Últimos vídeos
Heart Valves
Gastrointestinal GI Drug Delivery
Imperforate Hymen
Lower Face Lift Awake Plastic Surgery
Pelvic lymphadenectomy
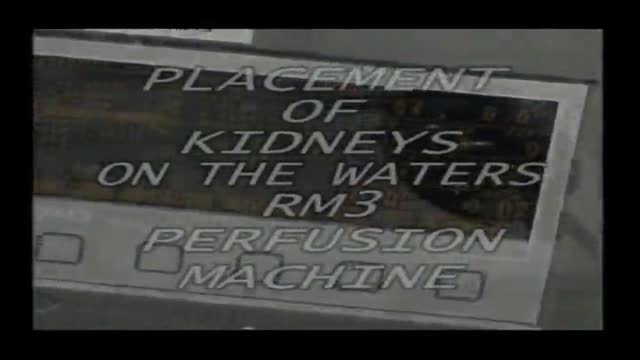
Dissection and Cannulation of Cadaveric Kidney
Traumatic Urinary Bladder Groin Injury
New Phacoemulsification Horizontal Chopping
Eye Surgery penetrating Keratoplasty
Eye Cyst Removal By Vitrectomy
Eye Surgery Trabeculectomy
Eye Surgery C Lasik
Abnormal Eye Lid Positions Ptosis
Gastric Lavage Video
Eye Phacoemulsification
Pterygium Excision with Auto Conjunctival Graft
Ocular Movement Examination
Keratectomy with Amniotic Membrane Graft Eye
Eye Lid Tarsal Fracture Surgery
Eye Lid Partial Tarsectomy Surgery
Showing 275 out of 276