Latest videos
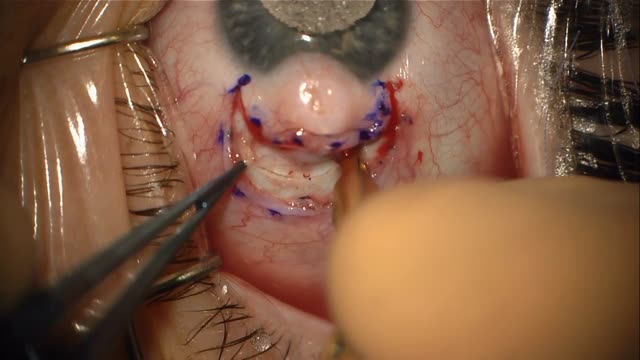
Limbal dermoid is a congenital growth on the eye that forms from germline cells that get trapped in this region during embryogenesis. The dermoid often has tissue from multiple germ layers including hair and fat. Dermoids on the eye can cause astigmatism and be unsightly.

McMurray's maneuver is used to detect the presence of meniscal tears. To detect a medial meniscal injury, the patient is put in a supine position with the knee in maximum flexion. One hand of the examiner is placed on the posteromedial margin of the involved knee and the other hand supports the foot. The tibia is then externally rotated, and the knee is extended slowly. The test is positive if there is an audible or palpable click or popping sensation during extension of the involved knee.
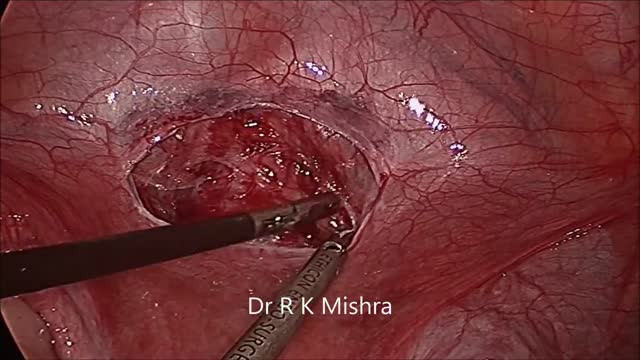
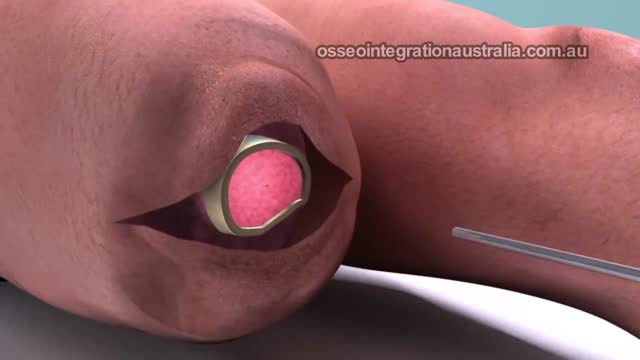
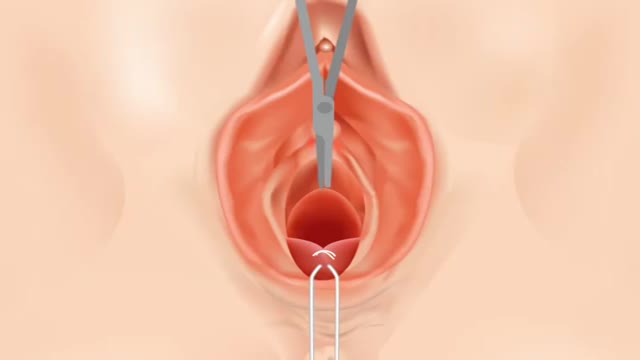
Cervical cerclage can be placed via transvaginal, open transabdominal, or laparoscopic transabdominal approach, preferably before pregnancy. Recurrent late miscarriages may be due to a weak (sometimes called an incompetent) cervix that shortens or opens too early in pregnancy. Cervical cerclage involves placing a stitch around the upper part of the cervix to keep it closed; the operation may be carried out through the vagina, or through the abdomen, as an open or laparoscopic ('keyhole') procedure.
Cerclage is indicated in a patient with a history of painless cervical dilation and a second trimester loss. It is also indicated in a patient with a history of preterm birth and a short cervix found on ultrasound between 16-24 weeks gestation. Cerclage placement occurs after the first trimester in case the pregnancy is genetically abnormal and would likely result in a first trimester loss.

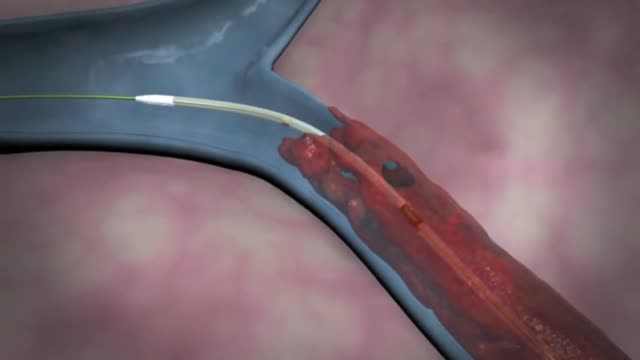
Defibrillation is a treatment for life-threatening cardiac dysrhythmias, specifically ventricular fibrillation (VF) and non-perfusing ventricular tachycardia (VT). A defibrillator delivers a dose of electric current (often called a countershock) to the heart.
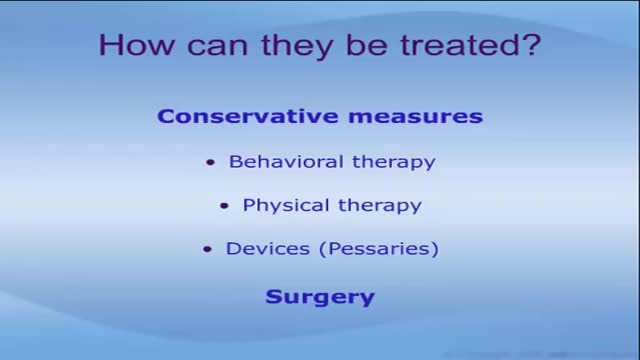
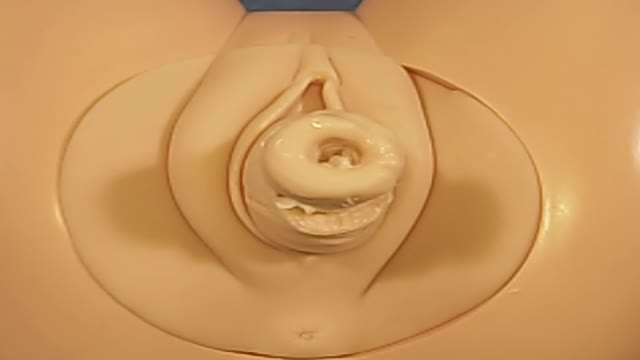
Pelvic organ prolapse occurs when a pelvic organ-such as your bladder-drops (prolapses) from its normal place in your lower belly and pushes against the walls of your vagina. This can happen when the muscles that hold your pelvic organs in place get weak or stretched from childbirth or surgery.

Vaginal prolapse (also called vaginal vault prolapse) is quite common after a hysterectomy (surgery to remove the uterus), but not everyone who has a hysterectomy experiences POP. Without the uterine attachments to hold it up, the top of the vagina can drop into the vaginal canal.
The cause of HELLP syndrome is unknown, but there are certain factors that may increase your risk of developing it. Preeclampsia is the greatest risk factor. This condition is marked by high blood pressure and swelling, and it typically occurs during the last trimester of pregnancy.

Formerly called toxemia, preeclampsia is a condition that pregnant women develop. It is marked by high blood pressure in women who have previously not experienced high blood pressure before. Preeclamptic women will have a high level of protein in their urine and often also have swelling in the feet, legs, and hands.
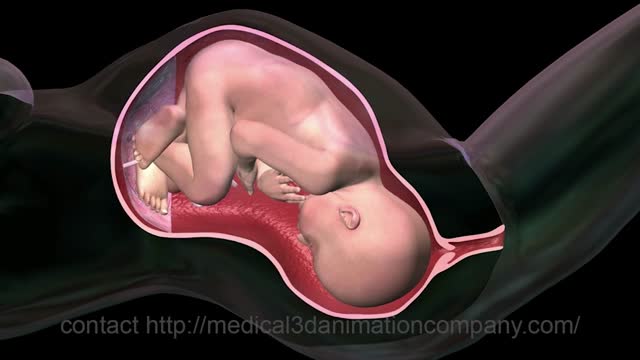
Chorionic villus sampling, often referred to as CVS, is a diagnostic test for identifying chromosome abnormalities and other inherited disorders. This test may be recommended by your health care provider, if you or your partner has family medical histories that reveal potential risks.
Adenomyosis is a condition in which the inner lining of the uterus (the endometrium) breaks through the muscle wall of the uterus (the myometrium). Adenomyosis can cause menstrual cramps, lower abdominal pressure, and bloating before menstrual periods and can result in heavy periods.