Latest videos
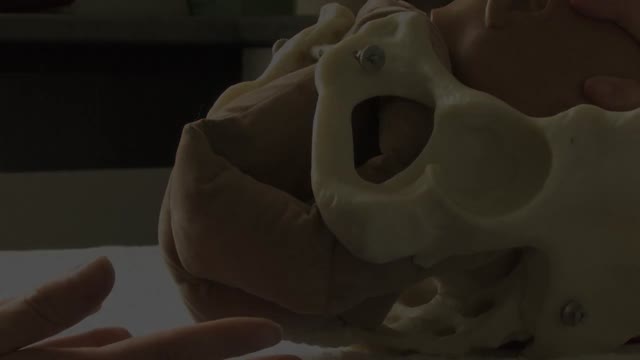
Not every woman undergoes a traditional vaginal delivery with the birth of her child. Under conditions of fetal or maternal distress, or in the case of breech presentation (when a baby is turned feet first at the time of delivery), or if the woman’s first baby was born by cesarean delivery, a procedure called a cesarean section may be required. During a cesarean, a doctor will make either a lateral incision in the skin just above the pubic hair line, or a vertical incision below the navel. As the incision is made, blood vessels are cauterized to slow bleeding. After cutting through the skin, fat, and muscle of the abdomen, the membrane that covers the internal organs is opened, exposing the bladder and uterus. At this time the physician will generally insert his or her hands into the pelvis in order to determine the position of the baby and the placenta. Next, an incision is made into the uterus and any remaining fluids are suctioned from the uterus. The doctor then enlarges the incision with his or her fingers. The baby’s head is then grasped and gently pulled with the rest of its body from the mother’s uterus. Finally, the abdominal layers are sewn together in the reverse order that they were cut. The mother is allowed to recover for approximately three to five days in the hospital. She will also be quite sore and restricted from activity for the following several weeks. There are several potential complications associated with this procedure that should be discussed with a doctor prior to surgery.
The majority of fetuses are in a breech presentation early in pregnancy. By week 38th week of gestation, however, the fetus normally turns to a cephalic presentation. Although the fetal head is the widest single diameter, the fetus’s buttocks [ breech], plus the lower extremities, actually takes up more space. The fundus, being the largest part of the uterus, probably accounts for the fact that in approximately 97% of all pregnancies, the fetus turns so that the buttocks and lower extremities are in the fundus. Vaginal delivery of a breech presentation requires great skill if the fetus is not to be damaged. With the low rate of vaginal breech deliveries in the developed world, experience is being lost. 6% of women with breech presentation still have a vaginal breech delivery as they present too late - so units need to retain a high level of preparedness. Types of breech presentation: I. Complete breech [ flexed breech]: The fetal attitude is one of complete flexion, with hips and knees both flexed and the feet tucked in beside the buttocks. The presenting part consists of two buttocks, external genitalia and two feet. It is commonly present in multiparae. II. Incomplete breech: This is due to varying degrees of extension of thighs or legs at podalic pole. Three varieties are possible; - Breech with extended legs [ frank breech ]: The breech presents with the hips flexed and legs extended on the abdomen. 70% of breech presentations are of this type and it is particularly common in primigravidae whose good uterine muscle tone inhibits flexion of the legs and free turning of the fetus. - Footling breech: This is rare. One or both feet present because neither hips nor knees are fully flexed. The feet are lower than the buttocks, which distinguishes it from the complete breech. - Knee presentation: This is very rare. Thighs are extended but the knees are flexed, bringing the knees down to present at the brim.
This is the incredible moment a new-born baby arrived still inside its amniotic sac, completely intact. The tiny infant can be seen moving and stretching still inside the sac, as medics prepare to snip the new born free. The amniotic sac is a thin but durable membrane filled with fluid which helps keep a baby warm and safe from bumps during pregnancy. When it breaks, this is typically referred to as a woman's 'waters breaking' shortly before she gives birth. But in rare cases, less than 1-in-80,000 births, the baby is delivered with the membranes still intact and this is known as a 'caul birth'. Some babies are born with part of the membrane still attached to them, but to be born completely encased in the intact membrane is incredibly rare. Many people still believe the phenomenon to be a good omen for the child's infancy and it is has even been suggested, but not proven, that caul babies will always have a natural affinity for water. The video was taken in Spain on Saturday and captures the rare moment the baby was born with the membrane covering its entire body, just minutes after its twin was delivered normally.
Shoulder dystocia is a specific case of obstructed labour whereby after the delivery of the head, the anterior shoulder of the infant cannot pass below, or requires significant manipulation to pass below, the pubic symphysis. It is diagnosed when the shoulders fail to deliver shortly after the fetal head. Shoulder dystocia is an obstetric emergency, and fetal demise can occur if the infant is not delivered, due to compression of the umbilical cord within the birth canal. It occurs in approximately 0.3-1% of vaginal births. Contemporary management of shoulder dystocia requires a calm operator and a well-thought-out plan of action. It is imperative that if not already present, help is summoned immediately after shoulder dystocia is recognized. This help may include additional nursing staff, an anesthesiologist, a pediatrician or neonatologist and an additional obstetrician or midwife. Future coordination may demonstrate that rapid response teams are best suited to attend to this emergency.
Your baby's sex is set at conception. At around 7 weeks, your baby's internal sex organs – such as ovaries and testes – begin to form in the abdomen. Male and female sex organs and genitalia look the same at this stage because they're derived from the same structures. At around 9 weeks, boys and girls begin to develop differently. In girls, a tiny bud emerges between the tissue of the legs. This bud will become the clitoris. The membrane that forms a groove below the bud separates to become the labia minora and the vaginal opening. By 22 weeks, the ovaries are completely formed and move from the abdomen to the pelvis. They already contain a lifetime supply of 6 million eggs. In boys, the bud develops into the penis and starts to elongate at around 12 weeks. The outer membrane grows into the scrotal sac that will later house the testicles. By 22 weeks, the testes have formed in the abdomen. They already contain immature sperm. Soon they'll begin their descent to the scrotum, but it's a long journey. They'll reach their destination late in pregnancy, or for some boys, after birth. If you're eager to find out whether you're having a girl or a boy, you'll have to wait until you're at least 17 weeks pregnant. That's when the genitals have developed enough to be seen on an ultrasound.
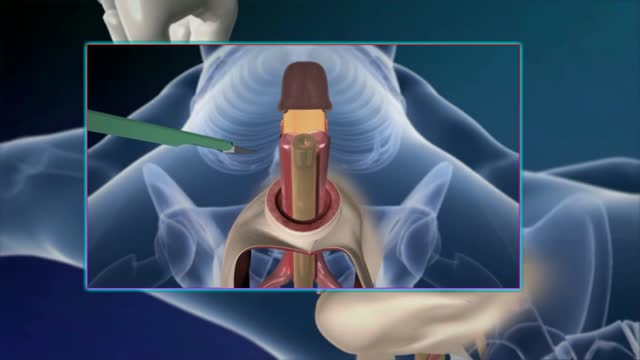
External cephalic version, or version, is a procedure used to turn a fetus from a breech position or side-lying (transverse) position into a head-down (vertex) position before labor begins. When successful, version makes it possible for you to try a vaginal birth.
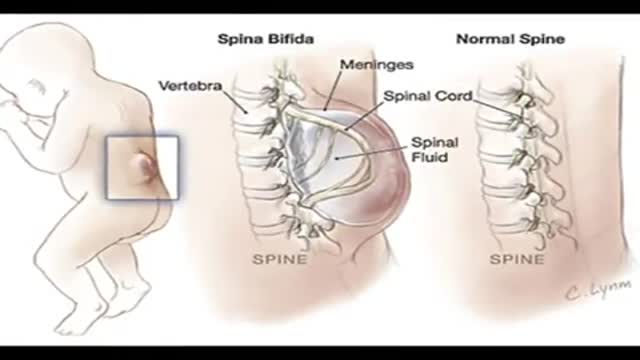
What is Myelomeningocele and how does it affect my baby? Myelomeningocele (MMC), one of the most severe forms of spina bifida, is a condition where the fetus’ spinal cord fails to close during development. This happens between 20 and 28 days of gestation, often before a woman knows she is pregnant. Because the spinal cord does not close, many of the nerves are exposed, resulting in damage to the cord as the pregnancy continues. Spina bifida can impact the nervous system, bones and muscles, kidneys and bladder. The location on the spine where the undeveloped area occurs is called the level of the spina bifida. Because nerve damage at this site prevents function below that level, the higher the level, the greater the impact on normal development and function. The opening in the spinal cord also results in loss of the fluid surrounding the nervous system. This causes the brain to be positioned further down into the upper spinal column than normal, which is called an Arnold Chiari II malformation. When this happens, the normal flow of fluid out of the brain is obstructed, causing Hydrocephalus, an excess of cerebrospinal fluid within the brain. After birth, most children with Hydrocephalus need to have the extra fluid shunted out of the brain into the abdomen via a ventriculoperitoneal shunt. MMC affects about 1 in every 1,000 babies, and it ranges in severity. Some children, with mild cases very low on the spinal cord, can function nearly normally. More severe cases can cause leg weakness and paralysis, as well as Hydrocephalus, and the Arnold Chiari malformation. People with MMC often live long lives, especially if the condition is diagnosed and treated early. How is Myelomeningocele diagnosed? At about 15 weeks gestation, a blood test measuring the levels of alpha-fetoprotein can show the physician that there might be a problem. After that, an ultrasound is performed to detect the MMC, but also to detect the conditions that can result from it, such as Hydrocephalus, the Chiari malformation, and any problems with the lower extremities. In all cases, we perform a fetal MRI to gain more detailed information and we perform a fetal echocardiogram (echo) to rule out any problem with the heart. What is the prenatal surgery for Myelomeningocele, and how does it differ from postnatal surgery? Until recently, the only way to treat MMC was surgery after birth. But, now that the nine-year long Management of Myelomeningocele (MOMS) trial has been completed, we know that repairing the MMC before birth, in the womb, can be beneficial to the baby’s outcome. The SSM Health St. Louis Fetal Care Institute has one of the fastest growing fetal MMC repair programs in the country. The results of the trial found that prenatal treatment helps reduce, or even eliminate, the major complications of MMC—the Hydrocephalus, the Chiari malformation, and the lack of movement in the lower extremities. Diagnosis and repair of the MMC before birth can make a big difference in the way the baby develops. The MOMS trial showed that babies treated in the womb need half the VP shunts, often have reversal of the Arnold-Chiari malformation, and are more likely to walk, at least until 30 months. Long-term follow up data of children treated with prenatal surgery is still being collected, so the benefit beyond 30 months is not fully known. The operation for open fetal surgery for MMC repair involves making a small opening in the uterus, then closing the spinal cord opening just like after birth. The womb is repaired and the mother is in the hospital for four to five days. The surgery is performed between 19 and 26 weeks of the pregnancy. Mothers usually stay locally for about two weeks so that we can monitor the pregnancy. After this, they can return home for delivery. Because of the scar caused by the surgery on the uterus, the baby and all future babies have to be delivered by Cesarean birth. The benefit to the fetal repair is several fold. First, the spine is protected after the fetal repair. The spine can no longer be damaged during the pregnancy and after. Second, the leakage of CSF is stopped. We think that this causes the brain to rise back into the skull, allowing the fluid within the brain to drain normally and preventing the development of Hydrocephalus. As with any prenatal surgery, there are risks to both the mother and the baby. Our team at the Fetal Care Institute will discuss all of the risks and benefits of the surgery with you and your family, so you can make the best decision for your baby. The standard care for babies with spina bifida is to repair the defect after birth. The neurosurgeon closes the opening of the spinal cord, and restores the muscle, skin, and tissue to cover it. Unfortunately, postnatal surgery cannot restore any of the function that has been lost during the pregnancy, and the damage from Hydrocephalus, the Chiari malformation, and/or loss of movement are then permanent. How will Myelomeningocele impact my baby after birth? MMC is a disease affecting many parts of the body. There can be a major impact on a baby’s leg and hip movement, depending on the level of the defect. Problems with Hydrocephalus and the Arnold-Chiari malformation need to be followed carefully. Because the spinal cord also affects urine and bowel function, these bodily functions often need to be managed to prevent complications. Optimally, babies need to be followed in a spina bifida clinic, where a team of specialists work together to help determine the best course of treatment. At SSM Health Cardinal Glennon Children’s Hospital, a long established spina bifida clinic is available for follow up care after birth. This is a very specialized clinic in which many doctors of different specialties and nurses are dedicated to the care of these babies.
Spina Bifida
Doctors save the life of an unborn baby who was injured along with her mother in a missile attack in the Syrian city of Aleppo. The video shows a team of emergency medical workers delivering the baby by Cesarean section and then treating the newborn for the shrapnel wounds covering her body and one very large gash in her head. “Medics can be seen frantically reviving the baby, after delivering her by emergency cesarean, as she lies motionless,” the article states. “Eventually the tiny newborn begins to cry and seemingly comes to life as she is given an oxygen mask and rubbed vigorously.” “According to Reuters, the woman also has three other children, all of whom were injured in the attack, but are reported by doctors in the hospital to be in a good condition,” the Daily Mirror article states. The article does not provide the gestational age of the baby before it was delivered. The article said the pregnant woman was hit by a barrel bomb – “crude explosives and shrapnel and dropped from helicopters used by [Syrian] President Bashir al-Assad’s regime." The article notes an estimated 7.6 million Syrians have been displaced by the ongoing civil war and that 320,000, including 11,000 children, have been killed in the conflict. The Daily Mirror also reports that the doctors suggested that the tiny girl be named Amal, which means hope in Arabic. UK Daily Mirror: Incredible footage shows Syrian doctors perform lifesaving caesarean after missile strike leaves shrapnel embedded in unborn baby's face
Sex reassignment surgery for male-to-female involves reshaping the male genitals into a form with the appearance of, and, as far as possible, the function of female genitalia. Prior to any surgeries, patients usually undergo hormone replacement therapy (HRT), and, depending on the age at which HRT begins, facial hair removal. There are associated surgeries patients may elect to, including facial feminization surgery, breast augmentation, and various other procedures
Autonomous Tumor Localization and Extraction: Palpation, Incision, Debridement and Adhesive Closure with the da Vinci Research Kit. This video demonstrates a successful trial of the entire five-step procedure where human input is required only at four points to change tools. We also show failure modes of the current autonomous system and we are working on experiments to characterize the reliability of each step and on incorporating computer vision and new probing algorithms to improve robustness.
Soon enough, a robot will be doing surgeries on you!
An amputation is the removal of an extremity or appendage from the body. Amputations in the upper extremity can occur as a result of trauma, or they can be performed in the treatment of congenital or acquired conditions. Although successful replantation represents a technical triumph to the surgeon, the patient's best interests should direct the treatment of amputations. The goals involved in the treatment of amputations of the upper extremity include the following : Preservation of functional length Durable coverage Preservation of useful sensibility Prevention of symptomatic neuromas Prevention of adjacent joint contractures Early return to work Early prosthetic fitting These goals apply differently to different levels of amputation. Treatment of amputations can be challenging and rewarding. It is imperative that the surgeon treat the patient with the ultimate goal of optimizing function and rehabilitation and not become absorbed in the enthusiasm of the technical challenge of the replantation, which could result in poorer outcome and greater financial cost due to lost wages, hospitalization, and therapy.
http://vene-varicose-rimedi.good-info.co Vene Varicose, Vene Varicose Gambe, Chiva Varici, Laser Per Vene Varicose, Terapia Vene Varicose. Cosa Sono Le Vene Varicose e Quali Sono I Fattori Che Le Determinano? Le vene varicose si verificano quando il sangue non scorre naturalmente attraverso le vene del corpo verso il cuore. Quando ciò accade il sangue si accumula e ristagna nelle vene, di solito nelle vene delle gambe, dando alla pelle un aspetto davvero brutto e sgradevole. Quali Sono Le Vere Cause Delle Vene Varicose? Se si hanno vene varicose probabilmente ci si è già posti questa domanda più di una volta. Le vene varicose possono essere prodotte da vari fattori, quindi analizzeremo i fattori più importanti che possono produrle. 1. Vene Danneggiate. Molte volte le vene non funzionano correttamente, non permettendo al flusso dell sangue di circolare correttamente. Questo a lungo termine causa l'apparizione delle vene varicose. 2. L'Età. Nel corso degli anni molte parti del nostro corpo non funzionano più correttamente e le vene non sono un'eccezione. Gradualmente perdono la loro elasticità e diventano soggette a tutti i tipi di disturbi vascolari. 3. Il Sesso. Le donne sono più propense degli uomini a sviluppare le vene varicose. Le vene varicose compaiono di solito durante la fase di gravidanza, perché in questa fase si produce una maggiore quantità di estrogeni, un ormone che provoca un effetto rilassante nelle vene impedendo la corretta circolazione del sangue in esse. Altri fattori che possono produrre la comparsa delle vene varicose sono la menopausa femminile e le mestruazioni. 4. Stipsi. Le persone che soffrono di stipsi hanno maggiori probabilità di sviluppare vene varicose poiché al tempo dell'evacuazione lo sforzo è maggiore aumenteranno così le forti pressioni sulle vene. Come risultato di questo sforzo, le vene si danneggiano, si stirano e a lungo termine, si produce la comparsa di varici. 5. La Genetica. Se qualcuno nella vostra famiglia ha le vene varicose, è probabile che si svilupperanno in voi a un certo punto della vita. Questo è il motivo per il quale è molto importante sapere la storia della famiglia in modo che si possa essere in grado di identificare il fattore che ha dato origine alle vene varicose e trovare così il corretto trattamento per combatterle. 6. Il Sovrappeso. L’obesità e il sovrappeso possono portare alla comparsa di vene varicose, l'eccesso di peso esercita tensione in molte aree del corpo, includendo le vene. Inoltre, quando una persona è in sovrappeso viene ostacolata la circolazione del sangue, perché si mettono sotto pressione le vene e questo le danneggia. 7. Lesioni Alle Gambe. Le persone che hanno subito traumi a una o entrambe le gambe sono suscettibili allo sviluppo delle vene varicose. Quando si parla di lesioni queste includono: problemi di circolazione nelle gambe, interventi chirurgici, frattura della tibia e perone, ecc. 8. Stile Di Vita Sedentario. La vita sedentaria e le cattive abitudini alimentari possono favorire la comparsa di vene varicose. Una persona che passa seduta lunghi periodi di tempo, magari aggravando la situazione accavallando le gambe, impedisce al sangue di percorrere la sua strada consueta delle gambe al cuore. Il sangue non riesce quindi a lottare contro la forza di gravità e la mancanza di attività nelle gambe causa l'accumulo del sangue nello stesso luogo, portando alla creazione delle vene varicose. 9. Abbigliamento Stretto. Una certa varietà di capi d'abbigliamento e accessori, come ad esempio le scarpe con i tacchi alti, impediscono il flusso corretto del sangue per il corpo e favoriscono l'emergere della varici. Le scarpe chiuse con tacchi alti stringono il piede e impediscono il naturale flusso del sangue verso l'alto, in direzione del cuore. In questo modo il sangue resta all'interno delle vene nelle gambe e a lungo termine possono apparire le vene varicose. Con l'abbigliamento troppo stretto accade la stessa cosa perché impedisce che il sangue scorra correttamente per il corpo. 10. Attività Fisica Ad Alto Impatto. L’Attività fisica ad alto impatto come il sollevamento di pesi è molto popolare perché contribuisce a tonificare in poco tempo i vari gruppi muscolari. Tuttavia il sollevamento di oggetti pesanti, come i pesi, può favorire la comparsa di varici. Tutto questo è ciò che si può imparare in questa guida, Qui scoprirete i migliori metodi naturali per prevenire e contrastare la comparsa di vene varicose! http://vene-varicose-rimedi.good-info.co
Skin Cysts Cysts are noncancerous, closed pockets of tissue that can be filled with fluid, pus, or other material. Cysts are common on the skin and can appear anywhere. They feel like large peas under the surface of the skin. Cysts can develop as a result of infection, clogging of sebaceous glands (oil glands), or around foreign bodies, such as earrings.
Carpal tunnel surgery, also called carpal tunnel release (CTR) and carpal tunnel decompression surgery, is a surgery in which the transverse carpal ligament is divided. It is a treatment for carpal tunnel syndrome and recommended when there is static (constant, not just intermittent) numbness, muscle weakness, or atrophy, and when night-splinting no longer controls intermittent symptoms of pain in the carpal tunnel. In general, milder cases can be controlled for months to years, but severe cases are unrelenting symptomatically and are likely to result in surgical treatment.
A heart transplant, or a cardiac transplant, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease when other medical or surgical treatments have failed.
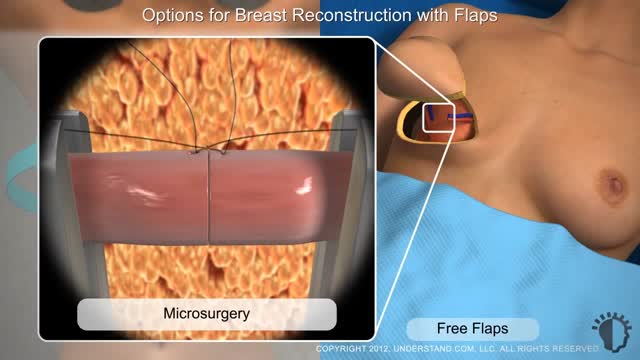
Typically, breast reconstruction takes place during or soon after mastectomy, and in some cases, lumpectomy. Breast reconstruction also can be done many months or even years after mastectomy or lumpectomy. During reconstruction, a plastic surgeon creates a breast shape using an artificial implant (implant reconstruction), a flap of tissue from another place on your body (autologous reconstruction), or both.
Rhinoplasty enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. Rhinoplasty surgery can change: Nose size in relation to facial balance. Nose width at the bridge or in the size and position of the nostrils.
Download Clash of Clans for free for mobile devices. http://supr.cl/ThisArmy
I don't know you, BigBuffetBoy85
But if you think you can humiliate me and take my gold, think again.
Oh, I am coming for you with lots of Barbarians and Dragons. I can't wait to destroy your village, while you beg for mercy, but you will get no mercy. I will have my revenge.