Latest videos

A Pap smear (Papanicolau smear; also known as the Pap test) is a screening test for cervical cancer. The test itself involves collection of a sample of cells from a woman's cervix (the end of the uterus that extends into the vagina) during a routine pelvic exam

Genital warts are soft growths that appear on the genitals. Genital warts are a sexually transmitted infection (STI) caused by certain strains of the human papillomavirus (HPV). These skin growths can cause pain, discomfort, and itching. They are especially dangerous for women because some types of HPV can also cause cancer of the cervix and vulva.
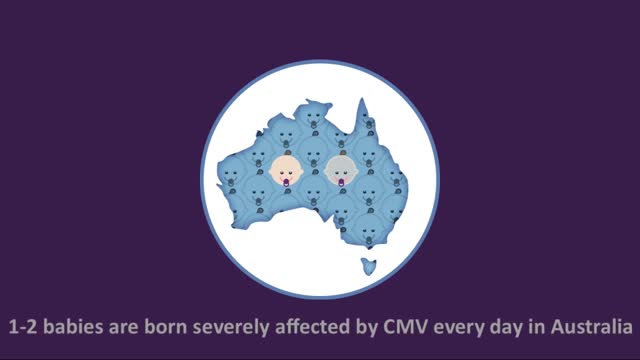
Cytomegalovirus (CMV) is a common virus that can infect almost anyone. Most people don't know they have CMV because it rarely causes symptoms. However, if you're pregnant or have a weakened immune system, CMV is cause for concern. Once infected with CMV, your body retains the virus for life. However, CMV usually remains dormant if you're healthy. CMV spreads from person to person through body fluids, such as blood, saliva, urine, semen and breast milk. CMV spread through breast milk usually doesn't make the baby sick. However, if you are pregnant and develop an active infection, you can pass the virus to your baby.
The virus was first discovered in 1964 when Sir Michael Anthony Epstein and Ms. Yvonne Barr found it in a Burkitt lymphoma cell line. In 1968, the virus was linked to the disease infectious mononucleosis. Infection with Epstein-Barr virus (EBV) is common and usually occurs in childhood or early adulthood. EBV is the cause of infectious mononucleosis (also termed "mono"), an illness associated with fever, sore throat, swollen lymph nodes in the neck, and sometimes an enlarged spleen. It is also known as human herpes virus 4. Although EBV can cause mononucleosis, not everyone infected with the virus will get mononucleosis. Less commonly, EBV can cause more serious disease. Symptoms caused by EBV are usually mild and self-limited, but the virus persists in the body for life. It can be reactivated quietly without causing symptoms and may contaminate saliva. Thus, otherwise healthy people can spread the virus to uninfected people through kissing or sharing
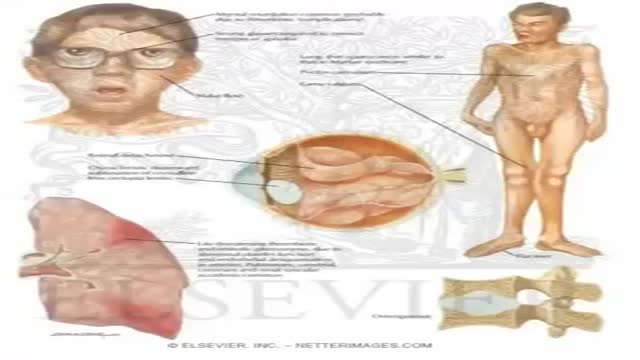
Homocystinuria is an inherited disorder that affects the metabolism of the amino acid methionine. Amino acids are the building blocks of life. Causes Homocystinuria is inherited in families as an autosomal recessive trait. This means that the child must inherit a non-working copy of the gene from each parent to be seriously affected. Homocystinuria has several features in common with Marfan syndrome, including joint and eye changes. Symptoms Newborn infants appear healthy. Early symptoms, if present, are not obvious. Symptoms may occur as mildly delayed development or failure to thrive. Increasing visual problems may lead to diagnosis of this condition. Other symptoms include: Chest deformities (pectus carinatum, pectus excavatum) Flush across the cheeks High arches of the feet Intellectual disability Knock knees Long limbs Mental disorders Nearsightedness Spidery fingers (arachnodactyly) Tall, thin build

Cystinuria is a condition characterized by the buildup of the amino acid cystine, a building block of most proteins, in the kidneys and bladder. As the kidneys filter blood to create urine, cystine is normally absorbed back into the bloodstream. People with cystinuria cannot properly reabsorb cystine into their bloodstream, so the amino acid accumulates in their urine. As urine becomes more concentrated in the kidneys, the excess cystine forms crystals. Larger crystals become stones that may lodge in the kidneys or in the bladder. Sometimes cystine crystals combine with calcium molecules in the kidneys to form large stones. These crystals and stones can create blockages in the urinary tract and reduce the ability of the kidneys to eliminate waste through urine. The stones also provide sites where bacteria may cause infections.
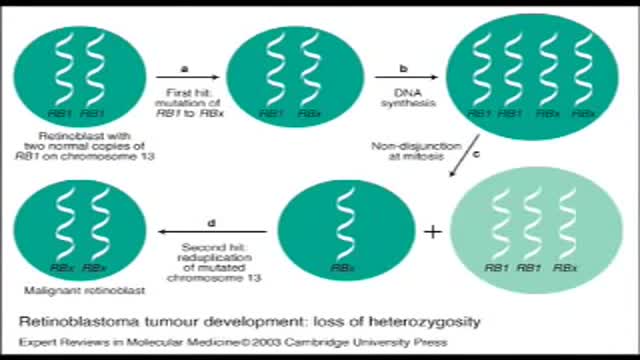
Retinoblastoma is an eye cancer that begins in the retina — the sensitive lining on the inside of your eye. Retinoblastoma most commonly affects young children, but can rarely occur in adults. Your retina is made up of nerve tissue that senses light as it comes through the front of your eye. The retina sends signals through your optic nerve to your brain, where these signals are interpreted as images. A rare form of eye cancer, retinoblastoma is the most common form of cancer affecting the eye in children. Retinoblastoma may occur in one or both eyes.
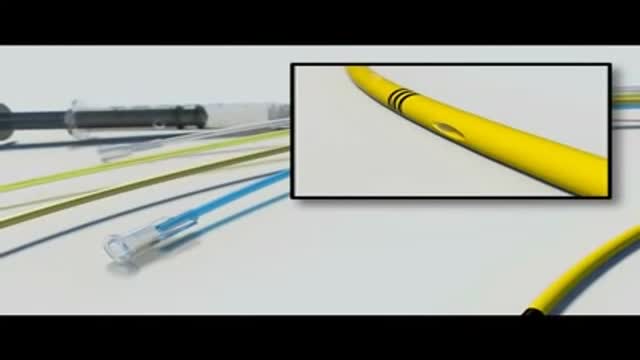
Any independent vertical movement of the transducer or the patient will affect the hydrostatic column of this fluid-filled system and thus alter the pressure measurements. At some time before or after PAC insertion, the system must therefore be zeroed to ambient air pressure. The reference point for this is the midpoint of the left atrium (LA), estimated as the fourth intercostal space in the midaxillary line with the patient in the supine position. With the transducer at this height, the membrane is exposed to atmospheric pressure, and the monitor is then adjusted to zero. Calibration Once zeroed, the monitoring system must be calibrated for accuracy. Currently, most monitors perform an automated electronic calibration. Two methods are used to manually calibrate and check the system. If the catheter has not been inserted, the distal tip of the PAC is raised to a specified height above the LA. For example, raising the tip 20 cm above the LA should produce a reading of approximately 15 mm Hg if the system is working properly (1 mm Hg equals 1.36 cm H 2 O). Alternatively, pressure can be applied externally to the transducer and adjusted to a known level using a mercury or aneroid manometer. The monitor then is adjusted to read this pressure, and the system is calibrated. Dynamic tuning Central pressures are dynamic waveforms (ie, they vary from systole to diastole) and thus have a periodic frequency. To monitor these pressures accurately, the system requires an appropriate frequency response. A poorly responsive system produces inaccurate pressure readings, and differentiating waveforms (eg, PA from pulmonary capillary wedge pressure [PCWP]) can become difficult. When signal energy is lost, the pressure waveform is dampened. Common causes of this are air bubbles (which are compressible), long or compliant tubing, vessel wall impingement, intracatheter debris, transducer malfunction, and loose connections in the tubing. A qualitative test of the frequency response is performed by flicking the catheter and observing a brisk high-frequency response in the waveform. After insertion, the system can be checked by using the rapid flush test. When flushed, an appropriately responsive system shows an initial horizontal straight line with a high-pressure reading. Once the flushing is terminated, the pressure drops immediately, which is represented by a vertical line that plunges below the baseline. A brief and well-defined oscillation occurs, followed by return of the PA waveform. A dampened system will not overshoot or oscillate, and causes a delay in returning to the PA waveform.
The average time from symptom onset to diagnosis has been reported to be approximately 2 years. Despite recent attempts at increasing the awareness of pulmonary arterial hypertension (PAH), especially associated PAH (APAH), this delay in diagnosis has not changed appreciably in recent years. Early symptoms are nonspecific. Often, neither the patient nor the physician recognizes the presence of the disease, which leads to delays in diagnosis. Complicating matters, idiopathic PAH (IPAH) requires an extensive workup in an attempt to elucidate an identifiable cause of the elevated pulmonary artery pressure. The most common symptoms and their frequency, reported in a national prospective study, are as follows: Dyspnea (60% of patients) Weakness (19%) Recurrent syncope (13%) Additional symptoms include fatigue, lethargy, anorexia, chest pain, and right upper quadrant pain. Cough, hemoptysis, and hoarseness are less common symptoms. Women are more likely to be symptomatic than men.
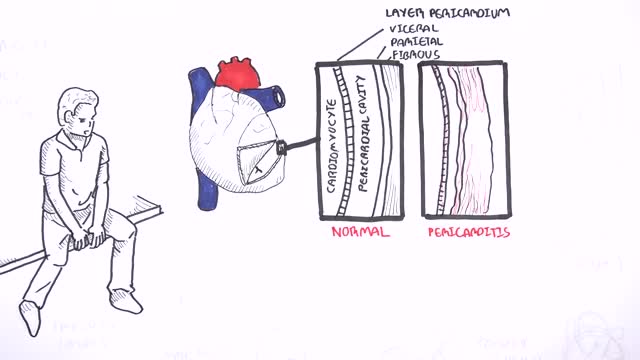
This video: Pericarditis is swelling and irritation of the pericardium, the thin sac-like membrane surrounding your heart. Pericarditis often causes chest pain and sometimes other symptoms. The sharp chest pain associated with pericarditis occurs when the irritated layers of the pericardium rub against each other. Pericarditis usually begins suddenly but doesn't last long (acute). When symptoms develop more gradually or persist, pericarditis is considered chronic. Most cases are mild and usually improve on their own. Treatment for more-severe cases may include medications and, rarely, surgery. Early diagnosis and treatment may help to reduce the risk of long-term complications from pericarditis.

Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo — the sudden sensation that you're spinning or that the inside of your head is spinning. Benign paroxysmal positional vertigo causes brief episodes of mild to intense dizziness. Benign paroxysmal positional vertigo is usually triggered by specific changes in the position of your head. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed. Although benign paroxysmal positional vertigo can be a bothersome problem, it's rarely serious except when it increases the chance of falls. You can receive effective treatment for benign paroxysmal positional vertigo during a doctor's office visit

Epley maneuver: Step 1 You will sit on the doctor's exam table with your legs extended in front of you. The doctor will turn your head so that it is halfway between looking straight ahead and looking directly to the side that causes the worst vertigo. Without changing your head position, the doctor will guide you back quickly so that your shoulders are on the table but your head is hanging over the edge of the table. In this position, the side of your head that is causing the worst vertigo is facing the floor. The doctor will hold you in this position for 30 seconds or until your vertigo stops. Epley maneuver: Step 2 Then, without lifting up your head, the doctor will turn your head to look at the same angle to the opposite side, so that the other side of your head is now facing the floor. The doctor will hold you in this position for 30 seconds or until your vertigo stops. Epley maneuver: Step 3 The doctor will help you roll in the same direction you are facing so that you are now lying on your side. (For example, if you are looking to your right, you will roll onto your right side.) The side that causes the worst vertigo should be facing up. The doctor will hold you in this position for another 30 seconds or until your vertigo stops. Epley maneuver: Step 4 The doctor will then help you to sit back up with your legs hanging off the table on the same side that you were facing. This maneuver is done with the assistance of a doctor or physical therapist. A single 10- to 15-minute session usually is all that is needed. When your head is firmly moved into different positions, the crystal debris (canaliths) causing vertigo will move freely and no longer cause symptoms.

Vertigo is a sensation of spinning. If you have these dizzy spells, you might feel like you are spinning or that the world around you is spinning. Causes of Vertigo Vertigo is often caused by an inner ear problem. Some of the most common causes include: BPPV. These initials stand for benign paroxysmal positional vertigo. BPPV occurs when tiny calcium particles (canaliths) clump up in canals of the inner ear. The inner ear sends signals to the brain about head and body movements relative to gravity. It helps you keep your balance. BPPV can occur for no known reason and may be associated with age. Meniere's disease. This is an inner ear disorder thought to be caused by a buildup of fluid and changing pressure in the ear. It can cause episodes of vertigo along with ringing in the ears (tinnitus) and hearing loss. Vestibular neuritis or labyrinthitis. This is an inner ear problem usually related to infection (usually viral). The infection causes inflammation in the inner ear around nerves that are important for helping the body sense balance

Megacolon, as well as megarectum, is a descriptive term. It denotes dilatation of the colon that is not caused by mechanical obstruction.[1, 2] Although the definition of megacolon has varied in the literature, most researchers use the measurement of greater than 12 cm for the cecum as the standard. Because the diameter of the large intestine varies, the following definitions would also be considered: greater than 6.5 cm in the rectosigmoid region and greater than 8 cm for the ascending colon. Megacolon can be divided into the following 3 categories: Acute megacolon ( pseudo-obstruction) Chronic megacolon, which includes congenital, acquired, and idiopathic causes Toxic megacolon
Men need to know that breast cancer is not limited to women. Possible symptoms of breast cancer to watch for include: A lump or swelling, which is usually (but not always) painless Skin dimpling or puckering Nipple retraction (turning inward) Redness or scaling of the nipple or breast skin Discharge from the nipple Sometimes a breast cancer can spread to lymph nodes under the arm or around the collar bone and cause a lump or swelling there, even before the original tumor in the breast tissue is large enough to be felt. These changes aren't always caused by cancer. For example, most breast lumps in men are caused by gynecomastia (a harmless enlargement of breast tissue). Still, if you notice any breast changes, you should see a health care professional as soon as possible.
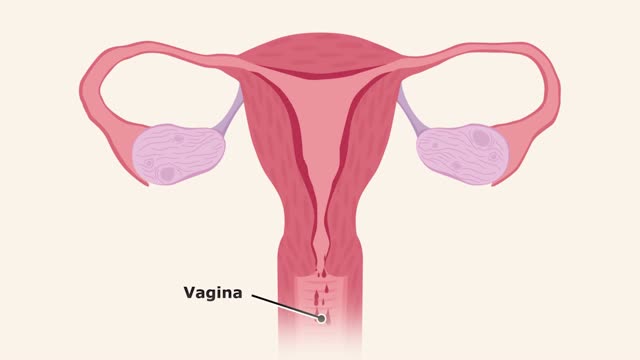
The menstrual cycle is the monthly series of changes a woman's body goes through in preparation for the possibility of pregnancy. Each month, one of the ovaries releases an egg — a process called ovulation. At the same time, hormonal changes prepare the uterus for pregnancy.
Emphysema gradually damages the air sacs (alveoli) in your lungs, making you progressively more short of breath. Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease Smoking is the leading cause of emphysema. Your lungs' alveoli are clustered like bunches of grapes. In emphysema, the inner walls of the air sacs weaken and eventually rupture — creating one larger air space instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream. When you exhale, the damaged alveoli don't work properly and old air becomes trapped, leaving no room for fresh, oxygen-rich air to enter. Treatment may slow the progression of emphysema, but it can't reverse the damage.
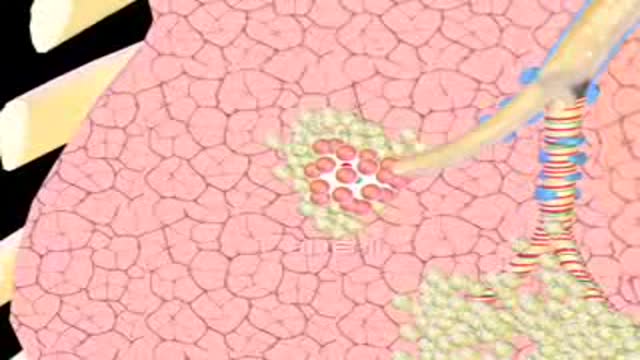
Emphysema gradually damages the air sacs (alveoli) in your lungs, making you progressively more short of breath. Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD). Smoking is the leading cause of emphysema. Your lungs' alveoli are clustered like bunches of grapes. In emphysema, the inner walls of the air sacs weaken and eventually rupture — creating one larger air space instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream. When you exhale, the damaged alveoli don't work properly and old air becomes trapped, leaving no room for fresh, oxygen-rich air to enter. Treatment may slow the progression of emphysema, but it can't reverse the damage.
Acute bronchitis and pneumonia share many of the same symptoms, and some people with acute bronchitis are at risk for getting pneumonia. Although acute bronchitis usually goes away within a few weeks, pneumonia can be a serious condition, especially in older adults. The following table outlines some differences between acute bronchitis and pneumonia. There are variations in symptoms of both conditions, so if you think you might have pneumonia, always check with your doctor.