Latest videos
Tooth preparation for All-ceramic crown
Art restoration of anterior teeth
Learn how to give an intramuscular injection
Opening of the Cranium
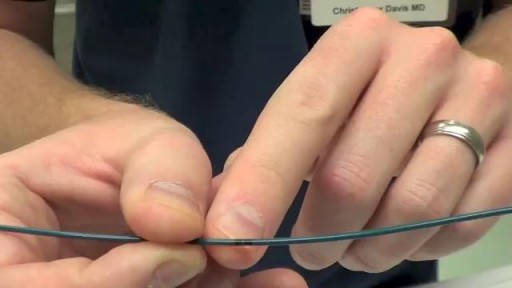
Transvenous cardiac pacing, also called endocardial pacing, is a potentially life saving intervention used primarily to correct profound bradycardia. It can be used to treat symptomatic bradycardias that do not respond to transcutaneous pacing or to drug therapy.
In emergencies (eg, asystole), transcutaneous pacing should be tried first. If transvenous pacing is tried, the catheter should be advanced during asynchronous pacing at maximum output until the ventricle has been captured and a palpable pulse is detected in the patient.
A pacemaker insertion is the implantation of a small electronic device that is usually placed in the chest (just below the collarbone) to help regulate slow electrical problems with the heart.
An AV fistula is a connection, made by a vascular surgeon, of an artery to a vein.Vascular surgeons specialize in blood vessel surgery. The surgeon usually places an AV fistula in the forearm or upper arm. An AV fistula causes extra pressure and extra blood to flow into the vein, making it grow large and strong.
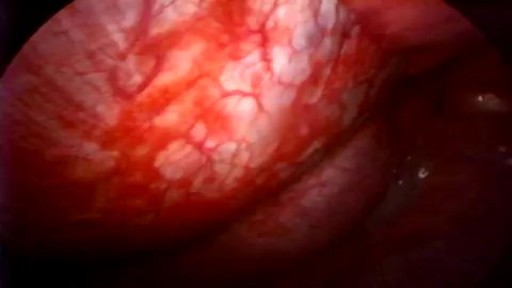
If you have a lung disease, a type of surgery called a lobectomy is one treatment option your doctor may suggest. Your lungs are made up of five sections called lobes. You have three in your right lung and two in your left. A lobectomy removes one of these lobes. After the surgery, your healthy tissue makes up for the missing section, so your lungs should work as well or better than they did before.
A chalazion is a swollen bump on the eyelid. It happens when the eyelid’s oil gland clogs up. It may start as an internal hordeolum (stye). At first, you might not know you have a chalazion as there is little or no pain. But as it grows, your eyelid may get red, swollen, and sometimes tender to touch. If the chalazion gets large, it can press on your eye and cause blurry vision. Rarely, the whole eyelid might swell.
A stye (also called a hordeolum) is a small, red, painful lump that grows from the base of your eyelash or under the eyelid. Most styes are caused by a bacterial infection. There are two kinds of styes: External hordeolum: A stye that begins at the base of your eyelash. Most are caused by an infection in the hair follicle. It might look like a pimple. Internal hordeolum: A stye inside your eyelid. Most are caused by an infection in an oil-producing gland in your eyelid.
The clinician performing the procedure should be familiar with the anatomy of the specific joint and cognizant of the relevant landmarks in order to avoid puncture of tendons, blood vessels, and nerves (see the images below).
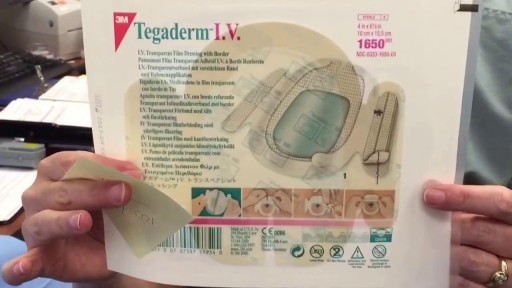
First described by Aubaniac in 1952, central venous catheterization, or central line placement, is a time-honored and tested technique of quickly accessing the major venous system. Benefits over peripheral access include greater longevity without infection, line security in situ, avoidance of phlebitis, larger lumens, multiple lumens for rapid administration of combinations of drugs, a route for nutritional support, fluid administration, and central venous pressure (CVP) monitoring. Central vein catheterization is also referred to as central line placement. Overall complication rates are as high as 15%, [1, 2, 3, 4] with mechanical complications reported in 5-19% of patients, [5, 6, 7] infectious complications in 5-26%, [1, 2, 4] and thrombotic complications in 2-26%. [1, 8] These complications are all potentially life-threatening and invariably consume significant resources to treat. Placement of a central vein catheter is a common procedure, and house staff require substantial training and supervision to become facile with this technique. A physician should have a thorough foreknowledge of the procedure and its complications before placing a central vein catheter. The supraclavicular approach was first put into clinical practice in 1965 and is an underused method for gaining central access. It offers several advantages over the infraclavicular approach to the subclavian vein. At the insertion site, the subclavian vein is closer to the skin, and the right-side approach offers a straighter path into the subclavian vein. In addition, this site is often more accessible during cardiopulmonary resuscitation (CPR) and during active surgical cases. Finally, in patients who are obese, this anatomic area is less distorted.
Pericardiocentesis is the aspiration of fluid from the pericardial space that surrounds the heart. This procedure can be life saving in patients with cardiac tamponade, even when it complicates acute type A aortic dissection and when cardiothoracic surgery is not available. [1] Cardiac tamponade is a time sensitive, life-threatening condition that requires prompt diagnosis and management. Historically, the diagnosis of cardiac tamponade has been based on clinical findings. Claude Beck, a cardiovascular surgeon, described 2 triads of clinical findings that he found associated with acute and chronic cardiac tamponade. The first of these triads consisted of hypotension, an increased venous pressure, and a quiet heart. It has come to be recognized as Beck's triad, a collection of findings most commonly produced by acute intrapericardial hemorrhage. Subsequent studies have shown that these classic findings are observed in only a minority of patients with cardiac tamponade. [2] The detection of pericardial fluid has been facilitated by the development and continued improvement of echocardiography. [3] Cardiac ultrasound is now accepted as the criterion standard imaging modality for the assessment of pericardial effusions and the dynamic findings consistent with cardiac tamponade. With echocardiography, the location of the effusion can be identified, the size can be estimated (small, medium, or large), and the hemodynamic effects can be examined by assessing for abnormal septal motion, right atrial or right ventricular inversion, and decreased respiratory variation of the diameter of the inferior vena cava
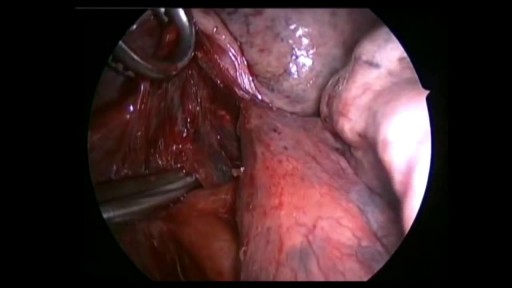
Video-assisted thoracoscopic talc pleurodesis is a highly effective technique to manage recurrent pneumothorax or pleural effusion.Surgical treatment using thoracoscopy may hasten postoperative recovery and reduce hospital stay.
Spontaneous pneumothorax is a life-threatening condition in patients with severe underlying lung disease; thus, tube thoracostomy is the procedure of choice in SSP. Pleurodesis decreases the risk of recurrence, as does thoracotomy or video-assisted thoracoscopic surgery (VATS) to excise the bullae
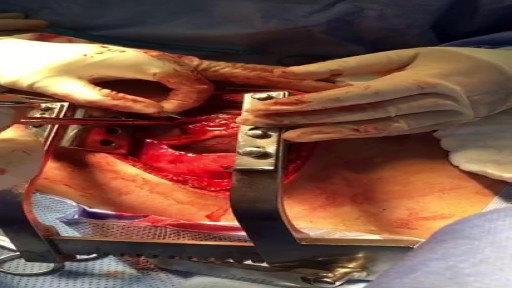
Pericardial window is used diagnostically and, more often, therapeutically for drainage of accumulated pericardial fluid (a condition that most often occurs after cardiac surgery but has many other possible causes). The pericardium envelops the heart like a cocoon; its cardiac filling can be impaired when this cavity fills with excess fluid. When the limited space between the noncompliant pericardium and heart is acutely filled with blood or fluid, cardiac compression and tamponade may result. Pericardial window in combination with systemic chemotherapy may also prevent accumulation of large fluid volumes in patients with neoplastic pericardial disease. [1, 2] Indications The following are indications for a pericardial window [6] : Symptomatic pericardial effusions Asymptomatic pericardial effusions that warrant a pericardial window for diagnosis Hemodynamically stable patients with an undiagnosed pericardial effusion (a thoracoscopic approach is ideal) Coexisting pericardial, pleural, or pulmonary pathology that requires diagnosis or therapy (a thoracoscopic approach is ideal) Known benign effusions that reaccumulate after aspiration Drainage of a purulent pericardial effusion Early fungal or tuberculous pericarditis in which resection of the pericardium is required to prevent future pericardial constriction Use as part of the mediastinal debridement, in patients with descending mediastinitis
30 yr old man presented to ER after Motor Vehicle Crash..blunt chest trauma...