow using this meter is an important part of managing your asthma symptoms and preventing an asthma attack.
The Irish Thoracic Society explain the Active Cycle of Breathing Technique for patients with acute and chronic respiratory illnesses and diseases and respiratory distress
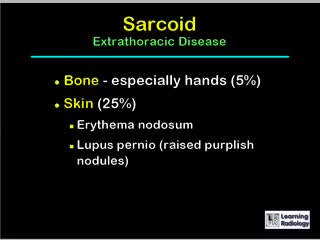
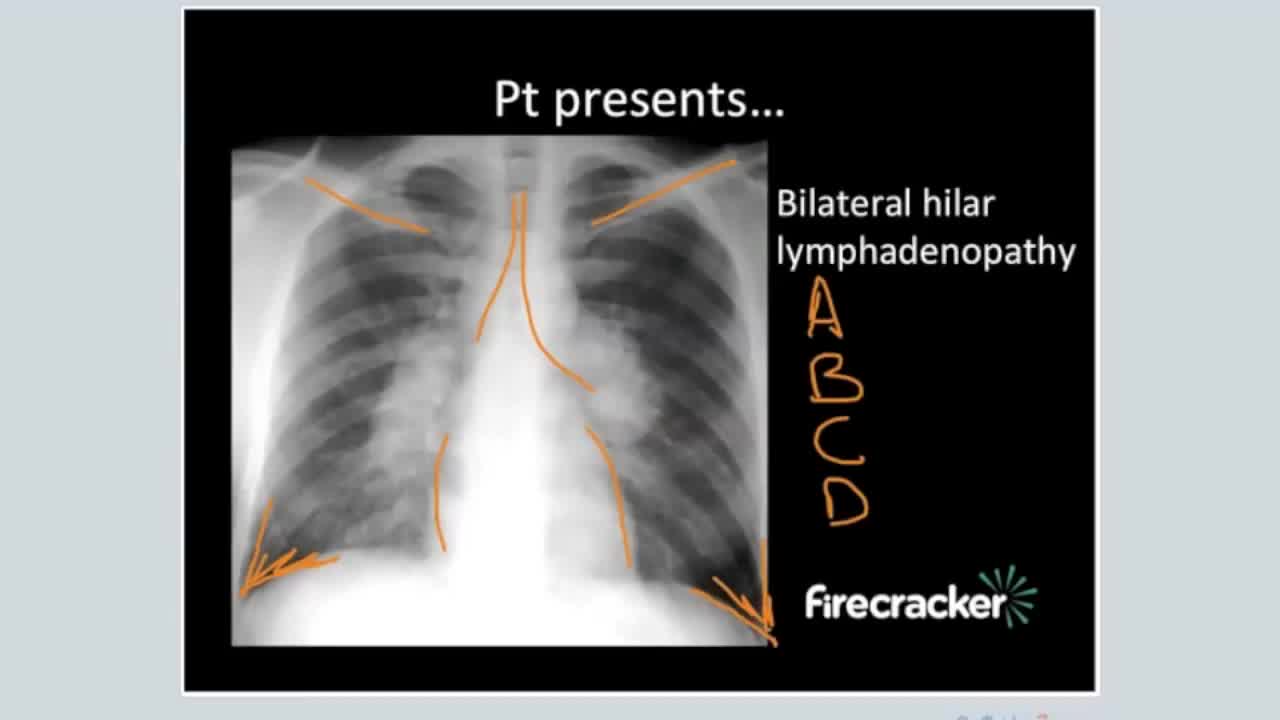
A diagnosis of sarcoidosis is established on the basis of compatible clinical and radiologic findings and histologic evidence of the presence of noncaseous epithelioid cell granulomas in one or more organs and the absence of causative organisms or particulates (16). Granulomas of known causes and local sarcoidlike reactions must be excluded. Granulomatous lesions may result from many conditions, including tuberculosis, berylliosis, leprosy, hypersensitivity pneumonitis, Crohn disease, primary biliary cirrhosis, and fungal disease. Moreover, local sarcoidlike reactions may be seen in lymph nodes that drain a neoplasm or a site of chronic inflammation (19). Such reactions also have been seen in patients who have undergone chemotherapy and radiation therapy (23). If biopsy of lymph nodes or pulmonary or pleural tissue is necessary for diagnosis, one of three techniques may be used: transbronchial biopsy, CT-guided biopsy, or surgical biopsy (24). The use of a surgical technique may be warranted when the results of biopsy with another procedure are not definitive and biopsy of mediastinal lymph nodes, lung, or both is required. This can generally be done with minimally invasive procedures, such as cervical mediastinoscopy, the Chamberlain procedure (a parasternal minithoracotomy for biopsy of the aortopulmonary window or para-aortic nodes), or video-assisted thoracoscopic surgical biopsy (25).
Sarcoidosis is an inflammatory disease that affects multiple organs in the body, but mostly the lungs and lymph glands. In people with sarcoidosis, abnormal masses or nodules (called granulomas) consisting of inflamed tissues form in certain organs of the body. These granulomas may alter the normal structure and possibly the function of the affected organ(s).
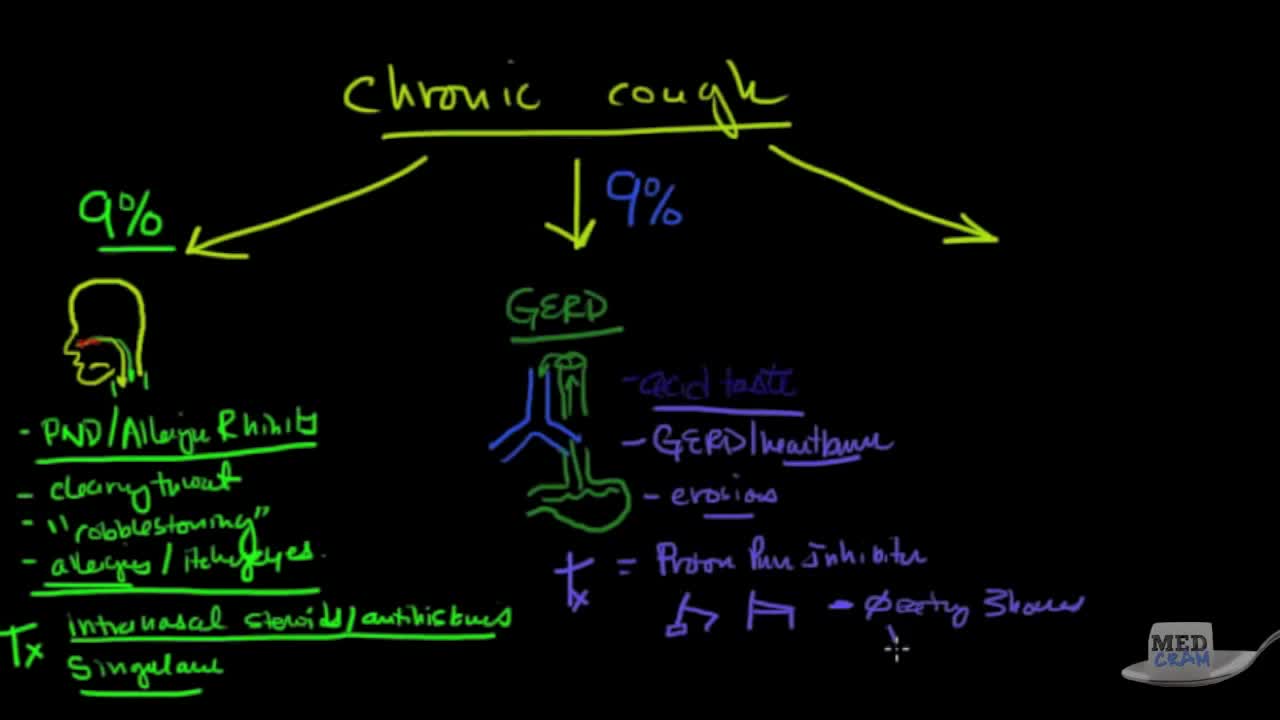
A chronic cough is a cough that lasts eight weeks or longer in adults, or four weeks in children. A chronic cough is more than just an annoyance. A chronic cough can interrupt your sleep and leave you feeling exhausted. Severe cases of chronic cough can cause vomiting, lightheadedness and even rib fractures. While it can sometimes be difficult to pinpoint the problem that's triggering a chronic cough, the most common causes are tobacco use, postnasal drip, asthma and acid reflux. Fortunately, chronic cough typically disappears once the underlying problem is treated.
Emphysema, also known as COPD, is a chronic condition with multiple factors that impact survival and life expectancy. Stages of COPD are generally defined using the GOLD criteria (Global Initiative for Chronic Obstructive Lung Disease). It has four levels or stages: mild - or Stage 1.
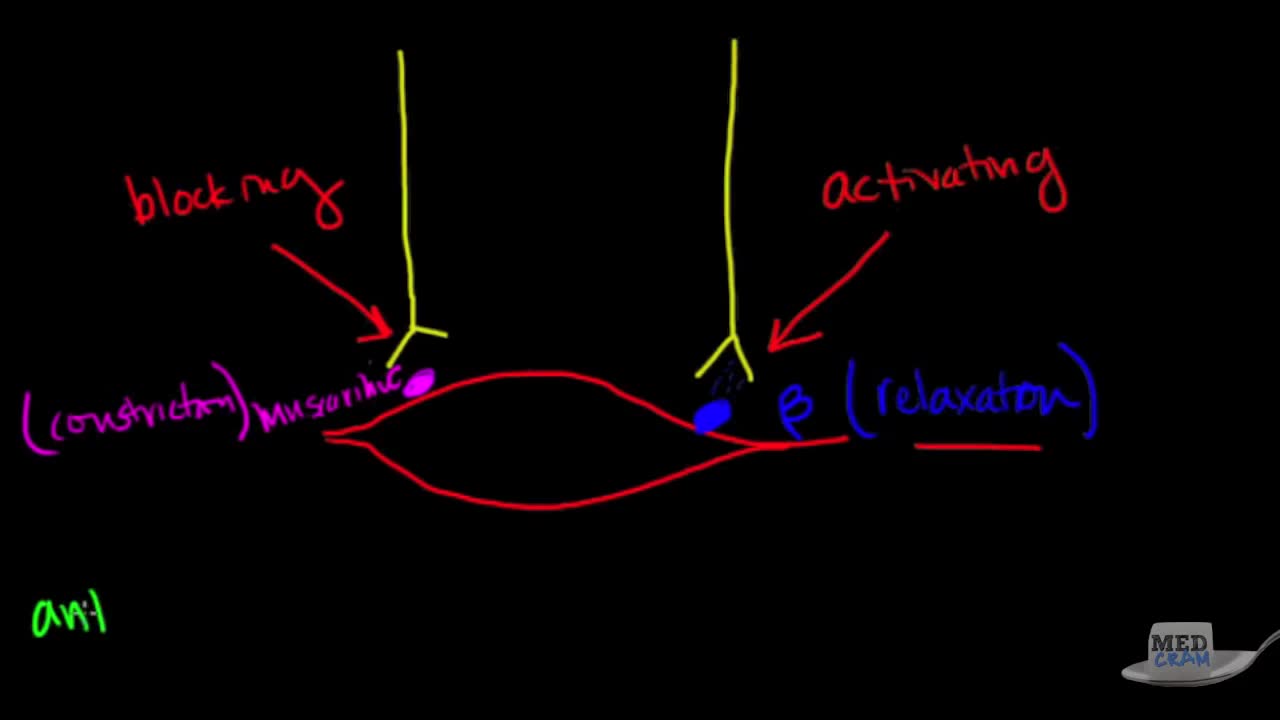
Includes discussion on asthma pathophysiology, signs and symptoms of asthma, diagnosis, triggers (GERD, post nasal drip, down feathers, etc.), flow volume loops, samter's triad, and more. This is video 1 of 2 on asthma and treatment.
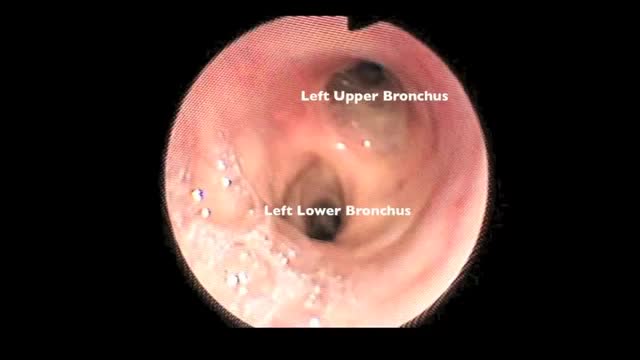
Flexible bronchoscopy is a procedure that allows a clinician to examine the breathing passages (airways) of the lungs (figure 1). Flexible bronchoscopy can be either a diagnostic procedure (to find out more about a possible problem) or a therapeutic procedure (to try to treat an existing problem or condition).
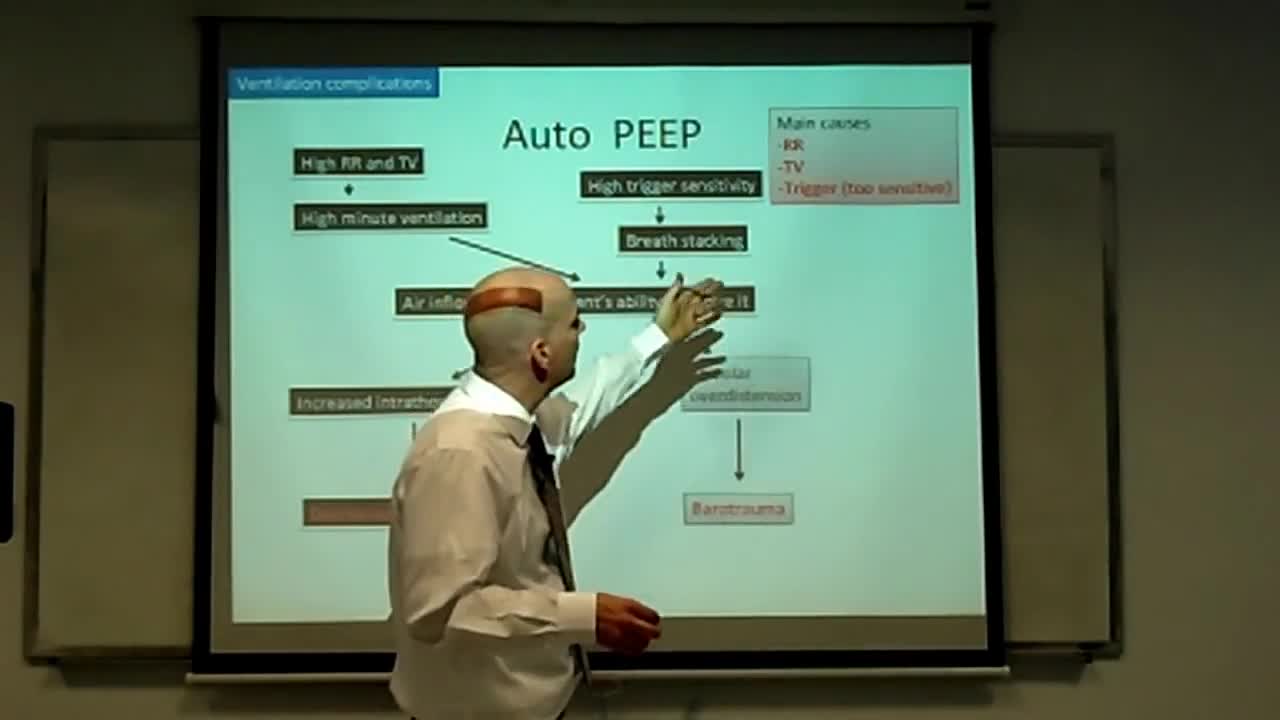
This is an introduction to ventilator settings like FIO2, PEEP, Flow rate,trigger,TV, and RR. I also discuss how these settings relate to CO2 and O2 control and to complications like oxygen toxicity and barotrauma with an emphasis on physiology.
This 3D medical animation provides a general overview of asthma, the clinical condition of the upper respiratory airways.
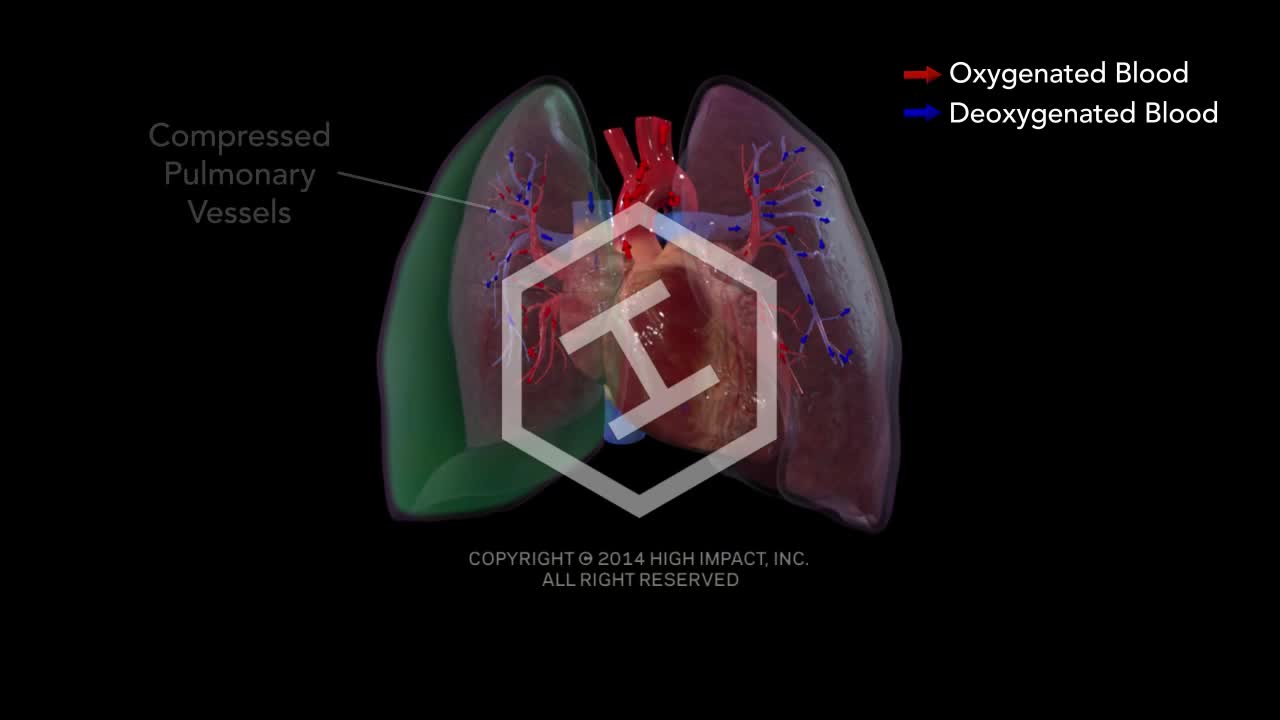
Tension pneumothorax develops when a lung or chest wall injury is such that it allows air into the pleural space but not out of it (a one-way valve). As a result, air accumulates and compresses the lung, eventually shifting the mediastinum, compressing the contralateral lung, and increasing intrathoracic pressure enough to decrease venous return to the heart, causing shock. These effects can develop rapidly, particularly in patients undergoing positive pressure ventilation.
Hemothorax is the presence of blood in the pleural space. The source of blood may be the chest wall, lung parenchyma, heart, or great vessels. Although some authors state that a hematocrit value of at least 50% is necessary to differentiate a hemothorax from a bloody pleural effusion, most do not agree on any specific distinction. Hemothorax is usually a consequence of blunt or penetrating trauma. Much less commonly, it may be a complication of disease, may be iatrogenically induced, [1] or may develop spontaneously. [2] Prompt identification and treatment of traumatic hemothorax is an essential part of the care of the injured patient. The upright chest radiograph is the ideal primary diagnostic study in the evaluation of hemothorax (see Workup). In cases of hemothorax unrelated to trauma, a careful investigation for the underlying source must be performed while treatment is provided.
Acute hemothorax due to aortic rupture in aortic dissection with lung collapse and mediastinal shift.