Latest videos
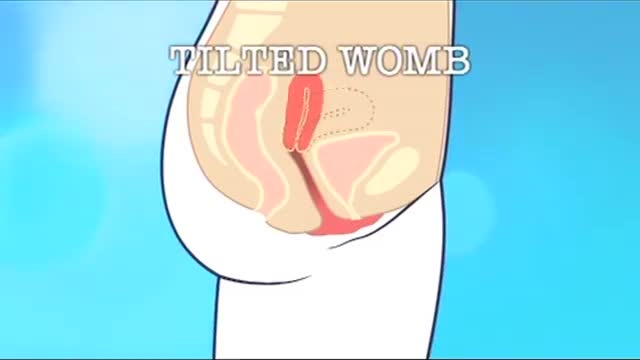
A retroverted uterus (tilted uterus, tipped uterus) is a uterus that is tilted posteriorly. This is in contrast to the slightly "anteverted" uterus that most women have, which is tipped forward toward the bladder, with the anterior end slightly concave.

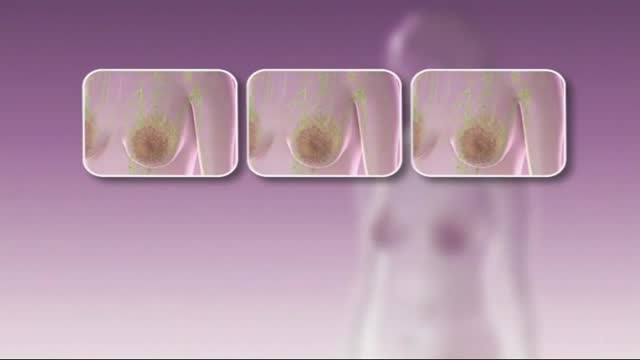
For both DCIS and invasive cancer, radiation therapy to the remaining breast tissue is generally recommended after surgery. A lumpectomy may also be called breast-conserving surgery, a partial mastectomy, quadrantectomy, or a segmental mastectomy. A mastectomy is the surgical removal of the entire breast.
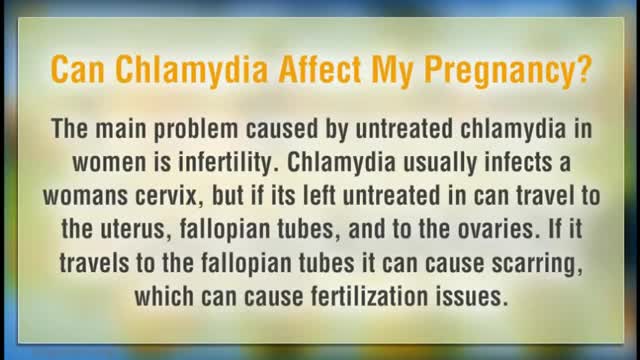
all pregnant women be screened for Chlamydia at the first prenatal visit. Women under age 25 and those at increased risk for chlamydia! Infection should have repeat testing in the third trimester. Chlamydia endometritis during pregnancy can lead to chorioamnionitis and premature delivery of the fetus. Untreated infection during pregnancy can also lead to conjunctivitis (ophthalmia neonatorum) and pneumonia in the newborn baby
The maneuver is commonly used during some activities: Straining to have a bowel movement Blowing a stuffy nose Certain medical tests or exams As a pressure equalization technique by scuba divers, sky divers and airplane passengers The effect of the Valsalva Maneuver is a drastic increase in the pressure within the thoracic cavity.