Latest videos
Best facial cosmetic surgeons Best facial plastic surgeon
Best facial cosmetic surgeons B
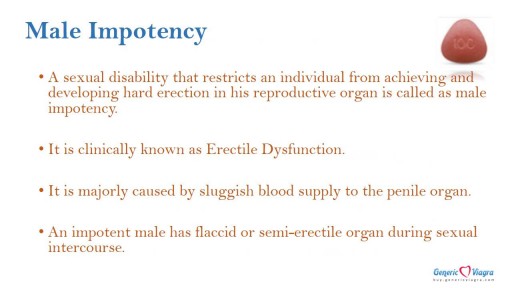
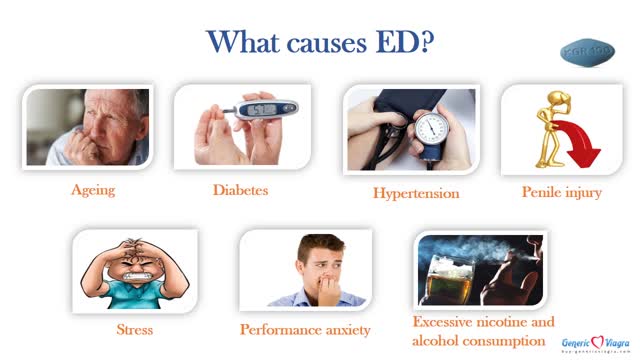
Caverta is an oral medication used to address male impotency related issues. It contains Sildenafil Citrate as the active ingredient. It is available in the form of hard conventional pills. It provides fast-acting results at affordable price. For More info visit : http://www.buy-genericviagra.com/caverta.aspx
There are many exciting milestones that accompany growing older with Down syndrome, old age can also bring unexpected challenges for which adults with Down syndrome, their families and caregivers.
www.homecareassistanceyork.com
• Kamagra Pill is the prescribed form of medicament for treating erectile dysfunction.
• It provides quick, satisfactory results at reasonable rate.
• Sildenafil Citrate is an active ingredient used in its making.
• It delivers lasting effect at the stretch of 4-6 hours.
For More Information visit : http://www.buy-genericviagra.com/kamagra.aspx
stage of pregnancy 2016
Introducing ARTAS in Cocoona Delhi & Dubai by Dr Sanjay Parashar - Hair Transplant Robot
For the elderly, consuming a healthy diet is important to maintaining a strong body and increasing longevity. Many seniors can suffer from vitamin D deficiency due to a lack of exposure to sunlight and by avoiding certain foods. Without enough vitamin D, there are several effects that it can have on both the body and mind for those who are over the age of 50.
http://www.homecareassistancechicago.com/
The video is about taking care of your plaster cast and the after care. What you should do if you have a problem. Your questions answered.
A new treatment option for men suffering from a fatal form of prostate cancer.
Ulcerative Colitis is a painful disease that affects over 100,000 Canadians.
Twin girls joined at the head who share the same brain and so much more
aasd
Want to know how much smart lipo costs? Information on liposuction including liposuction costs, different liposuction techniques, recovery tips and much more.
Laser lipo, or SmartLipo at SafeSculpt Laser Liposuction is the most advanced method for removing unwanted areas of fat from the body.
Dr. Salvador pioneered the development of new liposuction techniques. In 2005, he developed Smartlipo Ultra to provide a safer and more effective treatment for removal of unwanted fat. Smartlipo Ultra was the first liposuction treatment to combine ultrasound for fat removal with laser technology to tighten skin.Dr. Salvador now focuses his cosmetic practice exclusively on SafeSculpt Laser Liposuction. He is recognized internationally as an expert on minimally invasive liposuction and tumescent anesthesia.
Liposuction SmartLipo Ultra Procedure with Dr David Salvador Documentary
Dr. David Salvador provides ultrasonic liposuction for removing fat in West Palm Beach FL.
Dr. Arthur Handal discusses how injectable fillers can be used to restore a patient's youth.
Mommy Makeover Plastic Surgery Boca Raton FL