Latest videos
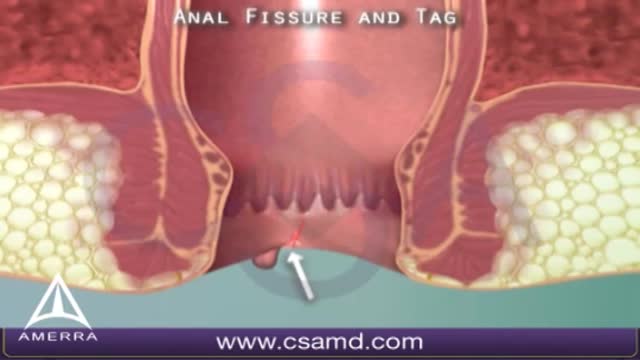
An anal fissure is a small tear in the thin, moist tissue (mucosa) that lines the anus. An anal fissure may occur when you pass hard or large stools during a bowel movement. Anal fissures typically cause pain and bleeding with bowel movements. You also may experience spasms in the ring of muscle at the end of your anus (anal sphincter). Anal fissures are very common in young infants but can affect people of any age. Most anal fissures get better with simple treatments, such as increased fiber intake or sitz baths. Some people with anal fissures may need medication or, occasionally, surgery.
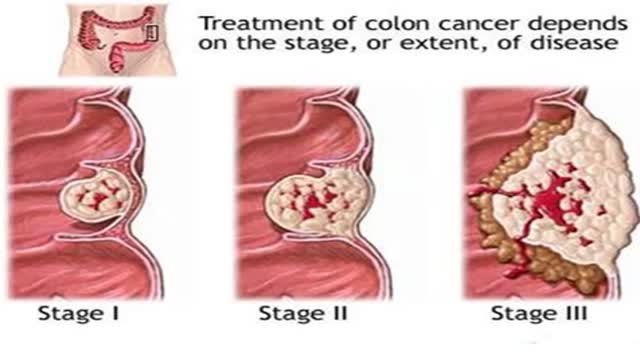
Signs and symptoms of colon cancer include: A change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool, that lasts longer than four weeks Rectal bleeding or blood in your stool Persistent abdominal discomfort, such as cramps, gas or pain A feeling that your bowel doesn't empty completely Weakness or fatigue Unexplained weight loss Many people with colon cancer experience no symptoms in the early stages of the disease. When symptoms appear, they'll likely vary, depending on the cancer's size and location in your large intestine.
Irritable bowel syndrome (IBS) is a common disorder that affects the large intestine (colon). Irritable bowel syndrome commonly causes cramping, abdominal pain, bloating, gas, diarrhea and constipation. IBS is a chronic condition that you will need to manage long term. Even though signs and symptoms are uncomfortable, IBS — unlike ulcerative colitis and Crohn's disease, which are forms of inflammatory bowel disease — doesn't cause changes in bowel tissue or increase your risk of colorectal cancer. Only a small number of people with irritable bowel syndrome have severe signs and symptoms. Some people can control their symptoms by managing diet, lifestyle and stress. Others will need medication and counseling.

Crohn's disease is an inflammatory bowel disease (IBD). It causes inflammation of the lining of your digestive tract, which can lead to abdominal pain, severe diarrhea, fatigue, weight loss and malnutrition. Inflammation caused by Crohn's disease can involve different areas of the digestive tract in different people. The inflammation caused by Crohn's disease often spreads deep into the layers of affected bowel tissue. Crohn's disease can be both painful and debilitating, and sometimes may lead to life-threatening complications. While there's no known cure for Crohn's disease, therapies can greatly reduce its signs and symptoms and even bring about long-term remission. With treatment, many people with Crohn's disease are able to function well.
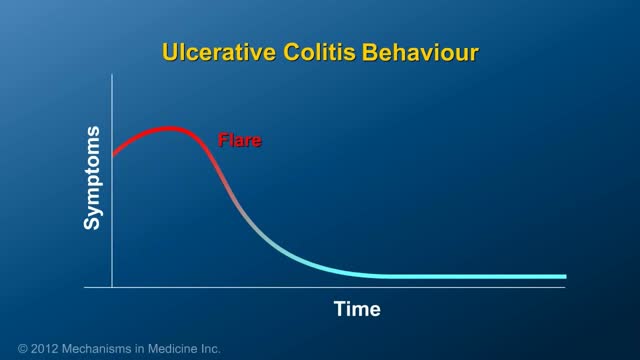
Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine (colon) and rectum. Symptoms usually develop over time, rather than suddenly. Ulcerative colitis can be debilitating and sometimes can lead to life-threatening complications. While it has no known cure, treatment can greatly reduce signs and symptoms of the disease and even bring about long-term remission.
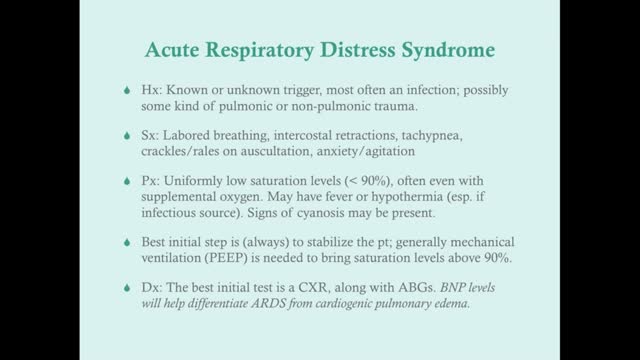
Acute respiratory distress syndrome (ARDS) occurs when fluid builds up in the tiny, elastic air sacs (alveoli) in your lungs. More fluid in your lungs means less oxygen can reach your bloodstream. This deprives your organs of the oxygen they need to function. ARDS typically occurs in people who are already critically ill or who have significant injuries. Severe shortness of breath — the main symptom of ARDS — usually develops within a few hours to a few days after the original disease or trauma. Many people who develop ARDS don't survive. The risk of death increases with age and severity of illness. Of the people who do survive ARDS, some recover completely while others experience lasting damage to their lungs.

Lyme disease is a bacterial infection primarily transmitted by Ixodes ticks, also known as deer ticks, and on the West Coast, black-legged ticks. These tiny arachnids are typically found in wooded and grassy areas. Although people may think of Lyme as an East Coast disease, it is found throughout the United States, as well as in more than sixty other countries. The Centers for Disease Control and Prevention estimate that 300,000 people are diagnosed with Lyme disease in the US every year. That’s 1.5 times the number of women diagnosed with breast cancer, and six times the number of people diagnosed with HIV/AIDS each year in the US. However, because diagnosing Lyme can be difficult, many people who actually have Lyme may be misdiagnosed with other conditions. Many experts believe the true number of cases is much higher. Lyme disease affects people of all ages. The CDC notes that it is most common in children, older adults, and others such as firefighters and park rangers who spend time in outdoor activities and have higher exposure to ticks. LymeDisease.org has developed a Lyme disease symptom checklist to help you document your exposure to Lyme disease and common symptoms for your healthcare provider. You will receive a report that you can print out and take with you to your next doctor’s appointment.

Rickets is the softening and weakening of bones in children, usually because of an extreme and prolonged vitamin D deficiency. Vitamin D promotes the absorption of calcium and phosphorus from the gastrointestinal tract. A deficiency of vitamin D makes it difficult to maintain proper calcium and phosphorus levels in bones, which can cause rickets. Adding vitamin D or calcium to the diet generally corrects the bone problems associated with rickets. When rickets are due to another underlying medical problem, your child may need additional medications or other treatment. Some skeletal deformities caused by rickets may require corrective surgery.
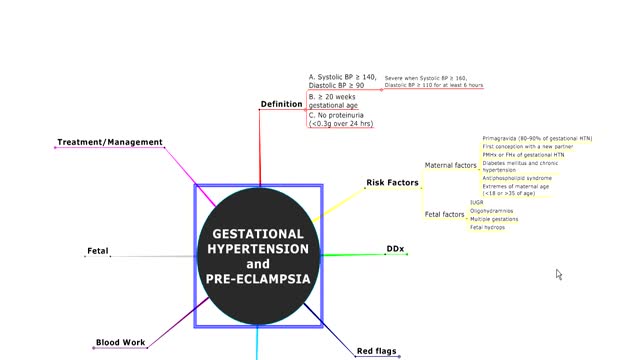
Gestational hypertension, also referred to as pregnancy induced hypertension (PIH) is a condition characterized by high blood pressure during pregnancy. Gestational hypertension can lead to a serious condition called preeclampsia, also referred to as toxemia. Hypertension during pregnancy affects about 6-8% of pregnant women.

Gestational diabetes develops during pregnancy (gestation). Like other types of diabetes, gestational diabetes affects how your cells use sugar (glucose). Gestational diabetes causes high blood sugar that can affect your pregnancy and your baby's health. Any pregnancy complication is concerning, but there's good news. Expectant moms can help control gestational diabetes by eating healthy foods, exercising and, if necessary, taking medication. Controlling blood sugar can prevent a difficult birth and keep you and your baby healthy. In gestational diabetes, blood sugar usually returns to normal soon after delivery. But if you've had gestational diabetes, you're at risk for type 2 diabetes. You'll continue working with your health care team to monitor and manage your blood sugar.

The Ortolani method is an examination method that identifies a dislocated hip that can be reduced into the socket (acetabulum). Ortolani described the feeling of reduction as a “Hip Click” but the translation from Italian was interpreted a sound instead of a sensation of the hip moving over the edge of the socket when it re-located. After the age of six weeks, this sensation is rarely detectable and should not be confused with snapping that is common and can occur in stable hips when ligaments in and around the hip create clicking noises. When the Ortolani test is positive because the hip is dislocated, treatment is recommended to keep the hip in the socket until stability has been established
Symptoms of liver failure include vomiting, diarrhea and fatigue as well as the symptoms from stage 3. While the progression from cirrhosis to failure can take years, the damage is irreversible and leads to eventual death. The key to treating liver disease is to diagnose the condition as early as possible.
Chronic kidney disease includes conditions that damage your kidneys and decrease their ability to keep you healthy by doing the jobs listed. If kidney disease gets worse, wastes can build to high levels in your blood and make you feel sick. You may develop complications like high blood pressure, anemia (low blood count), weak bones, poor nutritional health and nerve damage. Also, kidney disease increases your risk of having heart and blood vessel disease. These problems may happen slowly over a long period of time. Chronic kidney disease may be caused by diabetes, high blood pressure and other disorders. Early detection and treatment can often keep chronic kidney disease from getting worse. When kidney disease progresses, it may eventually lead to kidney failure, which requires dialysis or a kidney transplant to maintain life.

Finding a donor heart can be difficult. The heart must be donated by someone who is brain-dead but is still on life support. The donor heart must be matched as closely as possible to your tissue type to reduce the chance that your body will reject it. You are put into a deep sleep with general anesthesia, and a cut is made through the breastbone. Your blood flows through a heart-lung bypass machine while the surgeon works on your heart. This machine does the work of your heart and lungs while they are stopped, and supplies your body with blood and oxygen. Your diseased heart is removed and the donor heart is stitched in place. The heart-lung machine is then disconnected. Blood flows through the transplanted heart, which takes over supplying your body with blood and oxygen. Tubes are inserted to drain air, fluid, and blood out of the chest for several days, and to allow the lungs to fully re-expand.
An abdominal aortic aneurysm is an enlarged area in the lower part of the aorta, the major blood vessel that supplies blood to the body. The aorta, about the thickness of a garden hose, runs from your heart through the center of your chest and abdomen. Because the aorta is the body's main supplier of blood, a ruptured abdominal aortic aneurysm can cause life-threatening bleeding. Depending on the size and the rate at which your abdominal aortic aneurysm is growing, treatment may vary from watchful waiting to emergency surgery. Once an abdominal aortic aneurysm is found, doctors will closely monitor it so that surgery can be planned if it's necessary. Emergency surgery for a ruptured abdominal aortic aneurysm can be risky.

Mitral valve surgery is surgery to either repair or replace the mitral valve in your heart. Blood flows from the lungs and enters a pumping chamber of the heart called the left atrium. The blood then flows into the final pumping chamber of the heart called the left ventricle. The mitral valve is located between these two chambers. It makes sure that the blood keeps moving forward through the heart. You may need surgery on your mitral valve if: The mitral valve is hardened (calcified). This prevents blood from moving forward through the valve. The mitral valve is too loose. Blood tends to flows backward when this occurs. Minimally invasive mitral valve surgery is done through several small cuts. Another type of operation, open mitral valve surgery requires a larger cut.