أحدث مقاطع الفيديو
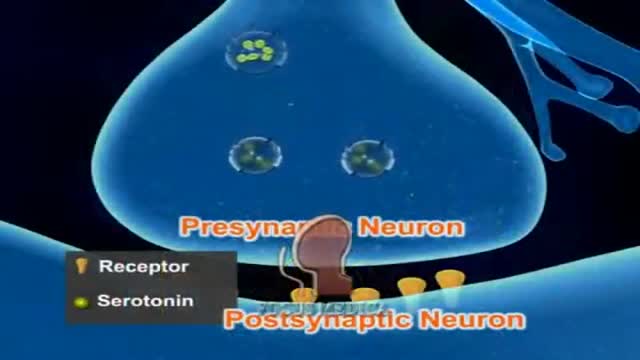
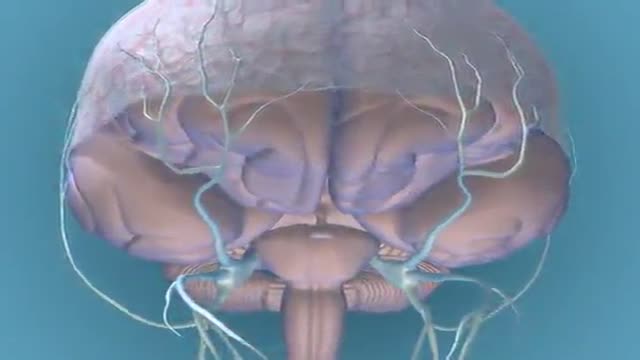
Migraine Pathophysiology 3D Animation
Hiatal Hernia 3D Medical Animation
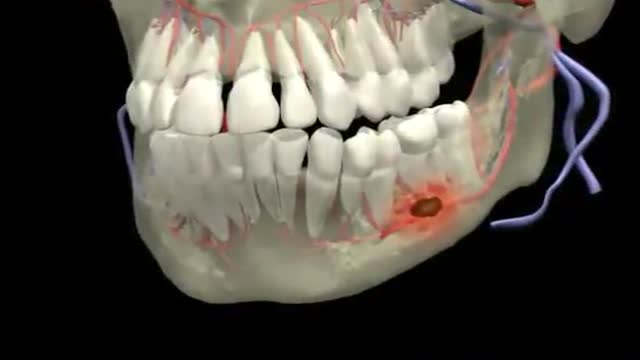
Dental Abscess 3D Animation
Understanding narcolepsy symptoms to improve alertness.
Emergency Medicine Importance If London Was Occupied
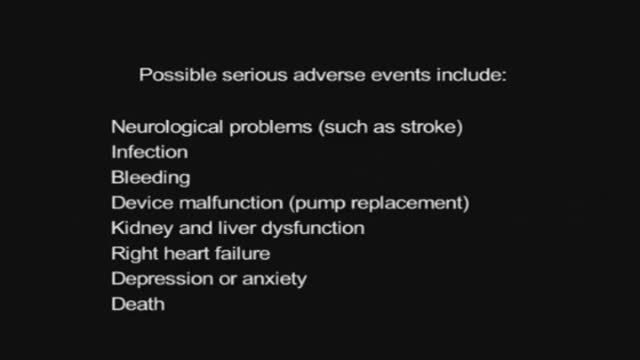
Ventricular Assist Devices
Mechanical Circulatory Support
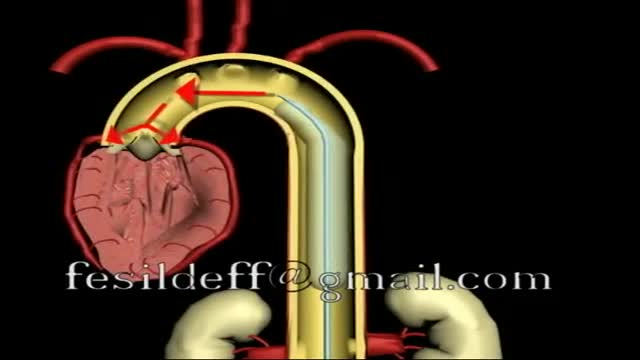
Intra Aortic Balloon Pump
Central Line Placement 3D Animation
Dental Braces and Jaw Reconstruction
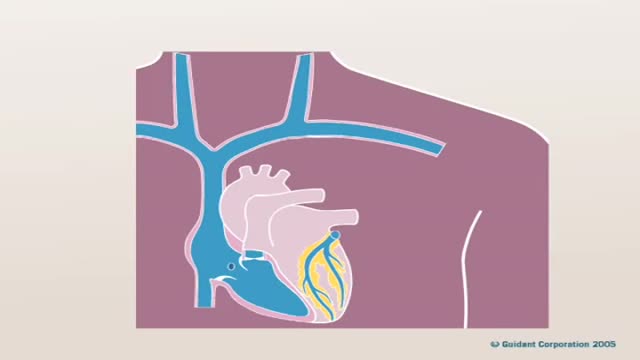
Pacemaker Implantation 3D Animation
Ventricular Assist Device How It Works
New Pacemaker to treat Congestive Heart Failure
Carpal Tunnel Syndrome Self Test
Carpal Tunnel Syndrome 3D Animation
General Neurological Exam Power Reflex Sensory Cranial erves
General Physical Examination
Complete Eye Exam Importance 3D Animation
Dilation and Curettage D and C
Showing 269 out of 270