最新の動画
http://milagroparaelacne.plus101.com
---Como Quitar Acne Cara. Existe una CAUSA PRINCIPAL DEL ACNÉ. Y no siempre un producto para el acné ataca esta causa. Esto significa que, si bien podrías obtener un beneficio de lociones, u otros productos o terapias, nunca curarás tu acné con ellos.
Es un poco como tener un techo con goteras y "solucionarlo" poniendo recipientes para recoger el agua de lluvia que cae del techo. Para solucionar adecuadamente el techo con goteras, se debe corregir la causa de raíz, que es el agujero en el techo.
Entonces... ¿Cuál Es La Principal
Causa Del ACNE?
La causa del acné es un DESEQUILIBRIO HORMONAL. Esto es algo que las empresas del acné nunca te dirán...
... Sin embargo, saber la causa del acné es una cosa. Descubrir la forma de eliminar eficazmente esta causa es otra cosa...
Como, Quitar, Acne, Cara, manchas de acne, quitar el acne, cicatrices de acne, como quitar granos, como quitar espinillas, cicatrices de acne, eliminar el acne, como eliminar barros, eliminar los barros,
Skin transplantation in the arm
This video goes through a case study of a 40 year old patient getting breast reduction surgery in NYC by board certified plastic surgeon Carlin Vickery of 5th Avenue Surgery located in New York, NY. For more information on this procedure please call our office at (212) 288-9800. This content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
http://crohnsulcerativecolitis.plus101.com/
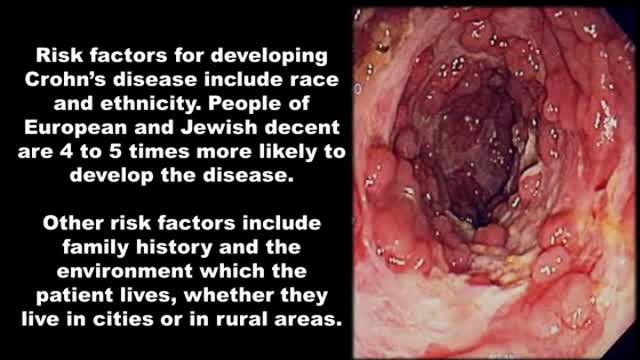
----Crohn's Disease Symptoms Pain. Are you suffering from diarrhea that sometimes leaves you feeling that you've completely emptied your intestine from eveything you've eaten that week?
Have you seen bright red blood traces in your stool or on the toilet paper at least once?
Do you sometimes have abdominal cramps after your meals?
Do you at times feel so nauseous that food doesn't have any appeal to you?
Have you had at least one onset of unexplained low grade fever?
Do you joints sometimes feel itchy, sore or painful?
Did you ever notice red spots or blisters on your arms or legs?
Did you ever experience episodes of itchy and even painfull pink eye (conjuctivitis)?
Have you lost weight?
Do you have episodes of overwhelming fatigue?
Do you experience increased frequency of bowel movement?
Did you ever get up during the night to defecate?
Crohn's, Disease, Symptoms, Pain, symptoms of crohns, chrons disease symptoms , ulcerative colitis symptoms, symptoms of colitis, United States, United Kingdom, Canada, ulcerative colitis diet, ulcerative colitis treatment, irritable bowel symptoms
Improve blood sugar control in adults with type 2 diabetes through new advancements
Rheumatoid Arthritis,physiology,pathology,clinincal features,manifestations and treatment
Rheumatoid Arthritis Onset and Symptoms and general information
Temporal Arteritis: what is it? how to treat it? follow up?
Multiple strains put your children and teens at risk of meningococcal meningitis. How-to ensure they are fully protected.
急性坏疽性阑尾炎的手术治疗
腹腔镜十二指肠穿孔修补术2
腹腔镜十二指肠球部溃疡修补术
A simple video showing the small tips to be followed by patients which a clinician should provide. The video is simple, easy to understand and can be provided to the patient for their reference.
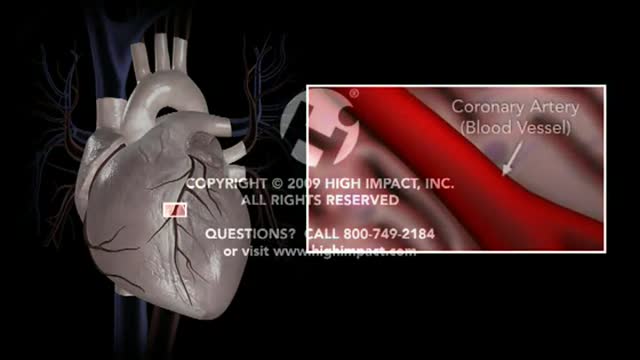
Coronary Artery Atherosclerosis
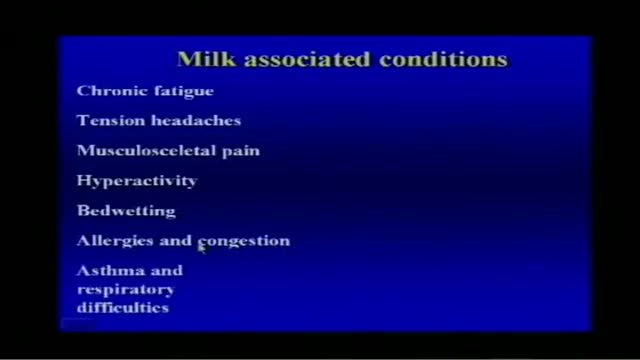
Milk Associated Diseases Information
Providing information on the Atherosclerosis and its complex biological process: it is the idea of this medical video dedicated to the prevention of the cardiovascular risks of diseases.
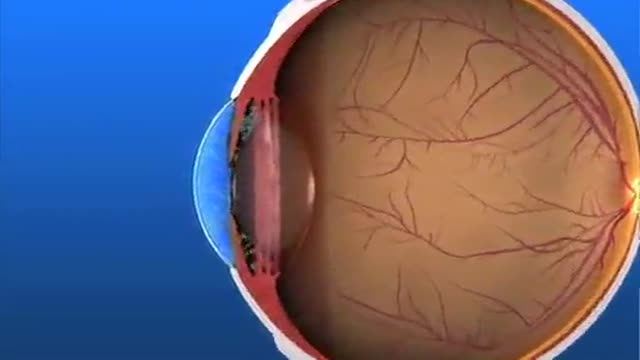
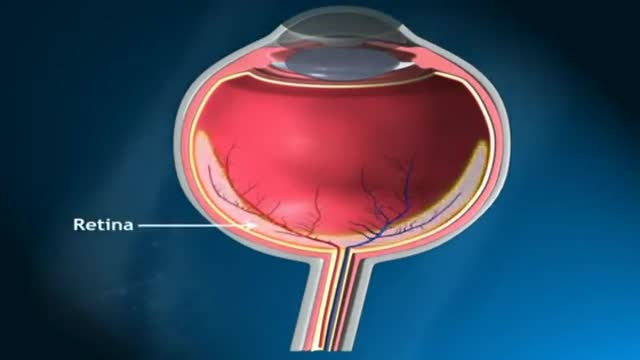
Glaucoma Pathogenesis Simplified
ADA IS ABSOLUTE CLUELESS AND IGNORANT CONCERNING MOST INNOVATIVE DENTAL IMPLANT METHOD
Glaucoma is called the silent thief of sight. It does not have symptoms during the early stages of the diseases and can make a patient blind over several years