Latest videos

Preventing Sexually Transmitted Diseases A sexually transmitted disease (STD) is an infection that is spread during sexual contact with another person. This includes touching, since some STDs can be spread from skin-to-skin contact. In general, STDs are highly preventable. Almost 20 million new STDs are diagnosed each year in the United States, according to the Centers for Disease Control and Prevention (CDC). However, a large number of those infections could be avoided if people made different decisions about their sexual health. The only guaranteed method to prevent STDs is to abstain from all sexual contact. This may not a practical solution for everyone. Fortunately, there are steps people can take to limit their risk of exposure.
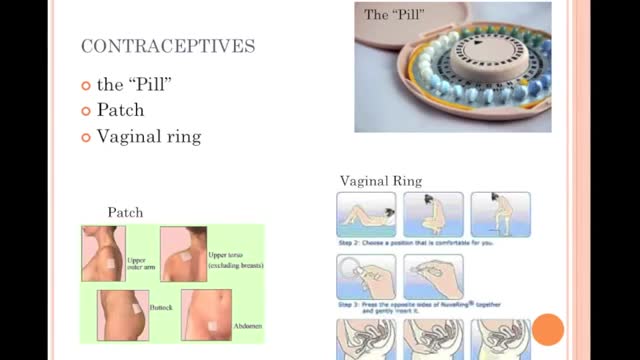
Choosing not to have sex provides 100 percent protection from HIV, STIs, and pregnancy. For some, this means avoiding vaginal, anal, and oral-genital intercourse altogether. Others may choose to avoid any type of sexual or intimate contact, including hugging and kissing. Choosing not to have sex is often referred to as “abstinence.” WHAT ARE THE ADVANTAGES OF CHOOSING NOT TO HAVE SEX (ABSTINENCE)? Choosing not to have sex is free and available to all. Not having sex is extremely effective at preventing both infection and pregnancy. It is the only 100% effective method of preventing sexually transmitted infections (STIs) and unintended pregnancy. Not having sex can be practiced at any time in one's life. Not having sex may encourage people to build relationships in other ways. Not having sex may be the course of action which you feel is right for you and makes you feel good about yourself.

Looking for a week-by-week guide to pregnancy? You're in luck! We've got loads of expert-approved info about each week and trimester, including what's up with your growing baby and what changes to expect for yourself. You'll find stunning fetal development videos, thousands of articles, and helpful tools like our Due Date Calculator and Baby Names Finder. Meet other parents-to-be in our online community, and get all of this and more in our free pregnancy app. Dive in, and congratulations!

Polycystic ovary syndrome (PCOS) is a common endocrine system disorder among women of reproductive age. Women with PCOS may have enlarged ovaries that contain small collections of fluid — called follicles — located in each ovary as seen during an ultrasound exam. Infrequent or prolonged menstrual periods, excess hair growth, acne, and obesity can all occur in women with polycystic ovary syndrome. In adolescents, infrequent or absent menstruation may raise suspicion for the condition. The exact cause of polycystic ovary syndrome is unknown. Early diagnosis and treatment along with weight loss may reduce the risk of long-term complications, such as type 2 diabetes and heart disease.
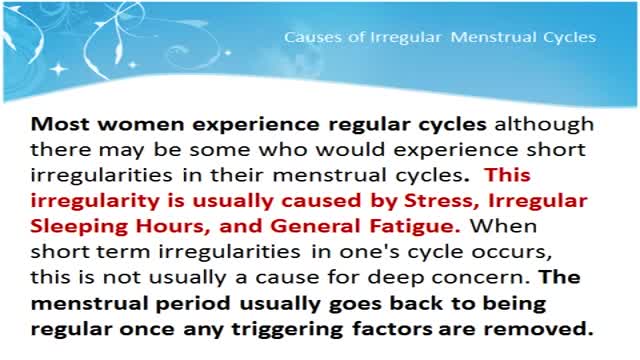
Menstruation is the time of month when the womb (uterus) sheds its lining and vaginal bleeding occurs. This is known as a menstrual period. Periods vary widely from woman to woman. Some periods are punctual, some are unpredictable. On average, a woman gets her period every 24 to 38 days. A period usually lasts about two to eight days. Irregular periods may require treatment. What Are Irregular Periods? You may have irregular periods if: The time between each period starts to change. You are losing more or less blood during a period than usual. The number of days that your period lasts varies significantly. There are different terms for different types of irregular periods: Irregular Menstrual Bleeding (IrregMB): Bleeding of more than 20 days in individual cycle lengths over a period of one year. Absent Menstrual Bleeding (amenorrhea): No bleeding in a 90-day period. Heavy Menstrual Bleeding (HMB): Excessive menstrual blood loss that interferes with the woman’s physical, emotional, social, and material quality of life and can occur alone or in combination with other symptoms. Heavy and Prolonged Menstrual Bleeding (HPMB): Less common than HMB. It is important to make a distinction from HMB given they may have different etiologies and respond to different therapies. Light Menstrual Bleeding: Based on patient complaint, rarely related to pathology.

To relieve mild menstrual cramps: Take aspirin or another pain reliever, such as Tylenol (acetaminophen), Motrin (ibuprofen) or Aleve (naproxen). (Note: For best relief, you must take these medications as soon as bleeding or cramping starts.) Place a heating pad or hot water bottle on your lower back or abdomen

Pulmonary fibrosis is a lung disease that occurs when lung tissue becomes damaged and scarred. This thickened, stiff tissue makes it more difficult for your lungs to work properly. As pulmonary fibrosis worsens, you become progressively more short of breath. The scarring associated with pulmonary fibrosis can be caused by a multitude of factors. But in most cases, doctors can't pinpoint what's causing the problem. When a cause can't be found, the condition is termed idiopathic pulmonary fibrosis. The lung damage caused by pulmonary fibrosis can't be repaired, but medications and therapies can sometimes help ease symptoms and improve quality of life. For some people, a lung transplant might be appropriate.
A traumatic brain injury (TBI) is defined as a blow or jolt to the head, or a penetrating head injury that disrupts the normal function of the brain. TBI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue. Symptoms of a TBI can be mild, moderate or severe, depending on the extent of damage to the brain. Mild cases (mild traumatic brain injury, or mTBI) may result in a brief change in mental state or consciousness, while severe cases may result in extended periods of unconsciousness, coma or even death. The 4th International Conference on Concussion in Sport held in Zurich, Switzerland in 2012 defined concussion, a subset of mTBI, as the following: Concussion is the historical term representing low velocity injuries that cause brain ‘shaking’ resulting in clinical symptoms and that are not necessarily related to a pathological injury. Concussion is a subset of TBI and will be the term used in this document. It was also noted that the term commotio cerebri is often used in European and other countries. Minor revisions were made to the definition of concussion, which is defined as follows: Concussion is a brain injury and is defined as a complex pathophysiological process affecting the brain, induced by biomechanical forces. Several common features that incorporate clinical, pathologic and biomechanical injury constructs that may be utilised in defining the nature of a concussive head injury include: 1. Concussion may be caused either by a direct blow to the head, face, neck or elsewhere on the body with an "impulsive" force transmitted to the head. 2. Concussion typically results in the rapid onset of short-lived impairment of neurological function that resolves spontaneously. However, in some cases, symptoms and signs may evolve over a number of minutes to hours. 3. Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury and, as such, no abnormality is seen on standard structural neuroimaging studies. 4. Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. However, it is important to note that in some cases symptoms may be prolonged. To view peer reviewed literature related to sports concussions, the Sports Concussion Library can be found here. Incidence The U.S. Consumer Product Safety Commission (CPSC) tracks product-related injuries through its National Electronic Injury Surveillance System (NEISS). According to CPSC data, there were an estimated 446,788 sports-related head injuries treated at U.S. hospital emergency rooms in 2009. This number represents an increase of nearly 95,000 sports-related injuries from the prior year. All of the 20 sports noted below posted increases in the number of injuries treated in 2009, except for trampolines, which posted 52 fewer injuries in 2009. Sports that exhibited substantial increases from 2008 to 2009 included water sports (11,239 to 28,716*), cycling (70,802 to 85,389), baseball and softball (26,964 to 38,394) and basketball (27,583 to 34,692). *Four categories were tabulated by the AANS in the current analysis that were not reflected in the 2008 injury data analysis, but together, these account for only 1,397 injuries. The actual incidence of head injuries may potentially be much higher for two primary reasons. 1). In the 2009 report, the CPSC excluded estimates for product categories that yielded 1,200 injuries or less, those that had very small sample counts and those that were limited to a small geographic area of the country; 2). Many less severe head injuries are treated at physician's offices or immediate care centers, or are self-treated. Included in these statistics are not only the sports/recreational activities, but the equipment and apparel used in these activities. For example, swimming-related injuries include the activity as well as diving boards, equipment, flotation devices, pools and water slides. The following 20 sports/recreational activities represent the categories contributing to the highest number of estimated head injuries treated in U.S. hospital emergency rooms in 2009.
Aortic valve replacement is a procedure in which a patient's failing aortic valve is replaced with an artificial heart valve. The aortic valve can be affected by a range of diseases; the valve can either become leaky (aortic insufficiency / regurgitation) or partially blocked (aortic stenosis).

Septic arthritis is also known as infectious arthritis, and is usually caused by bacteria, or fungus. The condition is an inflammation of a joint that's caused by infection. Typically, septic arthritis affects one large joint in the body, such as the knee or hip. Less frequently, septic arthritis can affect multiple joints
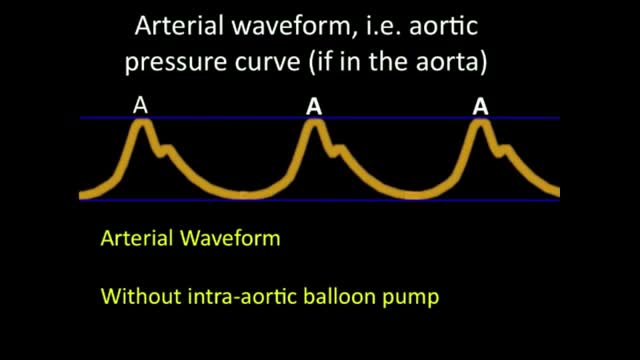
An intra-aortic balloon pump (IABP) is a mechanical device that helps the heart pump blood. This device is inserted into the aorta, the body's largest artery. It is a long, thin tube called a catheter with a balloon on the end of it. If you are hospitalized, your doctor may insert an IABP. Your doctor will numb an area of your leg and thread the IABP through the femoral artery in your leg into your aorta. He or she then positions the IABP at the center of your aorta, below your heart. The doctor will use an X-ray machine during this procedure to help accurately position the IABP. Why is it used? An IABP might be used to stabilize a person who is in the hospital for acute mitral valve regurgitation or severe heart failure. An IABP is only used for a short period of time (hours to days). A long-term treatment will likely be needed, such as valve surgery or the insertion of a left ventricular assist device (LVAD).
Atrial flutter is a type of abnormal heart rate, or arrhythmia. It occurs when the upper chambers of your heart beat too fast. When the chambers in the top of your heart (atria) beat faster than the bottom ones (ventricles), it complicates your heart rhythm
Atrial flutter (AFL) is a type of abnormal heart rate, or arrhythmia. It occurs when the upper chambers of your heart beat too fast. When the chambers in the top of your heart (atria) beat faster than the bottom ones (ventricles), it complicates your heart rhythm
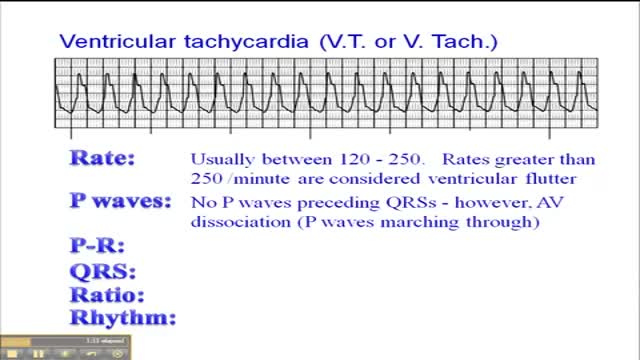
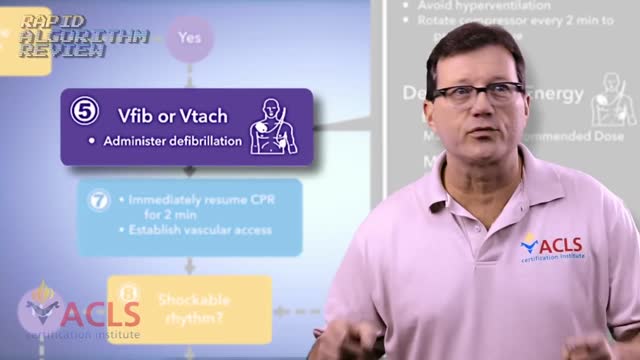
Ventricular tachycardia is a type of heart rhythm disorder (arrhythmia) in which the lower chambers of your heart (ventricles) beat very quickly because of a problem in your heart's electrical system. In ventricular tachycardia, your heart may not be able to pump enough blood to your body and lungs because the chambers are beating so fast that they don't have time to properly fill. Ventricular tachycardia may be brief — lasting for just seconds and often not causing symptoms — or it can last for much longer, and you can develop symptoms such as dizziness or lightheadedness, or you can even pass out. This condition usually occurs in people with other heart conditions, such as coronary artery disease, cardiomyopathy and some types of valvular heart disease. Ventricular tachycardia may lead to a condition in which your lower heart chambers quiver (ventricular fibrillation), which may cause your heart to stop (sudden cardiac arrest) and lead to death if not treated immediately. Ventricular tachycardia can also cause your heart to stop, especially if the heart is beating very quickly, if it's lasting for a long period, and if you have an underlying heart condition.

Ventricular fibrillation is a heart rhythm problem that occurs when the heart beats with rapid, erratic electrical impulses. This causes pumping chambers in your heart (the ventricles) to quiver uselessly, instead of pumping blood. Sometimes triggered by a heart attack, ventricular fibrillation causes your blood pressure to plummet, cutting off blood supply to your vital organs. Ventricular fibrillation, an emergency that requires immediate medical attention, causes the person to collapse within seconds. It's the most frequent cause of sudden cardiac death. Emergency treatment includes cardiopulmonary resuscitation (CPR) and shocks to the heart with a device called a defibrillator. Treatments for those at risk of ventricular fibrillation include medications and implantable devices that can restore a normal heart rhythm.
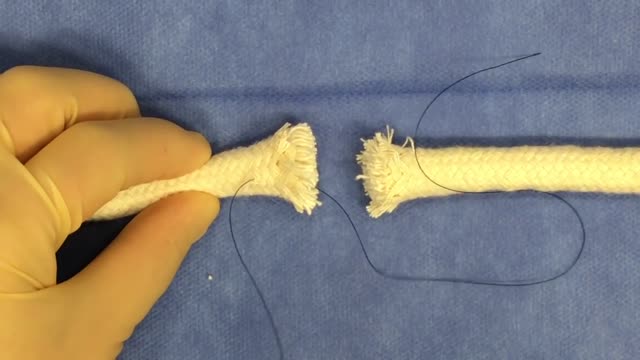
Tendon repair can be performed using: Local anesthesia (the immediate area of the surgery is pain-free) Regional anesthesia (the local and surrounding areas are pain-free) General anesthesia (the patient is asleep and pain-free) The surgeon makes a cut on the skin over the injured tendon. The damaged or torn ends of the tendon are sewn together. If the tendon has been severely injured, a tendon graft may be needed. In this case, a piece of tendon from the foot, toe, or another part of the body is often used. If needed, tendons are reattached to the surrounding tissue. The surgeon examines the area to see if there are any injuries to nerves and blood vessels. When the repair is complete, the wound is closed. If the tendon damage is too severe, the repair and reconstruction may have to be done at different times. The surgeon will perform one surgery to repair part of the injury, and then allow the hand to heal for a few weeks. Another surgery will be done later to complete the reconstruction and repair the tendon.

How Does a Bone Heal? All broken bones go through the same healing process. This is true whether a bone has been cut as part of a surgical procedure or fractured through an injury. The bone healing process has three overlapping stages: inflammation, bone production and bone remodeling. Inflammation starts immediately after the bone is fractured and lasts for several days. When the bone is fractured, there is bleeding into the area, leading to inflammation and clotting of blood at the fracture site. This provides the initial structural stability and framework for producing new bone. Diagram of inflammation in a fractured bone Bone production begins when the clotted blood formed by inflammation is replaced with fibrous tissue and cartilage (known as soft callus). As healing progresses, the soft callus is replaced with hard bone (known as hard callus), which is visible on x-rays several weeks after the fracture. Bone remodeling, the final phase of bone healing, goes on for several months. In remodeling, bone continues to form and becomes compact, returning to its original shape. In addition, blood circulation in the area improves. Once adequate bone healing has occurred, weightbearing (such as standing or walking) encourages bone remodeling.