Physical Examination
Loyola Full Thorax Exam Part 1 A video from Loyola Medical School, Chicago showing the medical and clinical examination of the respiratory system.
Loyola Respiratory System Exam Part 2 A video from Loyola Medical School, Chicago showing the medical and clinical examination of the respiratory system.
Loyola Respiratory System Exam Part 1 A video from Loyola Medical School, Chicago showing the medical and clinical examination of the respiratory system.
Loyola Full Male Exam Part 4 A video from Loyola medical school, Chicago showing the full examination of the male
Loyola Full Male Exam Part 3 A video from Loyola medical school, Chicago showing the full examination of the male
Loyola Full Male Exam Part 2 A video from Loyola medical school, Chicago showing the full examination of the male
Loyola Full Male Exam Part 1 A video from Loyola medical school, Chicago showing the full examination of the male
A video from Loyola medical school, Chicago showing the cardiovascular medical and clinical examination
A video from Loyola medical school, Chicago showing the cardiovascular medical and clinical medical examination
Examination of the lower limbs from Loyola medical school, Chicago
Examination of the knee from Loyola medical school, Chicago
Examination of the upper limb by Loyola medical school, Chicago Part 2
Examination of the upper limb by Loyola medical school, Chicago
A video from Physical Exam Series of Loyola University Health System, Chicago showing the medical examination of the abdomen
Medical examination of the abdomen from Loyola University, Chicago
Medical breast examination of a female from Loyola University,Chicago
Clinical case discussion for exams.
Useful for medical students and others.
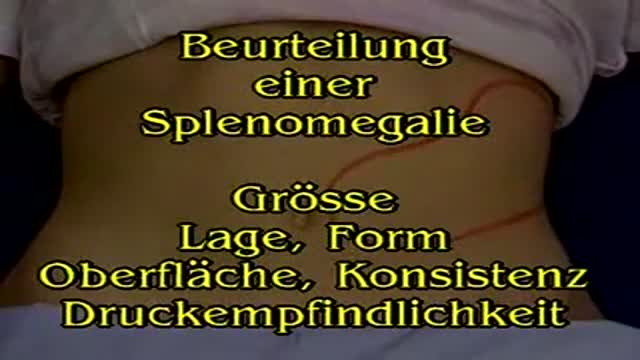
Spleen Palpation
Abdominal Aorta Palpation
Deep Palpation of the Abdomen