Underhållning
Para El Colon Irritable, Sintomas Del Colon Inflamado, Sindrome Del Intestino Irritable--- http://intestino-irritable-tratamiento.plus101.com --- La Acupuntura y el SII: Los Estudios Clínicos, Hemos investigado directamente sobre el uso de la acupuntura en comparación con la terapia de relajación en pacientes con SII. Esta investigación encontró que la calidad de vida y los síntomas gastrointestinales fueron igualmente satisfactorios en ambos grupos, logrando una reducción significativa en el dolor abdominal. Sin embargo, cuando los pacientes fueron seguidos durante un período de 4 semanas posterior a las pruebas, sólo en el grupo de acupuntura se mantuvo la reducción del dolor. Por otra parte, también se observó también una reducción significativa en la percepción del estrés en el grupo de acupuntura, pero no en el grupo de relajación. La conclusión fue que la acupuntura es una forma efectiva de tratamiento para el SII, sobre todo los síntomas de dolor y el estrés, y que sus beneficios superan a los de los tratamientos de relajación estándar. Podemos concluir que la acupuntura es un tratamiento natural válido para tratar el SII. Hay que encontrar una persona idónea para poder llevar a cabo este proceso y el mismo puede no ser efectivo en el muy corto plazo. Si quiere conocer más acerca de tratamientos naturales para eliminar los dolores causados por el SCI, no deje de visitar el sitio http://intestino-irritable-tratamiento.plus101.com
http://hidradenitis-suppurativa-cure.plus101.com --- What Is Hs, How To Get Rid Of Hidradenitis Suppurativa, Hidradenitis Suppurativa Treatment Options. What is Hidradenitis Suppurativa? Hidradenitis Suppurativa is a non-contagious skin disease that is also known as Acne Inversa. This condition affects areas of the body where there is skin to skin contact and where sweat or oil glands are present; common areas are the underarms, breasts, buttocks, anal region, and groin. It affects between 1 to 4% of the world's population, and is more likely to occur in females. Symptoms Hidradenitis Suppurativa is characterized by persistent abscesses, cysts (epidermoid, sebaceous, and pilonidal) and infections. The condition is chronic and often goes through alternating periods of remission and flare-ups. During flare-ups, the inflammation tends to be severe and patients may develop fever and be very fatigued. The pain can be unbearable and the person's movements will be very limited. The abscesses often drain pus and leave open wounds that may not heal. Eventually, abscesses may become interconnected through tunnels under skin and this makes the condition harder to treat. Causes The immediate cause of Hidradenitis Suppurativa is clogging of the apocrine glands, due to dead skin cells become trapped in the gland, over production of oil, or bacterial accumulation. This will cause the plug to swell with pus formation. What causes this simple blockage to progress into a full blow Hidradenitis Suppurativa case is still debated, however, possible theories include an auto-immune reaction, hormone imbalances and genetic disorders. It is also known that excessive sweating and being overweight will increase the risk of developing the condition. Furthermore, wearing tight clothing, excessive shaving, using lithium medications and hot humid climates have been identified as triggering factors. For a complete guide on curing Hidradenitis Suppurativa through a natural and holistic approach, visit http://hidradenitis-suppurativa-cure.plus101.com
Learn How to Give an Intramuscular Injection
http://tinnitus-solution.info-pro.co --- Ear Infection, Loud Ringing In Ears, Tinnitus Suicide, Ear Is Ringing, Tinnitus One Ear, Tinnitus. Do you suddenly get up in the middle of the night hearing strange noises? Yes it can definitely be frightening, more so when you cannot find the source. Now consider for a moment that these sounds are coming from within you. Most people would be stunned to know that. Many of us do not even know that our internal organs can make sounds. Let us try to see whether you actually heard these noises or not, and if you did, where did they come from. Now before anything, let us get this straight - yes, you actually heard those noises. No, they are not a result of a creative mind that imagined things in slumber. But having said that, it is also true that there is indeed no source of the sounds you heard. So what is it? Confused? This is a classic case of tinnitus. What is tinnitus? What you experienced last night (or did you just get up from sleep and switch on the computer) is a classic case of tinnitus. This is a medical condition wherein a person hears all kinds of strange clicking, ringing, buzzing, whistling or hissing sounds within the ear. What's so worrisome about this condition for a lot of people is that, there's actually no physical source of these sounds. What makes it even worse is that, no one else seems to hear them. Frankly, these people cannot be really blamed. Naturally, if you cannot see where the sound is coming from, and if you keep hearing it, you are bound to get worried. In tinnitus, the sounds a person hears are actually perceptions. Since there's no actual source, they are often referred to as "phantom noises". Will it help you if you knew that about 8% of all people in the US suffer from tinnitus? Perhaps not, but at least now you know that you are not alone who hears these strange noises. Cure tinnitus. this simple, but effective system to erasing Tinnitus out of your life for good has now helped cure over 105,302 people of all the frustrating ringing, hissing, buzzing. Even if you’ve tried every single tinnitus treatment or remedy under the sun. 100% natural tinnitus cure click here: http://tinnitus-solution.info-pro.co
Watch that video to learn How to Give an Intramuscular Injection
Wow! Ultrasound guided internal jugular vein cannulation (long axis approach)
How do you assess cerebellar function? Ask them to do this as fast as possible while you slowly move your finger. Repeat the test with the other hand. Perform the heel-to-shin test. Have the patient lying down for this and get them to run the heel of one foot down the shin of the other leg, and then to bring the heel back up to the knee and start again.
The principal signs of cerebellar dysfunction are the following: Ataxia: unsteadiness or incoordination of limbs, posture, and gait. A disorder of the control of force and timing of movements leading to abnormalities of speed, range, rhythm, starting, and stopping.
In a normal person, when a muscle tendon is tapped briskly, the muscle immediately contracts due to a two-neuron reflex arc involving the spinal or brainstem segment that innervates the muscle. The afferent neuron whose cell body lies in a dorsal root ganglion innervates the muscle or Golgi tendon organ associated with the muscles; the efferent neuron is an alpha motoneuron in the anterior horn of the cord. The cerebral cortex and a number of brainstem nuclei exert influence over the sensory input of the muscle spindles by means of the gamma motoneurons that are located in the anterior horn; these neurons supply a set of muscle fibers that control the length of the muscle spindle itself.
Start in RLQ (so you don’t miss a giant spleen). Get your fingers set then ask patient to take a deep breath. Don’t dip your fingers or do anything but wait. When patient expires, take up new position. Note lowest point of spleen below costal margin, texture of splenic contour, and tenderness If spleen is not felt, repeat with pt lying on right side. Gravity may bring spleen within reach. “LET THE SPLEEN PALPATE YOUR FINGERS AND NOT THE OTHER WAY AROUND. THERE IS NO GOLD, SO DON’T DIG!”
About Us Contact Disclaimer Get Published! Follow Us Epomedicine Medical Students Clinical Discussion Cases Emergencies Blog Medical Mnemonics Clinical Skills Search Subjects Clinical examination Gastrointestinal system Internal medicine Updated on January 31, 2017 Percussion of Spleen Traube’s semilunar space Borders: Superiorly: Left 6th rib superiorly Laterally: Left midaxillary line or Left anterior axillary line Inferiorly: Left costal margin Method: Patient’s position: supine with left arm slightly abducted. Percuss: from medial to lateral Interpretation: Resonance (Normal) and Dullness (Splenomegaly) Also: Pleural effusion or mass in stomach may cause dullness in Traube’s space.
Exam- COPD Patient
This video demonstrates the process for preparing and administering an intramuscular injection (IM)
This video demonstrates a boatload of excellent teaching points on how to perform a peritoneal tap to remove ascites fluid from the peritoneum.
Paracentesis is a procedure to take out fluid that has collected in the belly (peritoneal fluid). This fluid buildup is called ascites . Ascites may be caused by infection, inflammation, an injury, or other conditions, such as cirrhosis or cancer. The fluid is taken out using a long, thin needle put through the belly.
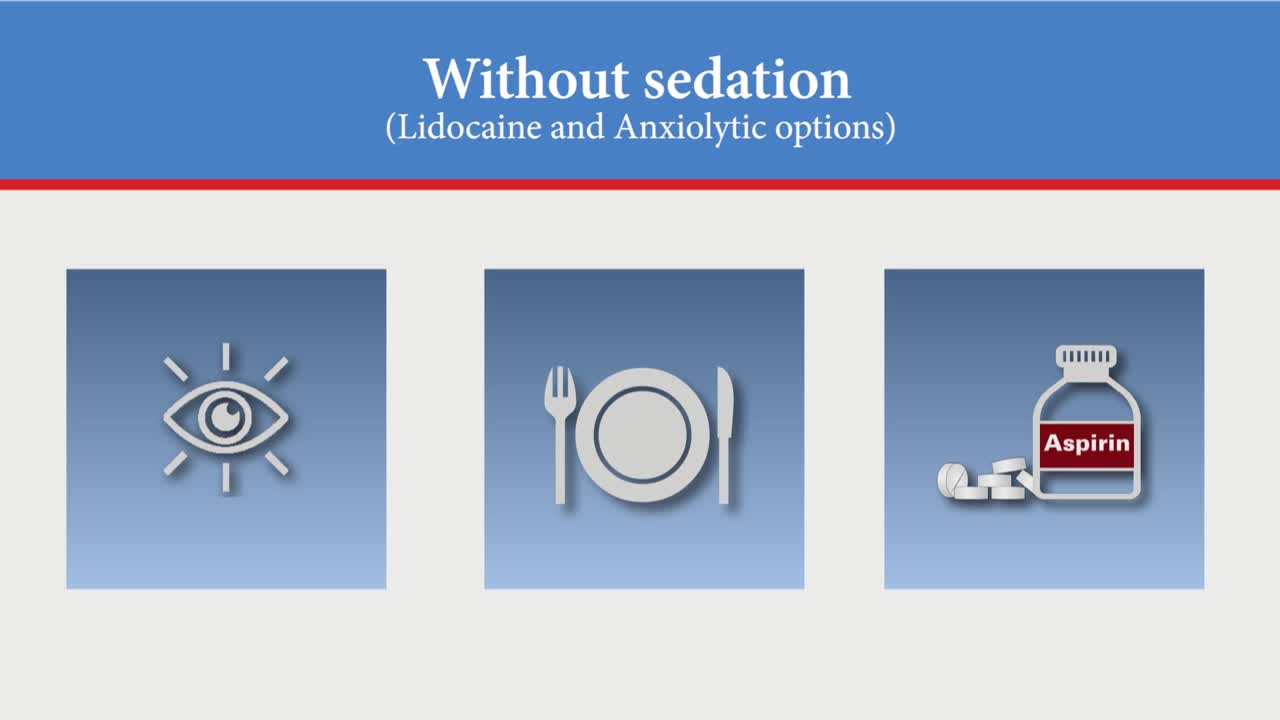
INDICATIONS Administration of agents into the central vasculature Central circulation and intracardiac access Maintenance of venous access Hemodialysis and plasmapheresis
Arterial line placement is a common procedure in various critical care settings. Intra-arterial blood pressure (BP) measurement is more accurate than measurement of BP by noninvasive means, especially in the critically ill. [1] Intra-arterial BP management permits the rapid recognition of BP changes that is vital for patients on continuous infusions of vasoactive drugs. Arterial cannulation also allows repeated arterial blood gas samples to be drawn without injury to the patient.
Biliary Colic Examination
A bone marrow biopsy removes a small amount of bone and a small amount of fluid and cells from inside the bone (bone marrow). A bone marrow aspiration removes only the marrow. These tests are often done to find the reason for many blood disorders and may be used to find out if cancer or infection has spread to the bone marrow. Bone marrow aspiration removes a small amount of bone marrow fluid and cells through a needle put into a bone. The bone marrow fluid and cells are checked for problems with any of the blood cells made in the bone marrow. Cells can be checked for chromosome problems. Cultures can also be done to look for infection. A bone marrow biopsy removes bone with the marrow inside to look at under a microscope. The aspiration (taking fluid) is usually done first, and then the biopsy.
Markle Test (heel jar test) for Peritonitis