Latest videos

Attention deficit hyperactivity disorder (ADHD) is a mental disorder of the neurodevelopmental type. It is characterized by problems paying attention, excessive activity, or difficulty controlling behavior which is not appropriate for a person's age.

attention deficit hyperactivity disorder (ADHD). Recent evidence supports initial treatment with nonpharmacological interventions (behavior therapy) in preschool age children (3- 5). Parent-child behavioral therapy improves problem behaviors and parent-child relationships. It involves teaching parents to consistently implement effective behavioral techniques (eg, rewards and non-punitive consequences to shape behavior, calm limit setting, structured daily schedules, minimizing distractions). Behavioral interventions can also be used in patients who do not meet full ADHD criteria or in combination with medication for school-aged children and adolescents with ADHD. Medication in preschool children should be considered when behavioral therapy fails or the child's function is severely impaired (repeatedly expelled from day care or school, risks injuring others). The family's preferences and values should always be considered in treatment decisions.
St. John's wort (Hypericum perforatum) is an over-the-counter herbal supplement used for its antidepressant, anti-inflammatory, and wound-healing properties. Although it has been prescribed in Europe for mild to moderate depression, negative clinical trials and multiple reports of adverse drug interactions have raised concern about its use. St. John's wort induces various P450 isozymes (CYP 1A2, 2C19, 2C9, and 3A4) and P-glycoprotein systems. Drug interactions with the herbal product can lead to treatment failures with many medications, including hormonal contraceptives, antiretrovirals, immunosuppressive agents, narcotics, anticoagulants, and antifungals. There is also a risk for serotonin syndrome when St. John's wort is used in combination with other serotonergic antidepressants. The lack of strict regulation of herbal products that results in variable quality and content (unknown toxic ingredients or inactive ingredients) is also a concern.

While an anal abscess is an infection within one or more of the anal spaces, an anal fistula (Choice B) is a tunneling between the anus or rectum and another epithelial lined space (eg, the skin overlying the drainage site). Fifty percent of patients with anal abscesses will go on to develop a chronic fistula from the involved anal gland to the overlying skin. Patients with fistulas typically present with an anal abscess that persists after incision and drainage, or with a pustule-like lesion in the perianal or ischiorectal area that continually drains. Surgical repair is usually necessary to eliminate the fistula while preserving fecal continence.

-The cremasteric reflex test is considered positive if there is elevation of the testis in response to stroking the upper inner thigh. This reaction is typically absent in testicular torsion and boys under the age of 6 months. Although not completely reliable in older boys and adults, an absent cremasteric reflex is highly suggestive of torsion. Patients with epididymitis usually have a normal cremasteric reflex, with pain and swelling isolated to
This syndrome was previously known as reflex sympathetic dystrophy, algodystrophy, causalgia, Sudeck atrophy, transient osteoporosis, and acute atrophy of bone. Usually occurring after an injury, CRPS presents with pain out of proportion to the injury, temperature change, edema, and abnormal skin color. Type I CRPS (90% of CRPS cases) occurs without a definable nerve lesion, while type II occurs with a definable nerve lesion. The pathogenesis is likely due to an injury causing increased sensitivity to sympathetic nerves, an abnormal response to and sensation of pain, and increased neuropeptide release causing burning pain to light touch (allodynia).

-Tibial stress fractures are common in athletes and nonathletes who suddenly increase their physical activity. Clinical features include pain, localized tenderness, and swelling. Plain x-ray is <50% sensitive for stress fractures, especially in the first 2-3 weeks after the onset of symptoms. MRI is preferred over bone scan or ultrasound as it can show the fracture line that extends through the cortex into the medullary line. MRI can also identify ligament, muscle, and cartilage injuries. However, MRI findings may be persistently abnormal for up to 1 year after the stress fracture has healed.
A stress fracture typically feels like an aching or burning localized pain somewhere along a bone. Usually, it will hurt to press on it, and the pain will get progressively worse as you run on it, eventually hurting while walking or even when you're not putting any weight on it at all.

Porcelain gallbladder is a condition characterized by calcium salt deposits in the wall of a chronically inflamed gallbladder. The calcifications can be thin or faintly visible, or may be amorphous, patchy, and thick. The gallbladder is generally large, but its size can vary considerably. Most porcelain gallbladders are associated with gallstones. A plain radiograph generally detects these, but computed tomography (CT) has a higher specificity; therefore, a CT scan is performed to confirm the diagnosis. Due to their high risk of gallbladder carcinoma, all patients with porcelain gallbladder should have an elective cholecystectomy.
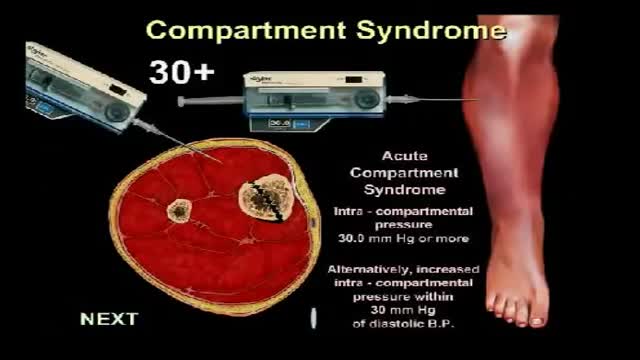
Acute compartment syndrome refers to ischemic tissue damage secondary to elevated pressures in the enclosed compartments of the lower legs or forearm. When the tissue pressure in an enclosed compartment exceeds the perfusion pressure, the resulting diminished tissue perfusion and compromised blood flow to the muscles and nerves inevitably lead to ischemic tissue necrosis. Majority of the cases involving the lower extremities are due to a traumatic event, most commonly tibial fractures. Other causes include a crush injury or other long bone fractures in a motor vehicle accident, a tight cast or dressing after trauma, and drug overdose.

-Traumatic amputation of a body part requires rapid transport of the appendage, which should be wrapped in a saline-moistened gauze, placed in a plastic bag, and transported in a container filled with ice mixed with either saline or sterile water to best preserve the body part and attempt replantation.
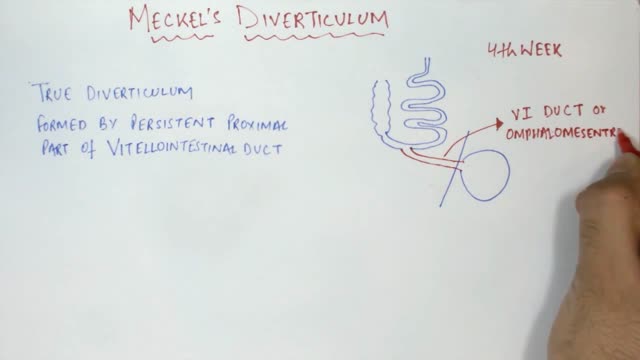
The differential diagnosis for this child's painless hematochezia includes Meckel's diverticulum as well as vascular malformations. Meckel's diverticulum results from a failure of the vitelline duct to obliterate during the first 8 weeks of gestation, leaving behind a blind pouch often containing ectopic gastric tissue. Meckel's diverticulum classically affects children age ~:2 but can also occur in older children or even adults. Young children are more likely to experience painless bleeding due to mucosal irritation from gastric acid; adolescents and adults are more likely to have signs of obstruction. A technetium-99 nuclear scan will identify the diverticulum, which is usually located in the right lower quadrant of the abdomen within 2 feet of the ileocecal valve. Technetium-99 concentrates in the parietal cells of the diverticulum and stomach. The scan is also known as "Meckel's scan" due to its high specificity. A symptomatic Meckel's diverticulum is generally treated with surgical resection.

A patient who has a problem with proprioception can still maintain balance by using vestibular function and vision. In the Romberg test, the standing patient is asked to close his or her eyes. A loss of balance is interpreted as a positive Romberg's test.

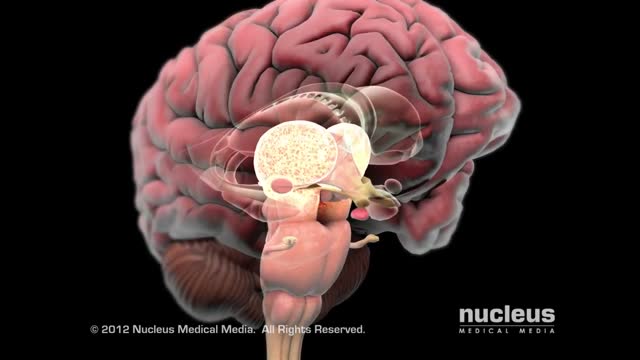
Definition. The principal signs of cerebellar dysfunction are the following: Ataxia: unsteadiness or incoordination of limbs, posture, and gait. A disorder of the control of force and timing of movements leading to abnormalities of speed, range, rhythm, starting, and stopping.