Latest videos

A simple test of fingernail clippings could replace a blood draw as a way to diagnose and monitor type 2 diabetes mellitus (T2DM), with huge implications for tracking the disease in the developing world. Research on this method by a team of Belgian researchers was reported July 28, 2015, at the 2015 American Association for Clinical Chemistry (AACC) Annual Meeting and Clinical Lab Expo in Atlanta. The team, led by Joris R. Delanghe, MD, PhD, of the Department of Global Chemistry, Microbiology and Immunology at Ghent University, collected nail clippings from 25 people with T2DM and 25 without the disease. The clippings were ground into a powder and tested with an inexpensive FT-IR photometer to measure how much the protein in the nails had bonded with sugar molecules, a process known as glycation. “We found a striking difference in the measurements between the control group and the patients with diabetes,” Delanghe said. In an interview with Evidence-Based Diabetes Management, he said replacing the standard blood test to measure glycated hemoglobin is a huge advantage. In many cultures, he said, “Taking blood is something that cannot be tolerated.” - See more at: http://www.ajmc.com/journals/evidence-based-diabetes-management/2015/september-2015/fingernail-tests-may-offer-cheap-simple-way-to-diagnose-diabetes#sthash.XQxnBcNO.dpuf

Prediabetes means that your blood sugar level is higher than normal but not yet high enough to be type 2 diabetes. Without lifestyle changes, people with prediabetes are very likely to progress to type 2 diabetes. If you have prediabetes, the long-term damage of diabetes — especially to your heart, blood vessels and kidneys — may already be starting. There's good news, however. Progression from prediabetes to type 2 diabetes isn't inevitable. Eating healthy foods, incorporating physical activity in your daily routine and maintaining a healthy weight can help bring your blood sugar level back to normal. Prediabetes affects adults and children. The same lifestyle changes that can help prevent progression to diabetes in adults might also help bring children's blood sugar levels back to normal.
Like any syndrome, fetal alcohol syndrome (FAS) is a group of signs and symptoms that appear together and indicate a certain condition. In the case of FAS, the signs and symptoms are birth defects that result from a woman's use of alcohol during her pregnancy.

To treat your tinnitus, your doctor will first try to identify any underlying, treatable condition that may be associated with your symptoms. If tinnitus is due to a health condition, your doctor may be able to take steps that could reduce the noise. Examples include: Earwax removal.
Odor is a topic that’s not only embarrassing to discuss for many, but it’s simply embarrassing to live with for anyone who may be experiencing it. Oftentimes, it’s the result of a vaginal yeast infection, but that’s not always the case — which is why it’s important to find the root cause. Having a healthy vagina is extremely important to overall health, healthy births and healthy marriages, and vaginal odor can be a signal that there might be a health issue at play. How this affects a woman’s self-esteem is another side effect, not to mention how it can affect her relationship with her significant other due to the impact it may have on their sex life. While there are many causes, most of the time it can be resolved through natural remedies. But where does this incredibly uncomfortable vaginal odor come from, and what is it in the first place? Vaginal odor is defined as any odor that originates from the vagina. It’s normal for your vagina to have a slight odor given it’s an opening to the interior of the body, but a strong vaginal smell, such as a fishy vaginal odor, could indicate a bigger problem and should be checked out with your physician.

White stretch marks are unsightly marks that are found along the thighs, abdomen and upper arms. These are marks that could be due to a recent weight loss, trauma or pregnancy. Stretch marks can affect your confidence if you wear revealing outfits and so you should do all you can to remove them.

Overweight does not necessarily equal unhealthy. There are actually plenty of overweight people who are in excellent health (1). Conversely, many normal weight people have the metabolic problems associated with obesity (2). That’s because the fat under the skin is actually not that big of a problem (at least not from a health standpoint, it’s more of a cosmetic problem). It’s the fat in the abdominal cavity, the belly fat, that causes the biggest issues (3). If you have a lot of excess fat around your waistline, even if you’re not very heavy, then you should take some steps to get rid of it. Belly fat is usually estimated by measuring the circumference around your waist. This can easily be done at home with a simple tape measure. Anything above 40 inches (102 cm) in men and 35 inches (88 cm) in women, is known as abdominal obesity. There are actually a few proven strategies that have been shown to target the fat in the belly area more than other areas of the body.
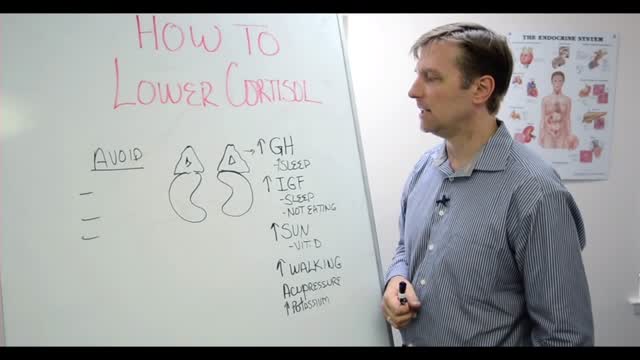
Assuming you haven't been diagnosed with Cushing's disease by your doctor, here are steps you can take to help lower high cortisol levels naturally: Switch to a Whole Foods, Anti-inflammatory Diet. Reduce and Manage Stress. Exercise Regularly. Use Adaptogen Herbs and Superfoods. Try Essential Oils to Promote Relaxation.
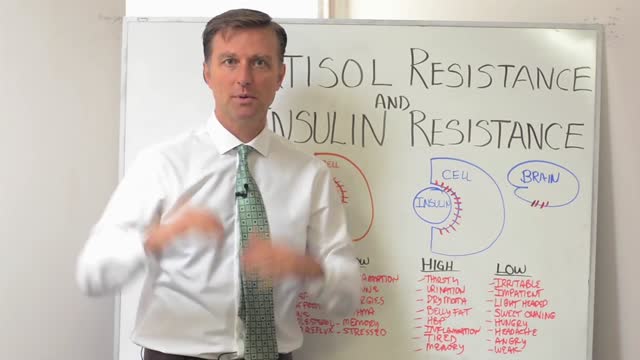
Insulin resistance — also called syndrome X or metabolic syndrome— is so pervasive today that we evaluate nearly every woman who visits our clinic to determine her level of risk. Most are taken aback when they learn they either already have insulin resistance syndrome (or as I call it pre-pre diabetic) or are well on their way to developing it. Experts estimate that 25% of all Americans suffer from insulin resistance. We believe the percentage is much higher among perimenopausal women. Because insulin is one of the “major” hormones, it’s also impossible for your body to balance its “minor” hormones (estrogen, progesterone and testosterone among them) until your insulin metabolism is balanced first. To put it simply, if you have hot flashes and you are insulin resistant, it’s going to be nearly impossible to cure the hot flashes without first healing the insulin resistance. Cortisol is also a “major” hormone – to understand it’s role in hormonal balance, read our related articles on adrenal fatigue. The good news is that you can heal insulin resistance. This has been a primary focus of our practice at Women to Women for over a decade, and our approach has been quite successful. Throughout the website you will find simple solutions on how to begin to heal this problematic syndrome.

New flu vaccines are released every year to keep up with rapidly adapting flu viruses. Because flu viruses evolve so quickly, last year's vaccine may not protect you from this year's viruses. After vaccination, your immune system produces antibodies that will protect you from the vaccine viruses.
How do you know if you have pneumonia? They may include: Cough. You will likely cough up mucus (sputum) from your lungs. ... Fever. Fast breathing and feeling short of breath. Shaking and "teeth-chattering" chills. Chest pain that often feels worse when you cough or breathe in. Fast heartbeat. Feeling very tired or very weak. Nausea and vomiting.
There are currently 2 types of pneumococcal vaccines: pneumococcal conjugate vaccine (PCV13 or Prevnar 13®) and pneumococcal polysaccharide vaccine (PPSV23 or Pneumovax®). PCV13 is recommended for all children younger than 5 years old, all adults 65 years or older, and people 6 years or older with certain risk factors.
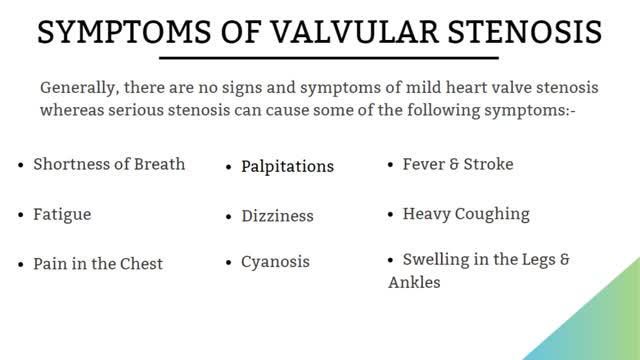
Valvular stenosis occurs when one or more heart valves are narrowed, stiffened, thickened or blocked. A variety of treatment options are available for this disorder. Learn more about the treatments on: bit.ly/2g6Mh8f
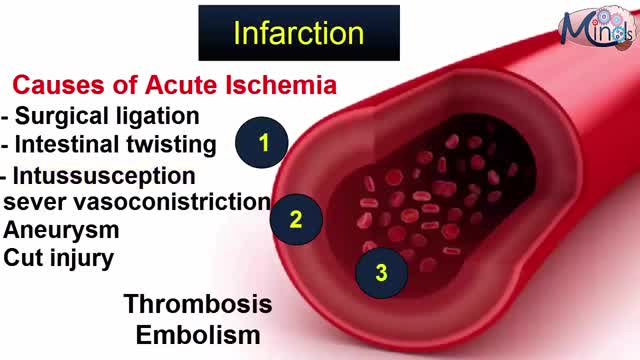
The occurrence and extent of cerebral infarction is determined by three basic factors: i) site of arterial occlusion, ii) the rapidity of arterial occlusion, and iii) the presence or absence of collateral circulation. Grossly, infarcts are usually divided into pale (non-hemorrhagic) and hemorrhagic types. Infarcts evolve over time, thus their gross appearance gives a clue to when they occurred. The temporal evolution of an infarct occurs in three stages: i) acute (1 day – 1 week) – the involved area is soft and edematous and there is a blurring of anatomic detail; ii) subacute (1 week – 1 month) – there is obvious tissue destruction and liquefactive necrosis of the involved brain; iii) chronic (>1 month) – the damaged tissue has been phagocytized and there is cavition with surrounding gliosis. Microscopically there is also a temporal evolution of cerebral infarcts. During the earliest phase of infarction (0-48 hours) chromatolysis and swollen eosinophilic neurons are seen. Neuronal cell necrosis and an acute inflammatory response are usually seen from 24-72 hours. This response is typically followed by an influx of mononuclear cells which begin to phagocytize necrotic debris (3-5 days). From 1-2 weeks after the infarct there is vascular proliferation and reactive astrocytosis. Over time (>1 month) the necrotic tissue will be completely removed and a cystic cavity surrounded by a glial scar will be formed.

What is the spleen and what causes an enlarged spleen (splenomegaly)? The spleen sits under your rib cage in the upper left part of your abdomen toward your back. It is an organ that is part of the lymph system and works as a drainage network that defends your body against infection. White blood cells produced in the spleen engulf bacteria, dead tissue, and foreign matter, removing them from the blood as blood passes through it. The spleen also maintains healthy red and white blood cells and platelets; platelets help your blood clot. The spleen filters blood, removing abnormal blood cells from the bloodstream. A spleen is normally about the size of your fist. A doctor usually can't feel it during an exam. But diseases can cause it to swell and become many times its normal size. Because the spleen is involved in many functions, many conditions may affect it.
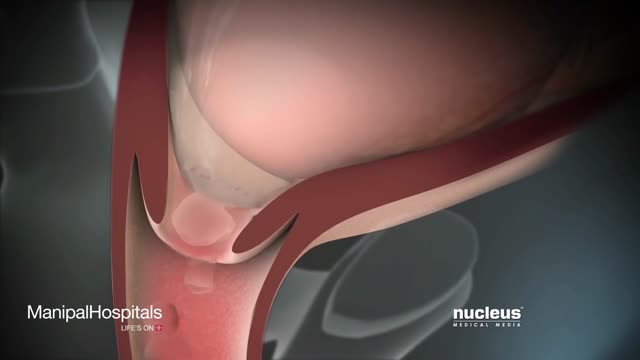
our uterus (or womb) is normally held in place inside your pelvis with various muscles, tissue, and ligaments. Because of pregnancy, childbirth or difficult labor and delivery, in some women these muscles weaken. Also, as a woman ages and with a natural loss of the hormone estrogen, her uterus can drop into the vaginal canal, causing the condition known as a prolapsed uterus.
During the examination, the doctor gently puts a lubricated, gloved finger of one hand into the rectum. He or she may use the other hand to press on the lower belly or pelvic area. A digital rectal exam is done for men as part of a complete physical examination to check the prostate gland .