Latest videos

Blunt injury to the heart ranges from contusion to disruption. This report comprises 14 patients seen during a 6-year period with cardiac rupture secondary to blunt trauma. Eight patients were injured in automobile accidents, two patients were injured in auto-pedestrian accidents, two were kicked in the chest by ungulates, and two sustained falls. Cardiac tamponade was suspected in ten patients. Five patients presented with prehospital cardiac arrest or arrested shortly after arrival. All underwent emergency department thoracotomy without survival. Two patients expired in the operating room during attempted cardiac repair; both had significant extracardiac injury. Seven patients survived, three had right atrial injuries, three had right ventricular injuries, and one had a left atrial injury. Cardiopulmonary bypass was not required for repair of the surviving patients. There were no significant complications from the cardiac repair.
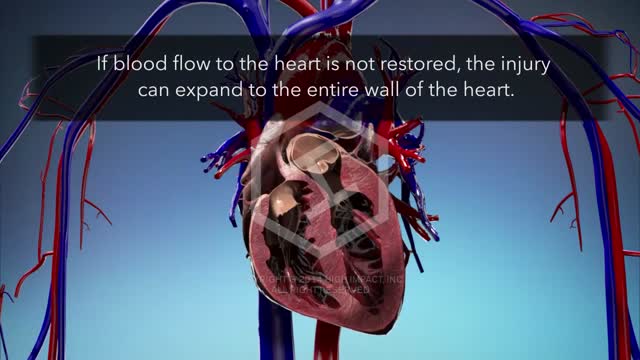
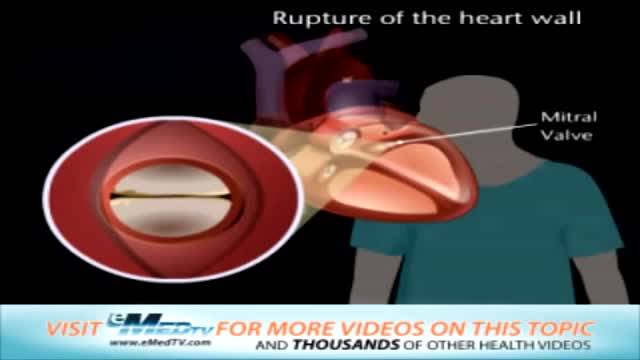
Myocardial rupture occurs in the setting of acute myocardial infarction (AMI), blunt and penetrating cardiac trauma, primary cardiac infection, primary and secondary cardiac tumors, infiltrative diseases of the heart, and aortic dissection. Myocardial rupture (or perforation) may also occur iatrogenically during percutaneous cardiac procedures (including device implantation) or open heart surgery (particularly valve replacement). Recently, myocardial rupture has been reported in the setting of stress cardiomyopathy (Takotsubo or regional ventricular ballooning syndrome). The clinical presentation of myocardial rupture depends on the mechanism and site of injury and the hemodynamic effects of the rupture. Mortality is extremely high unless early diagnosis is made and urgent surgical intervention is provided.

An abscess is a tender mass generally surrounded by a colored area from pink to deep red. Abscesses are often easy to feel by touching. The middle of an abscess is full of pus and debris. Painful and warm to touch, abscesses can show up any place on your body. The most common sites are in your armpits (axillae), areas around your anus and vagina(Bartholin gland abscess), the base of your spine (pilonidal abscess), around a tooth (dental abscess), and in your groin. Inflammation around a hair follicle can also lead to the formation of an abscess, which is called a boil (furuncle). Unlike other infections, antibiotics alone will not usually cure an abscess. In general an abscess must open and drain in order for it to improve. Sometimes draining occurs on its own, but generally it must be opened by a doctor in a procedure called incision and drainage (I&D).

BACKGROUND: Clubfoot occurs in approximately one in 1000 live births and is one of the most common congenital birth defects. Although there have been several reports of successful treatment of idiopathic clubfoot with the Ponseti method, the use of this method for the treatment of other forms of clubfoot has not been reported. The purpose of the present study was to evaluate the early results of the Ponseti method when used for the treatment of clubfoot associated with distal arthrogryposis. METHODS: Twelve consecutive infants (twenty-four feet) with clubfoot deformity associated with distal arthrogryposis were managed with the Ponseti method and were retrospectively reviewed at a minimum of two years. The severity of the foot deformity was classified according to the grading system of Diméglio et al. The number of casts required to achieve correction was compared with published data for the treatment of idiopathic clubfoot. Recurrent clubfoot deformities or complications during treatment were recorded. RESULTS: Twenty-two clubfeet in eleven patients were classified as Diméglio grade IV, and two clubfeet in one patient were classified as Diméglio grade II. Initial correction was achieved in all clubfeet with a mean of 6.9 +/- 2.1 casts (95% confidence interval, 5.6 to 8.3 casts), which was significantly greater than the mean of 4.5 +/- 1.2 casts (95% confidence interval, 4.3 to 4.7 casts) needed in a cohort of 219 idiopathic clubfeet that were treated during the same time period by the senior author with use of the Ponseti method (p = 0.002). Six feet in three patients had a relapse after initial successful treatment. All relapses were related to noncompliance with prescribed brace wear. Four relapsed clubfeet in two patients were successfully treated with repeat casting and/or tenotomy; the remaining two relapsed clubfeet in one patient were treated with extensive soft-tissue-release operations.
There are two types of surgery to repair a ruptured Achilles tendon : In open surgery, the surgeon makes a single large incision in the back of the leg. In percutaneous surgery, the surgeon makes several small incisions rather than one large incision.
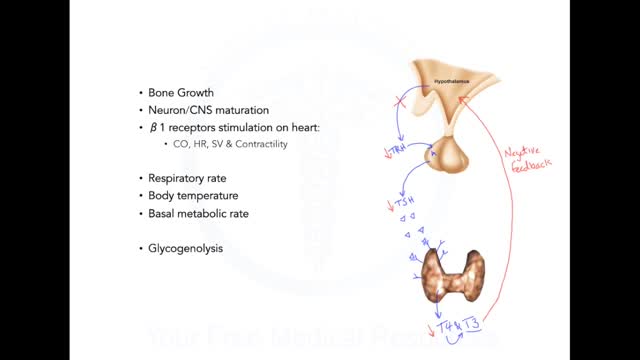
Graves' disease is an immune system disorder that results in the overproduction of thyroid hormones (hyperthyroidism). Although a number of disorders may result in hyperthyroidism, Graves' disease is a common cause. Because thyroid hormones affect a number of different body systems, signs and symptoms associated with Graves' disease can be wide ranging and significantly influence your overall well-being. Although Graves' disease may affect anyone, it's more common among women and before the age of 40. The primary treatment goals are to inhibit the overproduction of thyroid hormones and lessen the severity of symptoms.
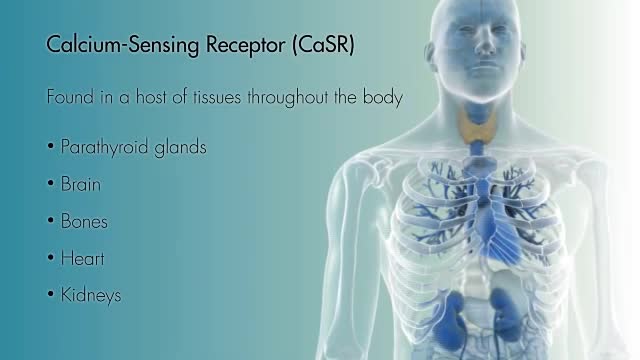
Hypoparathyroidism is an uncommon condition in which your body secretes abnormally low levels of parathyroid hormone (PTH). PTH plays a key role in regulating and maintaining a balance of your body's levels of two minerals — calcium and phosphorus. The low production of PTH in hypoparathyroidism leads to abnormally low ionized calcium levels in your blood and bones and to an increase of serum phosphorus. Treatment for hypoparathyroidism consists of taking supplements to normalize your calcium and phosphorus levels. Depending on the cause of your hypoparathyroidism, you'll likely need to take supplements for life.

Hyperparathyroidism is an excess of parathyroid hormone in the bloodstream due to overactivity of one or more of the body's four parathyroid glands. These glands are about the size of a grain of rice and are located in your neck. The parathyroid glands produce parathyroid hormone, which helps maintain an appropriate balance of calcium in the bloodstream and in tissues that depend on calcium for proper functioning. Two types of hyperparathyroidism exist. In primary hyperparathyroidism, an enlargement of one or more of the parathyroid glands causes overproduction of the hormone, resulting in high levels of calcium in the blood (hypercalcemia), which can cause a variety of health problems. Surgery is the most common treatment for primary hyperparathyroidism. Secondary hyperparathyroidism occurs as a result of another disease that initially causes low levels of calcium in the body and over time, increased parathyroid hormone levels occur.
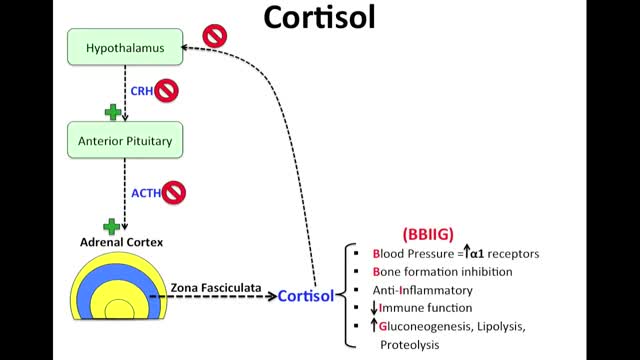
Cushing syndrome occurs when your body is exposed to high levels of the hormone cortisol for a long time. Cushing syndrome, sometimes called hypercortisolism, may be caused by the use of oral corticosteroid medication. The condition can also occur when your body makes too much cortisol on its own. Too much cortisol can produce some of the hallmark signs of Cushing syndrome — a fatty hump between your shoulders, a rounded face, and pink or purple stretch marks on your skin. Cushing syndrome can also result in high blood pressure, bone loss and, on occasion, type 2 diabetes. Treatments for Cushing syndrome can return your body's cortisol production to normal and noticeably improve your symptoms. The earlier treatment begins, the better your chances for recovery.
Addison's disease is a disorder that occurs when your body produces insufficient amounts of certain hormones produced by your adrenal glands. In Addison's disease, your adrenal glands produce too little cortisol and often insufficient levels of aldosterone as well. Also called adrenal insufficiency, Addison's disease occurs in all age groups and affects both sexes. Addison's disease can be life-threatening. Treatment for Addison's disease involves taking hormones to replace the insufficient amounts being made by your adrenal glands, in order to mimic the beneficial effects produced by your naturally made hormones.
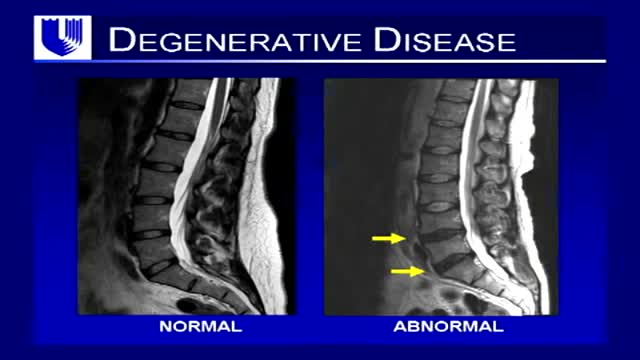
Neck pain is a common complaint. Neck muscles can be strained from poor posture — whether it's leaning over your computer or hunching over your workbench. Osteoarthritis also is a common cause of neck pain. Rarely, neck pain can be a symptom of a more serious problem. Seek medical care if your neck pain is accompanied by numbness or loss of strength in your arms or hands or if you have shooting pain into your shoulder or down your arm