Latest videos

External cephalic version, or version, is a procedure used to turn a fetus from a breech position or side-lying (transverse) position into a head-down (vertex) position before labor begins. When successful, version makes it possible for you to try a vaginal birth.

Doctors save the life of an unborn baby who was injured along with her mother in a missile attack in the Syrian city of Aleppo. The video shows a team of emergency medical workers delivering the baby by Cesarean section and then treating the newborn for the shrapnel wounds covering her body and one very large gash in her head. “Medics can be seen frantically reviving the baby, after delivering her by emergency cesarean, as she lies motionless,” the article states. “Eventually the tiny newborn begins to cry and seemingly comes to life as she is given an oxygen mask and rubbed vigorously.” “According to Reuters, the woman also has three other children, all of whom were injured in the attack, but are reported by doctors in the hospital to be in a good condition,” the Daily Mirror article states. The article does not provide the gestational age of the baby before it was delivered. The article said the pregnant woman was hit by a barrel bomb – “crude explosives and shrapnel and dropped from helicopters used by [Syrian] President Bashir al-Assad’s regime." The article notes an estimated 7.6 million Syrians have been displaced by the ongoing civil war and that 320,000, including 11,000 children, have been killed in the conflict. The Daily Mirror also reports that the doctors suggested that the tiny girl be named Amal, which means hope in Arabic. UK Daily Mirror: Incredible footage shows Syrian doctors perform lifesaving caesarean after missile strike leaves shrapnel embedded in unborn baby's face
Sex reassignment surgery for male-to-female involves reshaping the male genitals into a form with the appearance of, and, as far as possible, the function of female genitalia. Prior to any surgeries, patients usually undergo hormone replacement therapy (HRT), and, depending on the age at which HRT begins, facial hair removal. There are associated surgeries patients may elect to, including facial feminization surgery, breast augmentation, and various other procedures

Autonomous Tumor Localization and Extraction: Palpation, Incision, Debridement and Adhesive Closure with the da Vinci Research Kit. This video demonstrates a successful trial of the entire five-step procedure where human input is required only at four points to change tools. We also show failure modes of the current autonomous system and we are working on experiments to characterize the reliability of each step and on incorporating computer vision and new probing algorithms to improve robustness.

An amputation is the removal of an extremity or appendage from the body. Amputations in the upper extremity can occur as a result of trauma, or they can be performed in the treatment of congenital or acquired conditions. Although successful replantation represents a technical triumph to the surgeon, the patient's best interests should direct the treatment of amputations. The goals involved in the treatment of amputations of the upper extremity include the following : Preservation of functional length Durable coverage Preservation of useful sensibility Prevention of symptomatic neuromas Prevention of adjacent joint contractures Early return to work Early prosthetic fitting These goals apply differently to different levels of amputation. Treatment of amputations can be challenging and rewarding. It is imperative that the surgeon treat the patient with the ultimate goal of optimizing function and rehabilitation and not become absorbed in the enthusiasm of the technical challenge of the replantation, which could result in poorer outcome and greater financial cost due to lost wages, hospitalization, and therapy.

http://vene-varicose-rimedi.good-info.co Vene Varicose, Vene Varicose Gambe, Chiva Varici, Laser Per Vene Varicose, Terapia Vene Varicose. Cosa Sono Le Vene Varicose e Quali Sono I Fattori Che Le Determinano? Le vene varicose si verificano quando il sangue non scorre naturalmente attraverso le vene del corpo verso il cuore. Quando ciò accade il sangue si accumula e ristagna nelle vene, di solito nelle vene delle gambe, dando alla pelle un aspetto davvero brutto e sgradevole. Quali Sono Le Vere Cause Delle Vene Varicose? Se si hanno vene varicose probabilmente ci si è già posti questa domanda più di una volta. Le vene varicose possono essere prodotte da vari fattori, quindi analizzeremo i fattori più importanti che possono produrle. 1. Vene Danneggiate. Molte volte le vene non funzionano correttamente, non permettendo al flusso dell sangue di circolare correttamente. Questo a lungo termine causa l'apparizione delle vene varicose. 2. L'Età. Nel corso degli anni molte parti del nostro corpo non funzionano più correttamente e le vene non sono un'eccezione. Gradualmente perdono la loro elasticità e diventano soggette a tutti i tipi di disturbi vascolari. 3. Il Sesso. Le donne sono più propense degli uomini a sviluppare le vene varicose. Le vene varicose compaiono di solito durante la fase di gravidanza, perché in questa fase si produce una maggiore quantità di estrogeni, un ormone che provoca un effetto rilassante nelle vene impedendo la corretta circolazione del sangue in esse. Altri fattori che possono produrre la comparsa delle vene varicose sono la menopausa femminile e le mestruazioni. 4. Stipsi. Le persone che soffrono di stipsi hanno maggiori probabilità di sviluppare vene varicose poiché al tempo dell'evacuazione lo sforzo è maggiore aumenteranno così le forti pressioni sulle vene. Come risultato di questo sforzo, le vene si danneggiano, si stirano e a lungo termine, si produce la comparsa di varici. 5. La Genetica. Se qualcuno nella vostra famiglia ha le vene varicose, è probabile che si svilupperanno in voi a un certo punto della vita. Questo è il motivo per il quale è molto importante sapere la storia della famiglia in modo che si possa essere in grado di identificare il fattore che ha dato origine alle vene varicose e trovare così il corretto trattamento per combatterle. 6. Il Sovrappeso. L’obesità e il sovrappeso possono portare alla comparsa di vene varicose, l'eccesso di peso esercita tensione in molte aree del corpo, includendo le vene. Inoltre, quando una persona è in sovrappeso viene ostacolata la circolazione del sangue, perché si mettono sotto pressione le vene e questo le danneggia. 7. Lesioni Alle Gambe. Le persone che hanno subito traumi a una o entrambe le gambe sono suscettibili allo sviluppo delle vene varicose. Quando si parla di lesioni queste includono: problemi di circolazione nelle gambe, interventi chirurgici, frattura della tibia e perone, ecc. 8. Stile Di Vita Sedentario. La vita sedentaria e le cattive abitudini alimentari possono favorire la comparsa di vene varicose. Una persona che passa seduta lunghi periodi di tempo, magari aggravando la situazione accavallando le gambe, impedisce al sangue di percorrere la sua strada consueta delle gambe al cuore. Il sangue non riesce quindi a lottare contro la forza di gravità e la mancanza di attività nelle gambe causa l'accumulo del sangue nello stesso luogo, portando alla creazione delle vene varicose. 9. Abbigliamento Stretto. Una certa varietà di capi d'abbigliamento e accessori, come ad esempio le scarpe con i tacchi alti, impediscono il flusso corretto del sangue per il corpo e favoriscono l'emergere della varici. Le scarpe chiuse con tacchi alti stringono il piede e impediscono il naturale flusso del sangue verso l'alto, in direzione del cuore. In questo modo il sangue resta all'interno delle vene nelle gambe e a lungo termine possono apparire le vene varicose. Con l'abbigliamento troppo stretto accade la stessa cosa perché impedisce che il sangue scorra correttamente per il corpo. 10. Attività Fisica Ad Alto Impatto. L’Attività fisica ad alto impatto come il sollevamento di pesi è molto popolare perché contribuisce a tonificare in poco tempo i vari gruppi muscolari. Tuttavia il sollevamento di oggetti pesanti, come i pesi, può favorire la comparsa di varici. Tutto questo è ciò che si può imparare in questa guida, Qui scoprirete i migliori metodi naturali per prevenire e contrastare la comparsa di vene varicose! http://vene-varicose-rimedi.good-info.co

Skin Cysts Cysts are noncancerous, closed pockets of tissue that can be filled with fluid, pus, or other material. Cysts are common on the skin and can appear anywhere. They feel like large peas under the surface of the skin. Cysts can develop as a result of infection, clogging of sebaceous glands (oil glands), or around foreign bodies, such as earrings.

Carpal tunnel surgery, also called carpal tunnel release (CTR) and carpal tunnel decompression surgery, is a surgery in which the transverse carpal ligament is divided. It is a treatment for carpal tunnel syndrome and recommended when there is static (constant, not just intermittent) numbness, muscle weakness, or atrophy, and when night-splinting no longer controls intermittent symptoms of pain in the carpal tunnel. In general, milder cases can be controlled for months to years, but severe cases are unrelenting symptomatically and are likely to result in surgical treatment.
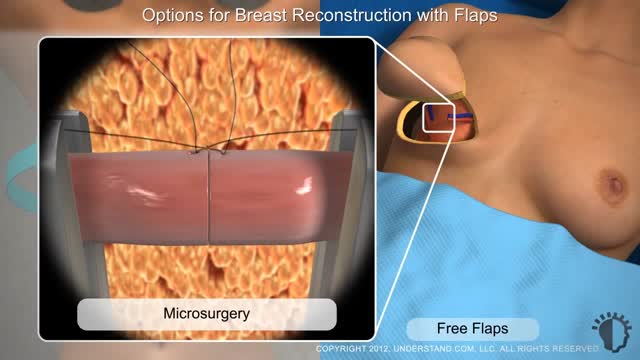
Typically, breast reconstruction takes place during or soon after mastectomy, and in some cases, lumpectomy. Breast reconstruction also can be done many months or even years after mastectomy or lumpectomy. During reconstruction, a plastic surgeon creates a breast shape using an artificial implant (implant reconstruction), a flap of tissue from another place on your body (autologous reconstruction), or both.

Rhinoplasty enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. Rhinoplasty surgery can change: Nose size in relation to facial balance. Nose width at the bridge or in the size and position of the nostrils.

Download Clash of Clans for free for mobile devices. http://supr.cl/ThisArmy
I don't know you, BigBuffetBoy85
But if you think you can humiliate me and take my gold, think again.
Oh, I am coming for you with lots of Barbarians and Dragons. I can't wait to destroy your village, while you beg for mercy, but you will get no mercy. I will have my revenge.
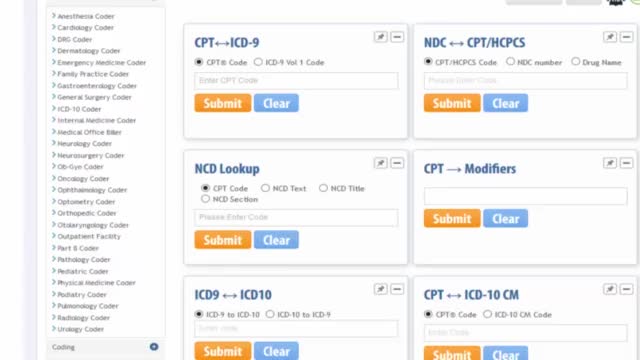
Check out how Physician Coder – an online specialty solution – can help you meet your practice’s goals for error-free coding. From helping you meet all your ICD-10 coding needs from one place with code lookup, crosswalk, superbill converter, scrubber, and monthly specialty articles to helping you review CPT® 2016 changes with expert analysis for your specialty, we have you covered. Plus, you’ll also learn how to stay up-to-date on 2016 fee schedule details like RVUs, global days, and MUEs; check the latest CCI edits and view LCD policy details.
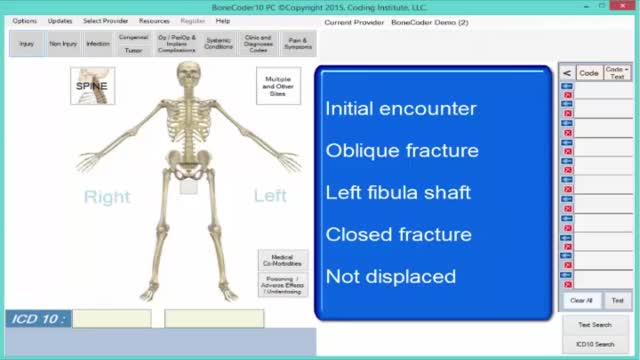
Learn to use SuperCoder’s intuitive online coding and billing tools by watching these step-by-step videos from experts. From learning how to use the ICD-10 Superbill Converter or the popular Physician Coder tool to understanding what SuperCoder’s latest launch – Intuitive Coder – is all about, our videos have you covered!
Health disorders are part of life when you are getting older , Some problems are life-threatening, while others lower the quality of life. The good news is that these Health disorders can be managed effectively.
homecareassistancesouthjersey.com
Liposuction surgery is used to reduce the extra fat from your body with the very safe surgical process but you must consult with your Surgeon first when deciding about using this surgery to meet your body fat needs.
Vaser Lipo was Rs. 65000 per region. Now at Rs. 50,000 per Region
Offer valid till 31st March only
Vaser Liposuction technology helps to reduce the healing time and increase effective skin contraction, giving you smooth, slim results. With Liposuction there are no stitches, only a single 1cm small incision giving you permanent large result.
For further information, are available visit our website:
http://www.imageclinic.org/liposuction.html
Your Query for Chat and call +91-9818369662, 9958221983 (WhatsApp)

MEDICAL DESIGN SIALKOT. ®
( Worldwide Medical Health care Supporting Company )
We are the Manufacturer And Exporter Of High
Quality Surgical Instruments, Dental Instruments, Veterinary Instruments, Ophthalmic Instruments, TC Instruments, from Pakistan and are registered member of
SIALKOT CHAMBER OF COMMERCE AND INDUSTRY(SCCI).
We assure our customers Premium Quality Surgical Instruments at very affordable prices, to establish long term mutual Beneficial relationship.
Further we have organized our manufacturing lines in such a way that
our skilled workforce is able to produce specified products as per our
valued customers specification.
MEDICAL DESIGN
Mr. Sajeel Anwar
Address:- Amir Street, Ali Ul haq Road,
Model Town SIALKOT-PAKISTAN
Call : 0092 345 6768889
Email: info@medicaldesignpk.com
Skype : medicaldesignpk