Reproductive Health

Childbirth (also called labour, birth, partus or parturition) is the culmination of a human pregnancy or gestation period with the birth of one or more newborn infants from a woman's uterus. The process of normal human childbirth is categorized in three stages of labour: the shortening and dilation of the cervix, descent and birth of the infant, and birth of the placenta. In many cases, with increasing frequency, childbirth is achieved through caesarean section, the removal of the neonate through a surgical incision in the abdomen, rather than through vaginal birth. In the U.S. and Canada it represents nearly 1 in 3 (31.8%) and 1 in 4 (22.5%) of all childbirths, respectively.

A breech birth is the birth of a baby from a breech presentation. In the breech presentation the baby enters the birth canal with the buttocks or feet first as opposed to the normal head first presentation.
There are either three or four main categories of breech births, depending upon the source:
* Frank breech - the baby's bottom comes first, and his or her legs are flexed at the hip and extended at the knees (with feet near the ears). 65-70% of breech babies are in the frank breech position.
* Complete breech - the baby's hips and knees are flexed so that the baby is sitting crosslegged, with feet beside the bottom.
* Footling breech - one or both feet come first, with the bottom at a higher position. This is rare at term but relatively common with premature fetuses.
* Kneeling breech - the baby is in a kneeling position, with one or both legs extended at the hips and flexed at the knees. This is extremely rare, and is excluded from many classifications.
As in labour with a baby in a normal head-down position, uterine contractions typically occur at regular intervals and gradually cause the cervix to become thinner and to open. In the more common breech presentations, the baby’s bottom (rather than feet or knees) is what is first to descend through the maternal pelvis and emerge from the vagina.
At the beginning of labour, the baby is generally in an oblique position, facing either the right or left side of the mother's back. As the baby's bottom is the same size in the term baby as the baby's head. Descent is thus as for the presenting fetal head and delay in descent is a cardinal sign of possible problems with the delivery of the head.
In order to begin the birth, internal rotation needs to occur. This happens when the mother's pelvic floor muscles cause the baby to turn so that it can be born with one hip directly in front of the other. At this point the baby is facing one of the mother's inner thighs. Then, the shoulders follow the same path as the hips did. At this time the baby usually turns to face the mother's back. Next occurs external rotation, which is when the shoulders emerge as the baby’s head enters the maternal pelvis. The combination of maternal muscle tone and uterine contractions cause the baby’s head to flex, chin to chest. Then the back of the baby's head emerges and finally the face.
Due to the increased pressure during labour and birth, it is normal for the baby's leading hip to be bruised and genitalia to be swollen. Babies who assumed the frank breech position in utero may continue to hold their legs in this position for some days after birth.

Vasectomy is a minor surgical procedure wherein the vasa deferentia of a man are severed, and then tied or sealed in a manner such to prevent sperm from entering the seminal stream (ejaculate). Typically done in an outpatient setting, a traditional vasectomy involves numbing (local anesthetic) of the scrotum after which 1 (or 2) small incisions are made, allowing a surgeon to gain access to the vas deferens.

When both mucosa and stroma are parts of the suspect lesion, a deep biopsy is needed. The Cervicore is designed to harvest samples from the cervix and vagina with minimal collateral injury to the surrounding tissues. The procedure is easy with minimal discomfort to the patient.

Amniotomy is the official term for artificially breaking the bag of waters during labor. It is believed that breaking the bag of waters will help to speed up an otherwise slow labor. Amniotomy is part of the Active Management of Labor practiced in some hospitals. Amniotomy is performed by a midwife or doctor. A long, thin instrument with a hook on the end is inserted into the vagina and through the cervix so it can catch and rip the bag of waters. To perform an amniotomy, the cervix must be dilated enough to allow the instrument through the cervix, generally at least a two. Why choose Amniotomy? Unlike other medical methods of starting labor, amniotomy does not add synthetic hormones to your labor. Instead it seems to stimulate your body’s own labor process. Amniotomy allows the use of an internal electronic fetal monitor. How effective is Amniotomy? Amniotomy alone is unpredictable, it may take hours for labor to start with amniotomy. Because amniotomy increases the risk for infection, most caregivers use amniotomy in combination with synthetic oxytocin. Birth does happen faster when amniotomy is combined with synthetic oxytocin than when amniotomy is used alone. Risks of Amniotomy Risks for Mother Increases the risk for infection. This risk is increased with length of time the waters are broken and with vaginal exams. Because of the infection risk, a time limit is given by which the mother must give birth. As the time limit approaches attempts to progress labor will become more aggressive. The fore waters equalize pressure on the cervix so it will open uniformly. When they are broken, the mother increases her chances of having uneven dilation. Risks for Baby Increases the risk of umbilical cord compression. The fore waters equalize pressure on the baby’s head as it presses against the cervix. When they are broken, the pressure on the baby’s head may be uneven causing swelling in some parts.
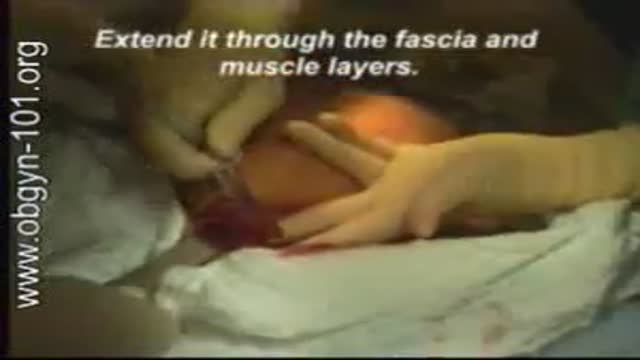
At one time, women who had delivered by cesarean section in the past would usually have another cesarean section for any future pregnancies. The rationale was that if allowed to labor, many of these women with a scar in their uterus would rupture the uterus along the weakness of the old scar. Over time, a number of observations have become apparent: Most women with a previous cesarean section can labor and deliver vaginally without rupturing their uterus. Some women who try this will, in fact, rupture their uterus. When the uterus ruptures, the rupture may have consequences ranging from near trivial to disastrous. It can be very difficult to diagnose a uterine rupture prior to observing fetal effects (eg, bradycardia). Once fetal effects are demonstrated, even a very fast reaction and nearly immediate delivery may not lead to a good outcome. The more cesarean sections the patient has, the greater the risk of subsequent rupture during labor. The greatest risk occurs following a “classical” cesarean section (in which the uterine incision extends up into the fundus.) The least risk of rupture is among women who had a low cervical transverse incision. Low vertical incisions probably increase the risk of rupture some, but usually not as much as a classical incision. Many studies have found the use of oxytocin to be associated with an increased risk of rupture, either because of the oxytocin itself, or perhaps because of the clinical circumstances under which it would be contemplated. Pain medication, including epidural anesthetic, has not resulted greater adverse outcome because of the theoretical risk of decreasing the attendant’s ability to detect rupture early. The greatest risk of rupture occurs during labor, but some of the ruptures occur prior to the onset of labor. This is particularly true of the classical incisions. Overall successful vaginal delivery rates following previous cesarean section are in the neighborhood of 70 This means that about 30of women undergoing a vaginal trial of labor will end up requiring a cesarean section. Those who undergo cesarean section (failed VBAC) after a lengthy labor will frequently have a longer recovery and greater risk of infection than had they undergone a scheduled cesarean section without labor. Women whose first cesarean was for failure to progress in labor are only somewhat less likely to be succesful in their quest for a VBAC than those with presumably non-recurring reasons for cesarean section. For these reasons, women with a prior cesarean section are counseled about their options for delivery with a subsequent pregnancy: Repeat Cesarean Section, or Vaginal Trial of Labor. They are usually advised of the approximate 70successful VBAC rate (modified for individual risk factors). They are counseled about the risk of uterine rupture (approximately 1in most series), and that while the majority of those ruptures do not lead to bad outcome, some of them do, including fetal brain damage and death, and maternal loss of future childbearing. They are advised of the usual surgical risks of infection, bleeding, anesthesia complications and surgical injury to adjacent structures. After counseling, many obstetricians leave the decision for a repeat cesarean or VBAC to the patient. Both approaches have risks and benefits, but they are different risks and different benefits. Fortunately, most repeat cesarean sections and most vaginal trials of labor go well, without any serious complications. For those choosing a trial of labor, close monitoring of mother and baby, with early detection of labor abnormalities and preparation for

Routine pelvic exams are important for good reproductive health. A woman should have her first GYN exam when she first thinks about becoming sexually active, when she becomes sexually active or when she turns 18.
At the gynecologist, you will have a short general physical exam, including a breast exam. You will wear a hospital gown and nothing else. For the actual pelvic examination, you will lie down on an examination table with your feet resting in elevated “stirrups” (props that support your legs in the air). Stirrups might look a little scary, but they are there to keep you comfortable. Your legs will be spread apart, with your knees falling to each side so that your vagina is exposed. You may feel uncomfortable, but relax and realize that everyone goes through this.
External Exam
The practitioner will visually examine your vulva for discoloration, irritation, swelling and other abnormalities, and will gently feel for glands.
Internal Exam
There are two parts to the internal exam. The first involves a speculum, a metal or plastic instrument that the practitioner inserts into the vagina. The speculum is shaped like a duck’s bill, and once it is inserted into the vaginal canal, it is gently widened to spread the interior vaginal walls (this is not painful). As the vaginal walls are spread, the practitioner is able to see the walls of the vagina itself, and up the vaginal canal to the cervix. When viewing the vaginal canal and the cervix, the practitioner can look for discoloration, abnormal discharge, lesions, growths and signs of infection. It is possible for you to look at your own cervix during this process by propping yourself up on your elbows and using a mirror. Some practitioners ask if you would like to do this, but feel free to ask to if she doesn’t mention it first.
Pap Smear
Next the practitioner will take a pap smear. She/he uses a long-stemmed cotton swab to collect a sample of cells in the cervix. Some women feel a slight cramping sensation when their cervix is touched. The collected cells are smeared onto a slide and sent to a lab for testing and examination. The pap smear is extremely important for spotting abnormalities in the cervix which may indicate infection or disease.
STD Testing
If you are sexually active, the practitioner will test for STDs. The gynecologist will swab the inside of the cervix with a long cotton swab. The speculum is then taken out of the vagina. The samples are sent to a laboratory for various STD testing. The tests will probably take a couple days. Ask when your results will be available so you can call. If you want to be tested for HIV, syphilis, genital herpes or hepatitis you need to have blood taken. They can do that as well, but you will need to ask since it is not usually routine.
Manual Exam
The second part of the pelvic exam is called the manual or bi-manual exam. The practitioner will insert one or two fingers into your vagina and press with her/his other hand on the outside of your lower abdomen. They will use a lubricant on their fingers so it is more comfortable. The person can then feel the uterus, fallopian tubes and ovaries, and check for any swelling or tenderness. Once the doctor is finished checking your uterus and ovaries, the exam is complete. The entire pelvic exam (the parts involving your vagina, cervix, uterus, and ovaries) takes 3 to 5 minutes to complete.