Latest videos
Acute leukaemias develop quickly and need to be treated urgently. Chronic leukaemias develop more slowly and may not need to be treated for some time after they are diagnosed. Some forms may not require any treatment. Myeloid leukaemias arise from myeloid stem cells and are characterised by the accumulation of cancerous myeloid cells. Lymphoid leukaemias arise from lymphoid stem cells and are characterised by the accumulation of cancerous lymphoid cells such as B-cells and T-cells. The most common forms of leukaemia in adults are CLL and AML, and the common cancer in children is ALL. Leukaemia is more common in adults.
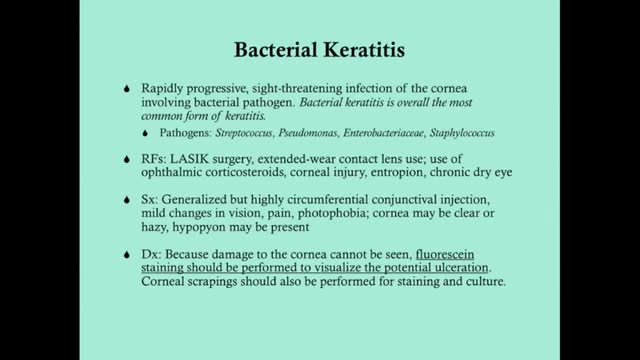
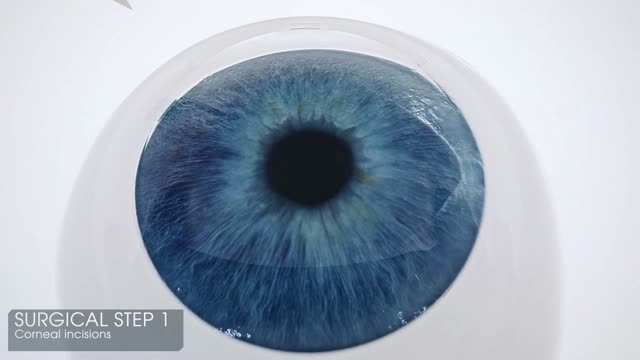
Keratitis is an inflammation of the cornea — the clear, dome-shaped tissue on the front of your eye that covers the pupil and iris. Keratitis is sometimes caused by an infection involving bacteria, viruses, fungi or parasites. Noninfectious keratitis can be caused by a minor injury, wearing your contact lenses too long or other noninfectious diseases. If you have eye redness or other symptoms of keratitis, make an appointment to see your doctor. With prompt attention, mild to moderate cases of keratitis can usually be effectively treated without loss of vision. If left untreated, or if an infection is severe, keratitis can lead to serious complications that may permanently damage your vision.
Pink eye (conjunctivitis) is an inflammation or infection of the transparent membrane (conjunctiva) that lines your eyelid and covers the white part of your eyeball. When small blood vessels in the conjunctiva become inflamed, they're more visible. This is what causes the whites of your eyes to appear reddish or pink. Pink eye is commonly caused by a bacterial or viral infection or an allergic reaction. It may affect one or both eyes. Pink eye can be irritating, but it rarely affects your vision. Treatments can help ease the discomfort of pink eye. Because pink eye can be contagious, early diagnosis and treatment can help limit its spread.
HOW BABY GROWS IN THE WOMB DURING PREGNANCY
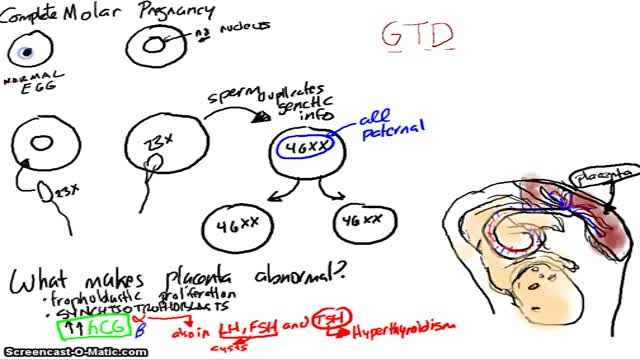
A molar pregnancy — also known as hydatidiform mole — is a noncancerous (benign) tumor that develops in the uterus. A molar pregnancy starts when an egg is fertilized, but instead of a normal, viable pregnancy resulting, the placenta develops into an abnormal mass of cysts. In a complete molar pregnancy, there's no embryo or normal placental tissue. In a partial molar pregnancy, there's an abnormal embryo and possibly some normal placental tissue. The embryo begins to develop but is malformed and can't survive. A molar pregnancy can have serious complications — including a rare form of cancer — and requires early treatment.
What is a mole? Many people refer to a mole as any dark spot or irregularity in the skin. Doctors use different terms. But the following types of skin marks such as these are not treated the same way moles are and are not discussed here: Birthmarks Abnormal formations of blood vessels (hemangiomas) Keratoses (benign or precancerous spots, which appear after about age 30 years)
Symptoms Burning stomach pain Feeling of fullness, bloating or belching Fatty food intolerance Heartburn Nausea The most common peptic ulcer symptom is burning stomach pain. Stomach acid makes the pain worse, as does having an empty stomach. The pain can often be relieved by eating certain foods that buffer stomach acid or by taking an acid-reducing medication, but then it may come back. The pain may be worse between meals and at night. Nearly three-quarters of people with peptic ulcers don't have symptoms. Less often, ulcers may cause severe signs or symptoms such as: Vomiting or vomiting blood — which may appear red or black Dark blood in stools, or stools that are black or tarry Trouble breathing Feeling faint Nausea or vomiting Unexplained weight loss Appetite changes
Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is stomach pain. Peptic ulcers include: Gastric ulcers that occur on the inside of the stomach Duodenal ulcers that occur on the inside of the upper portion of your small intestine (duodenum) The most common causes of peptic ulcers are infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of aspirin and certain other painkillers, such as ibuprofen (Advil, Motrin, others) and naproxen sodium (Aleve, Anaprox, others). Stress and spicy foods do not cause peptic ulcers. However, they can make your symptoms worse.
Pulmonary surfactant is a mixture of lipids and proteins that is produced by alveolar type II epithelial cells (AEC2) and secreted into the airspaces. Phospholipids are the major component of surfactant by weight, and are essential for lowering surface tension at the air-liquid interface, which prevents alveolar collapse at end-expiration. Four proteins highly expressed in the lung and found in surfactant are designated surfactant proteins (SP) A, B, C, and D. Additional proteins including ABCA3 and NKX2.1 are also important for the production of functional surfactant. The surfactant proteins are developmentally regulated, such that their expression increases in later gestation
Genetic surfactant dysfunction disorders are caused by mutations in genes encoding proteins critical for the production and function of pulmonary surfactant. These rare disorders may produce familial or sporadic lung disease, with clinical presentations ranging from neonatal respiratory failure to childhood- or adult-onset interstitial lung disease. An overview of these disorders is presented in the table.. Interstitial lung diseases in children until recently were categorized by their histologic appearance in a manner similar to that used for adult forms of interstitial lung disease (ILD). In children, the lung histopathology findings associated with desquamative interstitial pneumonitis (DIP) are now known to often result from genetic mechanisms that disrupt normal surfactant production and metabolism. By contrast, DIP in adults is considered to represent a distinct type of ILD, which is strongly associated with cigarette smoking and carries a relatively favorable prognosis [1]. These genetic disorders also result in histopathologic patterns other than DIP, including findings of pulmonary alveolar proteinosis and chronic pneumonitis of infancy. An understanding of the pathogenesis of these disorders permits a mechanistic classification as genetic surfactant dysfunction disorders instead of their previous classification based upon histologic appearance.
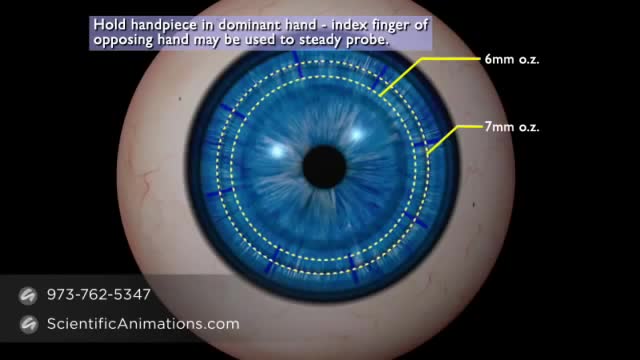
Less than a decade ago, corneal transplantation took a big leap forward with the introduction of Descemet’s stripping endothelial keratoplasty (DSEK), which removes only Descemet’s membrane and the diseased endothelium and replaces them with a thin, tripartite donor graft of posterior corneal stroma, Descemet’s membrane, and healthy endothelium. Then came DSAEK, in which the donor graft is prepared with an automated microkeratome, allowing for easier donor preparation and reproducible results by surgeons and eye bank technicians.1 DSAEK has proved to have many advantages over penetrating keratoplasty (PK) and its endothelial predecessors (see “A Brief History of Endothelial Keratoplasty”). Now DSAEK is being compared with a newer technique, Descemet’s membrane endothelial keratoplasty (DMEK), which has emerged as a promising alternative—grafting only Descemet’s membrane and endothelium, allowing for a pure anatomical replacement of only what was removed and the possibility of even better vision with quicker healing.1 Although indications for these procedures are similar, each has unique benefits and drawbacks. Five cornea surgeons offer their perspectives on the procedures and their thoughts on whether it may be time to move to the newer surgery.
A cornea transplant, also called keratoplasty, is a surgical procedure to replace part of your cornea with corneal tissue from a donor. Your cornea is the transparent, dome-shaped surface of your eye that accounts for a large part of your eye's focusing power. A cornea transplant can restore vision, reduce pain and improve the appearance of a damaged or diseased cornea. Most cornea transplant procedures are successful. But cornea transplant carries a small risk of complications, such as rejection of the donor cornea.
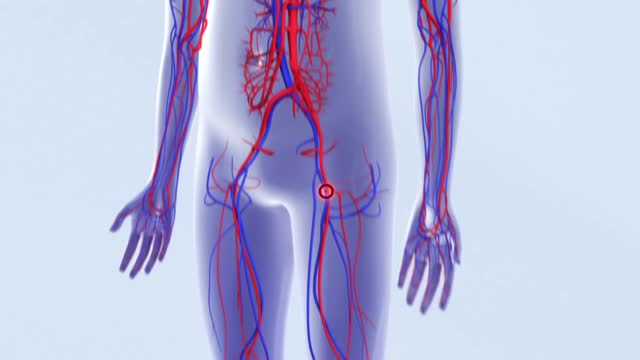
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs. Deep vein thrombosis can cause leg pain or swelling, but may occur without any symptoms. Deep vein thrombosis can develop if you have certain medical conditions that affect how your blood clots. Deep vein thrombosis can also happen if you don't move for a long time, such as after surgery, following an accident, or when you are confined to a hospital or nursing home bed. Deep vein thrombosis is a serious condition because blood clots in your veins can break loose, travel through your bloodstream and lodge in your lungs, blocking blood flow (pulmonary embolism).
The increased risk of thrombosis in patients with active cancer has multiple causes. Acute thrombosis of the aorta is an exceedingly rare but potentially devastating complication in patients with cancer receiving cisplatin-based chemotherapy. Prompt diagnosis and definitive treatment are imperative to decrease morbidity and mortality. Early diagnosis is difficult because initial presentation is often nonspecific, requiring a high degree of clinical suspicion. We report 4 cases of acute thrombosis of the abdominal aorta in patients with cancer receiving cisplatin-based chemotherapy. We review the clinical aspects, recommended investigation, and treatment of this potentially fatal complication.
Pulmonary embolism symptoms can vary greatly, depending on how much of your lung is involved, the size of the clots, and whether you have underlying lung or heart disease. Common signs and symptoms include: Shortness of breath. This symptom typically appears suddenly and always gets worse with exertion. Chest pain. You may feel like you're having a heart attack. The pain may become worse when you breathe deeply (pleurisy), cough, eat, bend or stoop. The pain will get worse with exertion but won't go away when you rest. Cough. The cough may produce bloody or blood-streaked sputum. Other signs and symptoms that can occur with pulmonary embolism include: Leg pain or swelling, or both, usually in the calf Clammy or discolored skin (cyanosis) Fever Excessive sweating Rapid or irregular heartbeat Lightheadedness or dizziness
Vasculitis is an inflammation of your blood vessels. It causes changes in the walls of blood vessels, including thickening, weakening, narrowing and scarring. These changes restrict blood flow, resulting in organ and tissue damage. There are many types of vasculitis, and most of them are rare. Vasculitis might affect just one organ, such as your skin, or it may involve several. The condition can be short term (acute) or long lasting (chronic). Vasculitis can affect anyone, though some types are more common among certain groups. Depending on the type you have, you may improve without treatment. Or you will need medications to control the inflammation and prevent flare-ups. Vasculitis is also known as angiitis and arteritis.
physical exam -Newborn Normal:Behavior
Most of the time when someone with cancer is told they have cancer in the bones, the doctor is talking about a cancer that has spread to the bones from somewhere else. This is called metastatic cancer. It can be seen in many different types of advanced cancer, like breast cancer, prostate cancer, and lung cancer. When these cancers in the bone are looked at under a microscope, they look like the tissue they came from. For example, if someone has lung cancer that has spread to bone, the cells of the cancer in the bone still look and act like lung cancer cells. They do not look or act like bone cancer cells, even though they are in the bones. Since these cancer cells still act like lung cancer cells, they still need to be treated with drugs that are used for lung cancer. For more information about metastatic bone cancer, please see our document called Bone Metastasis, as well as the document on the specific place the cancer started (Breast Cancer, Lung Cancer, Prostate Cancer, etc.). Other kinds of cancers that are sometimes called “bone cancers” start in the blood forming cells of the bone marrow − not in the bone itself. The most common cancer that starts in the bone marrow and causes bone tumors is called multiple myeloma. Another cancer that starts in the bone marrow is leukemia, but it is generally considered a blood cancer rather than a bone cancer. Sometimes lymphomas, which more often start in lymph nodes, can start in bone marrow. Multiple myeloma, lymphoma, and leukemia are not discussed in this document. For more information on these cancers, refer to the individual document for each. A primary bone tumor starts in the bone itself. True (or primary) bone cancers are called sarcomas. Sarcomas are cancers that start in bone, muscle, fibrous tissue, blood vessels, fat tissue, as well as some other tissues. They can develop anywhere in the body. There are several different types of bone tumors. Their names are based on the area of bone or surrounding tissue that is affected and the kind of cells forming the tumor. Some primary bone tumors are benign (not cancerous), and others are malignant (cancerous). Most bone cancers are sarcomas.
10 YOUNGEST Moms Of All Time
An orgasm is a feeling of intense sexual pleasure that happens during sexual activity. It's sometimes called "coming" or "climaxing". Both men and women have orgasms.