Latest videos

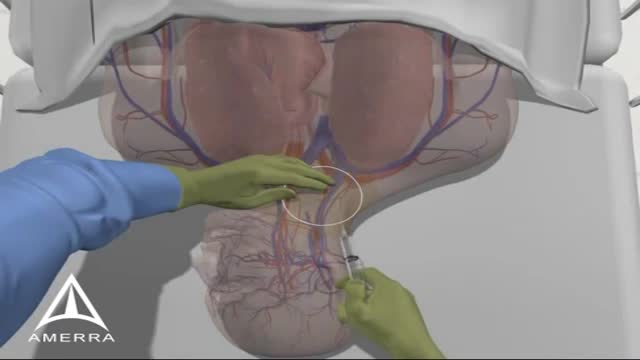
A central venous catheter (CVC), also known as a central line, central venous line, or central venous access catheter, is a catheter placed into a large vein. Catheters can be placed in veins in the neck (internal jugular vein), chest (subclavian vein or axillary vein), groin (femoral vein), or through veins in the arms (also known as a PICC line, or peripherally inserted central catheters). It is used to administer medication or fluids that are unable to be taken by mouth or would harm a smaller peripheral vein, obtain blood tests (specifically the "central venous oxygen saturation"), and measure central venous pressure.
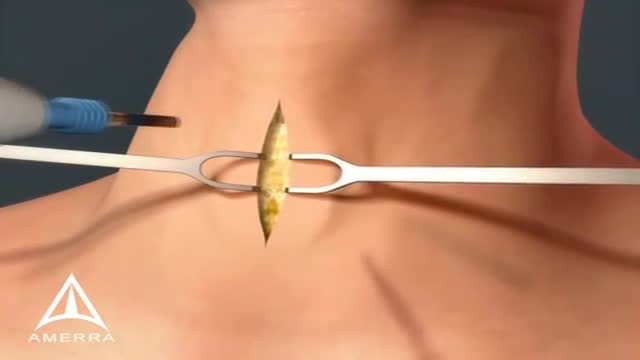
A tracheotomy or a tracheostomy: is simply an opening surgically created through the neck into the trachea (windpipe) to allow direct access to the breathing tube and is commonly done in an operating room under general anesthesia. A tube is usually placed through this opening to provide an airway and to remove secretions from the lungs. Breathing is done through the tracheostomy tube rather than through the nose and mouth. The term “tracheotomy” refers to the incision into the trachea (windpipe) that forms a temporary or permanent opening, which is called a “tracheostomy,” however; the terms are sometimes used interchangeably.

This minimally invasive surgical procedure repairs the valve without removing the old, damaged valve. Instead, it wedges a replacement valve into the aortic valve’s place. The surgery may be called a transcatheter aortic valve replacement (TAVR) or transcatheter aortic valve implantation (TAVI).

The human heart has four main valves—two on the left and two on the right. The aortic valve is one of the main valves on the left side of the heart. It is the outflow valve for the left ventricle, which means that it is the valve between the heart and the body. The aortic valve opens when the left ventricle squeezes to pump out blood, and closes in between heart beats to keep blood from going backward into the heart.

A torn meniscus is one of the most common knee injuries. Any activity that causes you to forcefully twist or rotate your knee, especially when putting your full weight on it, can lead to a torn meniscus. Each of your knees has two menisci — C-shaped pieces of cartilage that act like a cushion between your shinbone and your thighbone. A torn meniscus causes pain, swelling and stiffness. You also might feel a block to knee motion and have trouble extending your knee fully. Conservative treatment — such as rest, ice and medication — is sometimes enough to relieve the pain of a torn meniscus and give the injury time to heal on its own. In other cases, however, a torn meniscus requires surgical repair.

Cellulitis (sel-u-LIE-tis) is a common, potentially serious bacterial skin infection. Cellulitis appears as a swollen, red area of skin that feels hot and tender. It can spread rapidly to other parts of the body. Cellulitis isn't usually spread from person to person. Skin on lower legs is most commonly affected, though cellulitis can occur anywhere on your body or face. Cellulitis might affect only your skin's surface. Or it might also affect tissues underlying your skin and can spread to your lymph nodes and bloodstream. Left untreated, the spreading infection can rapidly turn life-threatening. It's important to seek immediate medical attention if cellulitis symptoms occur.
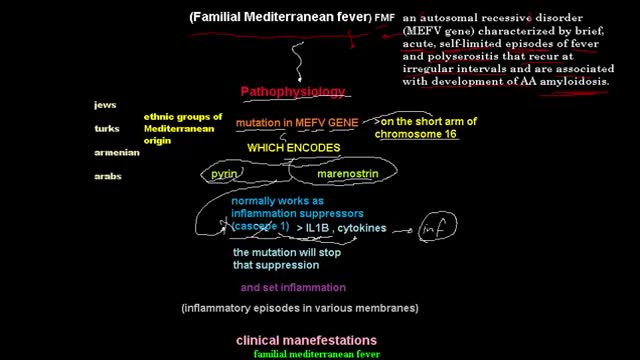
Familial Mediterranean fever is an inflammatory disorder that causes recurrent fevers and painful inflammation of your abdomen, lungs and joints. Familial Mediterranean fever is an inherited disorder that usually occurs in people of Mediterranean origin — including Sephardic Jews, Arabs, Greeks, Italians, Armenians and Turks. But it may affect any ethnic group. Familial Mediterranean fever is typically diagnosed during childhood. While there's no cure for this disorder, you may be able to relieve signs and symptoms of familial Mediterranean fever — or even prevent them altogether — by sticking to your treatment plan.

Rotationplasty is a type of autograft wherein a portion of a limb is removed, while the remaining limb below the involved portion is rotated and reattached. This procedure is used when a portion of an extremity is injured or involved with a disease, such as cancer. Typically, the ankle joint becomes the knee joint.
http://dissolve-kidney-stones-fast.info-pro.co/ No-one knows better than me the physical pain and heartache that’s caused by kidney stones. and for many years I was a fellow sufferer of this nasty affliction. I know that many of you are experiencing an attack right now. Let me tell you -I’ve been there lots of times myself. I know what it’s like: the shooting abdominal pain that can last for hours, the nausea, the burning sensation and the constant water infections. Even when you get some temporary relief, you can never really relax. You’re always looking over your shoulder, waiting for those tell tale signs which signify another kidney stone attack on the horizon. You want to just get on with your life. But you can’t. If you’re anything like I was, you’d do anything for a cure. I decided to utilise my research skills to get to the bottom of the problem. This led me on a mission to find a safe, natural and effective method of defeating kidney stones. The good news: I found it. You too can share in this discovery and rid yourself of kidney stones – the natural way. natural remedy brings instant relief finally a permanent cure for kidney stones. click here. http://dissolve-kidney-stones-fast.info-pro.co/
Influenza is a viral infection that attacks your respiratory system — your nose, throat and lungs. Influenza, commonly called the flu, is not the same as stomach "flu" viruses that cause diarrhea and vomiting. For most people, influenza resolves on its own. But sometimes, influenza and its complications can be deadly. People at higher risk of developing flu complications include: Young children under 5, and especially those under 2 years Adults older than 65 Residents of nursing homes and other long-term care facilities Pregnant women and women up to two weeks postpartum People with weakened immune systems People who have chronic illnesses, such as asthma, heart disease, kidney disease and diabetes People who are very obese, with a body mass index (BMI) of 40 or higher Your best defense against influenza is to receive an annual vaccination.

The examination room should be quiet, warm and well lit. After you have finished interviewing the patient, provide them with a gown (a.k.a. "Johnny") and leave the room (or draw a separating curtain) while they change. Instruct them to remove all of their clothing (except for briefs) and put on the gown so that the opening is in the rear. Occasionally, patient's will end up using them as ponchos, capes or in other creative ways. While this may make for a more attractive ensemble it will also, unfortunately, interfere with your ability to perform an examination! Prior to measuring vital signs, the patient should have had the opportunity to sit for approximately five minutes so that the values are not affected by the exertion required to walk to the exam room. All measurements are made while the patient is seated. Observation: Before diving in, take a minute or so to look at the patient in their entirety, making your observations, if possible, from an out-of-the way perch. Does the patient seem anxious, in pain, upset? What about their dress and hygiene? Remember, the exam begins as soon as you lay eyes on the patient. Temperature: This is generally obtained using an oral thermometer that provides a digital reading when the sensor is placed under the patient's tongue. As most exam rooms do not have thermometers, it is not necessary to repeat this measurement unless, of course, the recorded value seems discordant with the patient's clinical condition (e.g. they feel hot but reportedly have no fever or vice versa). Depending on the bias of a particular institution, temperature is measured in either Celcius or Farenheit, with a fever defined as greater than 38-38.5 C or 101-101.5 F. Rectal temperatures, which most closely reflect internal or core values, are approximately 1 degree F higher than those obtained orally. Respiratory Rate: Respirations are recorded as breaths per minute. They should be counted for at least 30 seconds as the total number of breaths in a 15 second period is rather small and any miscounting can result in rather large errors when multiplied by 4. Try to do this as surreptitiously as possible so that the patient does not consciously alter their rate of breathing. This can be done by observing the rise and fall of the patient's hospital gown while you appear to be taking their pulse. Normal is between 12 and 20. In general, this measurement offers no relevant information for the routine examination. However, particularly in the setting of cardio-pulmonary illness, it can be a very reliable marker of disease activity. Pulse: This can be measured at any place where there is a large artery (e.g. carotid, femoral, or simply by listening over the heart), though for the sake of convenience it is generally done by palpating the radial impulse. You may find it helpful to feel both radial arteries simultaneously, doubling the sensory input and helping to insure the accuracy of your measurements. Place the tips of your index and middle fingers just proximal to the patients wrist on the thumb side, orienting them so that they are both over the length of the vessel.
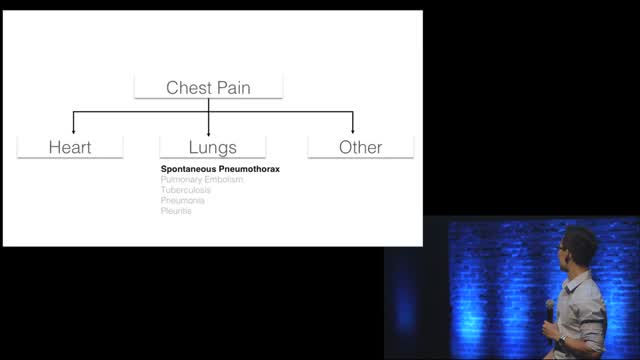
Chest pain is a frequent complaint of patients seeking urgent medical assistance, and accounts for an estimated 2-4 per cent of all A&E visits in the UK (Becker, 2000). Generally, acute chest pain should be considered cardiovascular in origin until proven otherwise and it is common in clinical practice to err on the conservative or ‘safe’ side when evaluating people with chest pain. Individuals with suspected ischaemic chest pain must be evaluated rapidly for several reasons: - Myocardial ischaemia, if prolonged and severe, can cause myocardial infarction (necrosis); - Treatment strategies that achieve myocardial salvage (thrombolytic therapy or primary coronary angioplasty) are available for patients with acute coronary syndromes and these treatments reduce morbidity and mortality;

More than 1 million Americans suffer a heart attack every year. Traditional symptoms—chest pain or pressure, cold sweat, extreme weakness—are well known. But there are more subtle signs you’re having or are about to have a heart attack that can be easy to miss. If you experience any of the following symptoms, see a doctor. Noticing heart attack signs early and getting prompt treatment can save your life.

Many women with hair loss suffer in silence, altering their hairstyle to hide thinning or patches. But the sooner you seek care, the better the chances of successfully treating it, says Mary Gail Mercurio, MD, associate professor of dermatology at the University of Rochester in Rochester, N.Y. It's not as uncommon as you may think: As many as 5% of women under 30 and 60% of those older than 70 are affected, she says. At the recent meeting of the American Academy of Dermatology in Miami Beach, Fla., Mercurio discussed common forms of hair loss in women and treatment options.

Anemia is a medical condition in which the red blood cell count or hemoglobin is less than normal. The normal level of hemoglobin is generally different in males and females. For men, a normal hemoglobin level is typically defined as a level of more than 13.5 gram/100 ml, and in women as hemoglobin of more than 12.0 gram/100 ml. These definitions may vary slightly depending on the source and the laboratory reference used. Continue Reading

Here are seven ways to start reining in your risks today, before a stroke has the chance to strike. Lower blood pressure. ... Lose weight. ... Exercise more. ... Drink — in moderation. ... Treat atrial fibrillation. ... Treat diabetes. ... Quit smoking.

Most frozen shoulders get better on their own within 12 to 18 months. For persistent symptoms, your doctor may suggest: Steroid injections. Injecting corticosteroids into your shoulder joint may help decrease pain and improve shoulder mobility, especially in the early stages of the process. Joint distension. Injecting sterile water into the joint capsule can help stretch the tissue and make it easier to move the joint. Shoulder manipulation. In this procedure, you receive a general anesthetic, so you'll be unconscious and feel no pain. Then the doctor moves your shoulder joint in different directions, to help loosen the tightened tissue. Surgery. Surgery for frozen shoulder is rare, but if nothing else has helped, your doctor may recommend surgery to remove scar tissue and adhesions from inside your shoulder joint. Doctors usually perform this surgery with lighted, tubular instruments inserted through small incisions around your joint (arthroscopically).