最新の動画
Diagnosis of HIV infection in infants is aided by HIV culture or DNA/RNA polymerase chain reaction (PCR); positive results are confirmed by repeating the test. In suspected cases, HIV testing should occur in the newborn period (ie, before the infant is 48 h old), at age 1-2 months, and again at age 3-6 months.
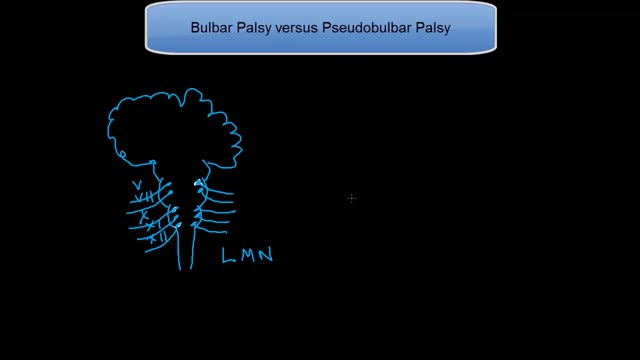
Tongue fassiculations
This tutorial explains the difference in mechanisms between the 2 palsies. Bulbar palsy is a lower motor neuron condition and pseudobulbar palsy is an upper motor neuron condidtion.
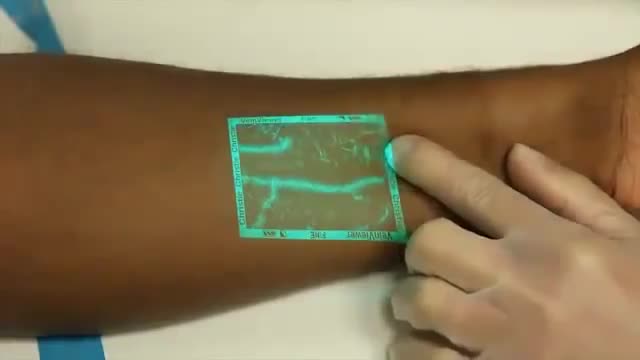
Venipuncture can be a challenging process for medical professionals especially when a patients veins are difficult to see. VeinViewer uses near infrared light to create a digital image of patient vasculature in real time.
Beckwith-Wiedemann Syndrome (BWS) is a congenital overgrowth syndrome, which can affect all systems of the body. It was first recognised in 1963-64 by Dr J. Bruce Beckwith, a paediatric pathologist in America and, independently, by Dr H.E. Wiedemann, a German geneticist.
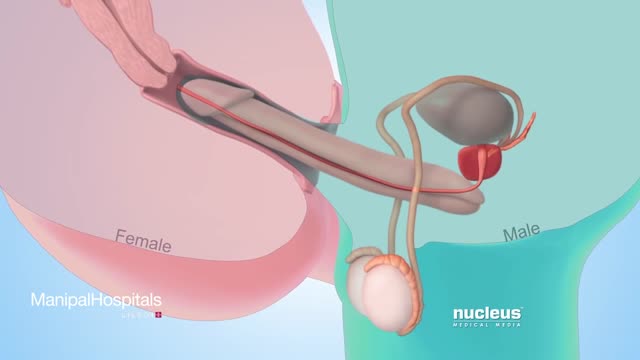
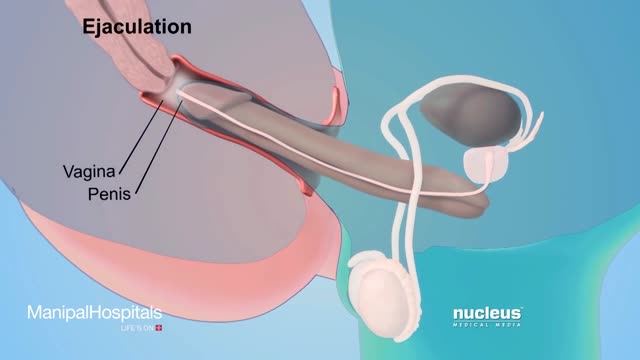
Testicular sperm aspiration (TESA) is a procedure performed for men who are having sperm retrieved for in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). It is done with local anesthesia in the operating room or office and is coordinated with their female partner's egg retrieval.
How To Use Male Condom Correctl
Female Condom Demonstration
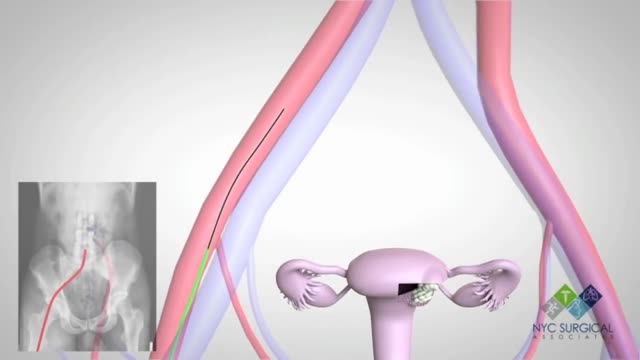
Dilation and curettage (D&C) is a procedure to remove tissue from inside your uterus. Doctors perform dilation and curettage to diagnose and treat certain uterine conditions — such as heavy bleeding — or to clear the uterine lining after a miscarriage or abortion. In a dilation and curettage — sometimes spelled "dilatation" and curettage — your doctor uses small instruments or a medication to open (dilate) your cervix — the lower, narrow part of your uterus. Your doctor then uses a surgical instrument called a curette to remove uterine tissue. Curettes used in a D&C can be sharp or use suction
Dilation and curettage (D&C) is a procedure to remove tissue from inside your uterus. Doctors perform dilation and curettage to diagnose and treat certain uterine conditions — such as heavy bleeding — or to clear the uterine lining after a miscarriage or abortion.
Hysteroscopy is a procedure that allows your doctor to look inside your uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
There's no single best approach to uterine fibroid treatment — many treatment options exist. If you have symptoms, talk with your doctor about options for symptom relief. Watchful waiting Many women with uterine fibroids experience no signs or symptoms, or only mildly annoying signs and symptoms that they can live with. If that's the case for you, watchful waiting could be the best option. Fibroids aren't cancerous. They rarely interfere with pregnancy. They usually grow slowly — or not at all — and tend to shrink after menopause, when levels of reproductive hormones drop. Medications Medications for uterine fibroids target hormones that regulate your menstrual cycle, treating symptoms such as heavy menstrual bleeding and pelvic pressure. They don't eliminate fibroids, but may shrink them. Medications include: Gonadotropin-releasing hormone (Gn-RH) agonists. Medications called Gn-RH agonists (Lupron, Synarel, others) treat fibroids by blocking the production of estrogen and progesterone, putting you into a temporary postmenopausal state. As a result, menstruation stops, fibroids shrink and anemia often improves. Your doctor may prescribe a Gn-RH agonist to shrink the size of your fibroids before a planned surgery. Many women have significant hot flashes while using Gn-RH agonists. Gn-RH agonists typically are used for no more than three to six months because symptoms return when the medication is stopped and long-term use can cause loss of bone. Progestin-releasing intrauterine device (IUD). A progestin-releasing IUD can relieve heavy bleeding caused by fibroids. A progestin-releasing IUD provides symptom relief only and doesn't shrink fibroids or make them disappear. It also prevents pregnancy. Tranexamic acid (Lysteda). This nonhormonal medication is taken to ease heavy menstrual periods. It's taken only on heavy bleeding days. Other medications. Your doctor might recommend other medications. For example, oral contraceptives or progestins can help control menstrual bleeding, but they don't reduce fibroid size. Nonsteroidal anti-inflammatory drugs (NSAIDs), which are not hormonal medications, may be effective in relieving pain related to fibroids, but they don't reduce bleeding caused by fibroids. Your doctor may also suggest that you take vitamins and iron if you have heavy menstrual bleeding and anemia
#STOP VIOLENCE AGAINST DOCTORS#SAVE THE DOCTOR
STOP VIOLENCE AGAINST DOCTORs
today we talk about Amniotic fluid during your pregnancy! Looking forward to your comments.
How to Get Rid of Vaginal Discharge - Treating Normal Discharge.
Pregnancy is one of the beautiful phases of a woman’s life after their marriage. The feeling of the baby growing inside the womb is exceptional and very special.
A lot of women want to know what type of vaginal discharge is normal during pregnancy, and when you're not pregnant. So let's start out by talking about what's normal when you're not pregnant. It's normal to have about 1/2 teaspoon to 1 teaspoon of whitish, creamy, tannish discharge on most days of your cycle in between periods, with the exception of the time of ovulation. Actually, around the time of ovulation, it's normal to notice the discharge becoming more slippery and clear, almost like egg whites. And this is actually a sign that you can watch for to know when you're ovulating. And if you're seeing this type of discharge and you're trying to have a baby, then you should start to time intercourse with ovulation to increase your chances of conceiving.
It sounds like you're questioning whether or not your water may have broken, and this can actually be a hard thing for a lot of women to tell. Usually if your water breaks, it's just a trickle of fluid, and you're afraid to admit it to anyone because you think you peed your pants. And it is normal to pee your pants when you're pregnant because the bladder is right below the uterus, and if the baby moves just right, it might kick out a little bit of urine. So if you feel a trickle or a little tiny gush of fluid, what you want to do is put a pad or a pantie-liner on after going to the bathroom and emptying your bladder, and wait an hour and see if fluid continues to come out. And if it does, then you're not having bladder leakage issues - your water is probably broken.
Women are routinely invited to have cervical screening tests (also called smear tests). The tests are done to prevent cervical cancer, not to diagnose cancer. During each test some cells are removed from the neck of the womb (cervix), with a plastic brush. The cells are examined under a microscope to look for early changes that, if ignored and not treated, could develop into cancer of the cervix. You are very unlikely to develop cervical cancer if you have regular cervical screening tests at the times advised by your doctor. If the test shows any abnormality, you will have treatment to stop you ever getting cancer of the cervix. So, an abnormal test does not mean you have cancer. It means you should have some treatment to stop you getting cancer.